Coverage of Llin Among Expectant Mothers in Nwangele, Imo State, Nigeria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nigeria's Constitution of 1999
PDF generated: 26 Aug 2021, 16:42 constituteproject.org Nigeria's Constitution of 1999 This complete constitution has been generated from excerpts of texts from the repository of the Comparative Constitutions Project, and distributed on constituteproject.org. constituteproject.org PDF generated: 26 Aug 2021, 16:42 Table of contents Preamble . 5 Chapter I: General Provisions . 5 Part I: Federal Republic of Nigeria . 5 Part II: Powers of the Federal Republic of Nigeria . 6 Chapter II: Fundamental Objectives and Directive Principles of State Policy . 13 Chapter III: Citizenship . 17 Chapter IV: Fundamental Rights . 20 Chapter V: The Legislature . 28 Part I: National Assembly . 28 A. Composition and Staff of National Assembly . 28 B. Procedure for Summoning and Dissolution of National Assembly . 29 C. Qualifications for Membership of National Assembly and Right of Attendance . 32 D. Elections to National Assembly . 35 E. Powers and Control over Public Funds . 36 Part II: House of Assembly of a State . 40 A. Composition and Staff of House of Assembly . 40 B. Procedure for Summoning and Dissolution of House of Assembly . 41 C. Qualification for Membership of House of Assembly and Right of Attendance . 43 D. Elections to a House of Assembly . 45 E. Powers and Control over Public Funds . 47 Chapter VI: The Executive . 50 Part I: Federal Executive . 50 A. The President of the Federation . 50 B. Establishment of Certain Federal Executive Bodies . 58 C. Public Revenue . 61 D. The Public Service of the Federation . 63 Part II: State Executive . 65 A. Governor of a State . 65 B. Establishment of Certain State Executive Bodies . -

Application of Index Models for Assessing Freshwater Microplastics Pollution
Available online at www.worldnewsnaturalsciences.com WNOFNS 38 (2021) 37-48 EISSN 2543-5426 Application of Index Models for Assessing Freshwater Microplastics Pollution Christian Ebere Enyoh1,*, Andrew Wirnkor Verla1, Md. Refat Jahan Rakib2 1Group Research in Analytical Chemistry, Environment and Climate change (GRACE&CC), Department of Chemistry, Faculty of Science, Imo State University, Owerri, Nigeria 2Department of Fisheries and Marine Science, Faculty of Science, Noakhali Science and Technology University, Noakhali, Bangladesh *E-mail address: [email protected] ABSTRACT Due to the differences in reporting units and methodology on microplastics (MP) studies, there has been some difficulty in comparing results across studies. In this study, we presented index models that can be address this issue. Index models for pollution and health risks assessment was applied to MP data obtained from rivers in Nwangele L.G.A. Models such as microplastics contamination factor (MPCF), microplastics pollution load index (MPPLI), Microplastics polymer risk indices (Hi) and pollution risk index (MPR) for pollution and contamination assessment. Health risk models such estimated daily intake (EDI) and microplastic carcinogenic risks (MPCR) through oral and dermal pathway were also presented and applied. Results showed that there is no direct correlation of MP abundance with MPR. However, Hi correlated but with MPR. Increased MPs pollution risks and levels were extensively subject to the presence of harmful MPs polymers, just as the high MPs pollution loads index (MPPLI). The index models enabled easy comparison of MP pollution of the different rivers and provided concise information on the status of MPs in the rivers. Keywords: Carcinogenic, Estimated daily intake, Health risks, Modeling, Plastic pollution 1. -

Statistical Prediction of Gully Erosion Development on the Coastal Plain Sands of the South Eastern Nigeria
Nigerian Journal of Technology, Vol. 24, No. 2, September 2005 Nwakwasi and Tee 59 STATISTICAL PREDICTION OF GULLY EROSION DEVELOPMENT ON THE COASTAL PLAIN SANDS OF THE SOUTH EASTERN NIGERIA NWAKWASI, N.L., and TEE, D.P. Department of Civil Engineering, Federal University of Technology, Owerri, Nigeria ABSTRACT A statistical model for predicting gully initiation was developed using variables from 20 randomly selected sites. The random samples gave 10 gully sites and 10 non-gully sites. In all, 12 variables were identified but using students t-tests approach, only four variables contributed to gully development. These four variables include Maximum slope, Maximum slope length, Microrelief amplitude and percentage coarse sand. The four variables were combined through factor analysis and statistical manipulations to form Linear Discriminant Function (LDF). Three functions were obtained by combining the variables in three different ways. An application of the three functions to the field situation identified function 1,1 as a very comfortable prediction. When Yl was used to classify the various sites using the variables obtained from the field, a 25% wrong classification was obtained. This value was quite low when compared with the other two functions whose wrong classification ranged from 35% and above. It was observed from the study that when Yl is less than 30, it indicated little or no gully erosion threat. INTRODUCTION spatial distribution of rainfall as induced gully Today, in our country Nigeria, erosion menace formation in most of our towns and express the has become all object of discussion and a major need to adopt good planning and policy ecological problem facing the nation. -

2456-8643 Assessment of Quality Of
International Journal of Agriculture, Environment and Bioresearch Vol. 4, No. 01; 2019 ISSN: 2456-8643 ASSESSMENT OF QUALITY OF TANKER WATER DISTRIBUTED IN ATTA, AMARAKU AND ABAJAH COMMUNITIES IN IMO STATE 1Uzoechi A.U; 2Okoro P. E 3 and Agwunobi K. E 1Department of Microbiology, Federal University of Technology Owerri 2Department of Pharmacology, College of Medicine, Imo State University Owerri 3 Department of Medical Laboratory Science, College of Health and Management Sciences Amaigbo Nwangele ABSTRACT Microbiological and chemical quality of drinking water primarily results from water origin and type of applied water treatment. many infectious agents can be transmitted to humans through drinking water causing waterborne diseases, regular monitoring of drinking water quality in water supply systems is needed. This study investigates the microbiological quality of tanker water supplied to selected different local communities(Atta, Amaraku, Abajah) in Imo state during summer, Rainy and winter season for the period of the year June, 2017 to June, 2018. Since increased concentrations of some chemical compounds in water can influence on appearance and growth of microbiological populations, in this study relevant physicochemical parameters were also measured and correlated with obtained values of analyzed microbiological parameters. Physico-chemical parameters studied includes determination of the pH, temperature, turbidity, hardness, alkalinity, chlorides, fluorides nitrate, iron, silica levels in the water samples. The results obtained indicated that the chemical quality of the water samples under study falls within the standards recommended by World Health Organization. However, more potentially dangerous discovery was the level of Coliform contamination which exceeds the WHO standards. Other microorganisms detected were E. -

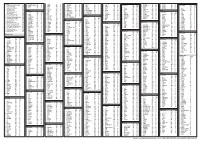
List of Community Banks Converted to Microfinance Banks As at 31St
CENTRAL BANK OF NIGERIA IMPORTANT NOTICE LIST OF COMMUNITY BANKS THAT HAVE SUCESSFULLY CONVERTED TO MICROFINANCE BANKS AS AT DECEMBER 31, 2007 Following the expiration of December 31, 2007 deadline for all existing community banks to re-capitalize to a minimum of N20 million shareholders’ fund, unimpaired by losses, and consequently convert to microfinance banks (MFB), it is imperative to publish the outcome of the conversion exercise for the guidance of the general public. Accordingly, the attached list represents 607 erstwhile community banks that have successfully converted to microfinance banks with either final licence or provisional approval. This list does not, however, include new investors that have been granted Final Licences or Approvals-In- Principle to operate as microfinance banks since the launch of Microfinance Policy on December 15, 2005. The Central Bank of Nigeria (CBN) hereby states categorically that only the community banks on this list that have successfully converted to microfinance banks shall continue to be supervised by the CBN. Members of the public are hereby advised not to transact business with any community bank which is not on the list of these successfully converted microfinance banks. Any member of the public, who transacts business with any community bank that failed to convert to MFB does so at his/her own risk. Members of the public are also to note that the operating licences of community banks that failed to re-capitalize and consequently do not appear on this list, have automatically been revoked pursuant to Section 12 of BOFIA, 1991 (as amended). For the avoidance of the doubt, new applications either as a Unit or State Microfinance Banks from potential investors or promoters shall continue to be received and processed for licensing by the Central Bank of Nigeria. -

Water Quality Assessment of Nwangele River in Imo State, Nigeria
Journal of Ecobiotechnology 2019, 11: 1-5 doi: 10.25081/jebt.2019.v11.3866 http://updatepublishing.com/journal/index.php/jebt Research Article Water quality assessment of Nwangele river in Imo State, Nigeria Anudike Joseph1*, Duru Majesty2, Uhegbu Friday1 ISSN: 2077-0464 1Department of Biochemistry, Abia State University, Uturu, Nigeria, 2Department of Chemical Sciences (Biochemistry Unit), Rhema University, Aba, Nigeria. ABSTRACT Water quality assessment of Nwangele river was undertaken using standard methods. Water samples were drawn from upstream, midstream and downstream of the river and assessed for quality. Results obtained for physicochemical characteristics showed pH (4.83±.0.01-5.00±0.31), total solid (200.00±2.40-613.19±1.10 mg/L), and total suspended solid (49.98±0.11-399.04±2.09 mg/L). Heavy metals found in the river water were iron (0.132±0.01- 0.144±0.02 mg/L), zinc (0.034±0.02- 0.044±0.02 mg/L), mercury (0.004±0.001- 0.011±0.00 mg/L), lead (0.008±0.00- 0.016±0.00 mg/L) Received: November 12, 2018 and cadmium (0.03±0.01- 0.011±0.00 mg/L). Microbiological studies on the river revealed the presence of Klebsieilla Accepted: February 21, 2019 sp., Vibro sp., Pseudomonas sp., Proteus sp., Escherichia sp., Staphylococcus sp., Shigella sp., Bacillus sp., Serratia sp., Published: February 28, 2019 Citrobacter sp., and Enterobacter sp as bacterial isolates with high total heterotrophic bacteria count (THBC), total coliform count (TCC), Salmonella-shigella count (SSC), and total viable count (TVC). -

Environmental-And-Social-Impact-Assessment-For-The-Rehabilitation-And-Construction-Of
Public Disclosure Authorized FEDERAL REPUPLIC OF NIGERIA IMO STATE RURAL ACCESS AND MOBILITY PROJECT (RAMP-2) ENVIRONMENTAL AND SOCIAL IMPACT ASSESSMENT (ESIA) Public Disclosure Authorized FOR Public Disclosure Authorized THE REHABILITATION/ CONSTRUCTION OF 380.1KM OF RURAL ROADS IN IMO STATE August 2019 Public Disclosure Authorized Final ESIA for the Rehabilitation of 88 Rural Roads in Imo State under RAMP-2 TABLE OF CONTENTS TABLE OF CONTENTS ..................................................................................................................... ii LIST OF TABLES .............................................................................................................................. vii LIST OF FIGURES ........................................................................................................................... viii LIST OF PLATES ............................................................................................................................. viii LIST OF ACRONYMS AND ABBREVIATIONS ........................................................................... ix EXECUTIVE SUMMARY .................................................................................................................. x CHAPTER ONE: INTRODUCTION ................................................................................................. 1 1.1 Background................................................................................................................................ 1 1.2 Project Development Objective -

LGA Aboh Mbaise Ahiazu Mbaise Ehime Mbano Ezinihitte Mbaise Ideato North Ideato South Ihitte Uboma Ikeduru Isiala Mbano Isu Mbai
LGA Aboh Mbaise Ahiazu Mbaise Ehime Mbano Ezinihitte Mbaise Ideato North Ideato South Ihitte Uboma Ikeduru Isiala Mbano Isu Mbaitoli Ngor Okpala Njaba Nkwerre Nwangele Obowo Oguta Ohaji/Egbema Okigwe Onuimo Orlu Orsu Oru East Oru West Owerri Municipal Owerri North Owerri West PVC PICKUP ADDRESS Inside The Local Govt. Secretariat Behind The Local Govt. Stadium Along Umuezela Isiala Mbano Road, Near Aba Branch Inside The Lga Secretariat Inside The Lga Secretariat Behind The Lga Office (SHARES A Common Fence With The Lga Office Along Isinweke Express Road Opposite The Lga Office Along Umuelemai/Umuezeala Road Along The Lga Office Road, Umundugba Along Awo-Mbieri Road, Nwaorieubi Inside The Lga Office Inside The Lga Office Along Nkwerre Orlu Road, Near The Lga Office Situated Within The Old Site Of The Lga Office Along Umuahia-Obowo Road, Opp. Obowo Police Station At Nkwo-Oguta Inside The Lga Secretariat Office Inside The Lga Complex Inside The Lga Office Along Ezerioha Road Along Police Station Road Awo-Idemili Insde The Lga Office Along Onitsha-Owerri Road, Mgbidi (AFTER Magistrate Court-Sharing Same Fence Opposite The State Post Office, Along Douglas Road, Within The Lga Secretariat After The Lga H/Q (ORIE Uratta) Within The Lga Office Along Onitsha-Owerri Road, Mgbidi (AFTER Magistrate Court-Sharing Same Fence Opposite The State Post Office, Along Douglas Road, Within The Lga Secretariat. -

Hydrogeophysical Evaluation of Aquifer of the Lower Orashi River
International Journal of Advanced Academic Research | Sciences, Technology and Engineering | ISSN: 2488-9849 Vol. 5, Issue 8 (August 2019) HYDROGEOPHYSICAL EVALUATION OF AQUIFER UNITS AROUND THE LOWER ORASHI RIVER AREA, SOUTHEASTERN NIGERIA 1MBAGWU E.C., 1IBENEME S.I., 1OKEREKE C.N AND 1EZEBUNANWA A.C. 1Department of Geology, Federal University of Technology Owerri, Imo State, Nigeria. Corresponding Authors: [email protected], [email protected] ABSTRACT Hydrogeophysical characteristics of the aquifers of the Lower Orashi River Area, Southeastern Nigeria was done using VES to delineate the aquifers and evaluate their geometric characteristics. The study area is underlain by the Ameki, Ogwashi and Benin Formations. The unconsolidated nature of the Formations and their high susceptibility to contamination have made this study imperative, as it would assist water resource planners and developers in the area to understand the best way to plan and site boreholes in the area. Eighty eight (88) Schlumberger Vertical Electrical Soundings (VES) were carried out in various parts of the study area with a maximum electrode separation (AB/2) of 350 m. The VES data were processed using a combination of curve matching techniques and computer iterative modeling. The study revealed seven to ten geo-electric layers with varying lithologies majorly sand units and a multiple aquifer system ranging from confined to unconfined aquifers. The results indicate that aquifer thickness ranges from 20m to about 227m. A quantitative interpretation of the curves -
States and Lcdas Codes.Cdr
PFA CODES 28 UKANEFUN KPK AK 6 CHIBOK CBK BO 8 ETSAKO-EAST AGD ED 20 ONUIMO KWE IM 32 RIMIN-GADO RMG KN KWARA 9 IJEBU-NORTH JGB OG 30 OYO-EAST YYY OY YOBE 1 Stanbic IBTC Pension Managers Limited 0021 29 URU OFFONG ORUKO UFG AK 7 DAMBOA DAM BO 9 ETSAKO-WEST AUC ED 21 ORLU RLU IM 33 ROGO RGG KN S/N LGA NAME LGA STATE 10 IJEBU-NORTH-EAST JNE OG 31 SAKI-EAST GMD OY S/N LGA NAME LGA STATE 2 Premium Pension Limited 0022 30 URUAN DUU AK 8 DIKWA DKW BO 10 IGUEBEN GUE ED 22 ORSU AWT IM 34 SHANONO SNN KN CODE CODE 11 IJEBU-ODE JBD OG 32 SAKI-WEST SHK OY CODE CODE 3 Leadway Pensure PFA Limited 0023 31 UYO UYY AK 9 GUBIO GUB BO 11 IKPOBA-OKHA DGE ED 23 ORU-EAST MMA IM 35 SUMAILA SML KN 1 ASA AFN KW 12 IKENNE KNN OG 33 SURULERE RSD OY 1 BADE GSH YB 4 Sigma Pensions Limited 0024 10 GUZAMALA GZM BO 12 OREDO BEN ED 24 ORU-WEST NGB IM 36 TAKAI TAK KN 2 BARUTEN KSB KW 13 IMEKO-AFON MEK OG 2 BOSARI DPH YB 5 Pensions Alliance Limited 0025 ANAMBRA 11 GWOZA GZA BO 13 ORHIONMWON ABD ED 25 OWERRI-MUNICIPAL WER IM 37 TARAUNI TRN KN 3 EDU LAF KW 14 IPOKIA PKA OG PLATEAU 3 DAMATURU DTR YB 6 ARM Pension Managers Limited 0026 S/N LGA NAME LGA STATE 12 HAWUL HWL BO 14 OVIA-NORTH-EAST AKA ED 26 26 OWERRI-NORTH RRT IM 38 TOFA TEA KN 4 EKITI ARP KW 15 OBAFEMI OWODE WDE OG S/N LGA NAME LGA STATE 4 FIKA FKA YB 7 Trustfund Pensions Plc 0028 CODE CODE 13 JERE JRE BO 15 OVIA-SOUTH-WEST GBZ ED 27 27 OWERRI-WEST UMG IM 39 TSANYAWA TYW KN 5 IFELODUN SHA KW 16 ODEDAH DED OG CODE CODE 5 FUNE FUN YB 8 First Guarantee Pension Limited 0029 1 AGUATA AGU AN 14 KAGA KGG BO 16 OWAN-EAST -

Bank Directory Page 1 S/N Name Staff Staff Position Address Website 1
Bank Directory S/N Name Staff Staff Position Address Website 1 Central Bank Of Nigeria Mr. Godwin Emefiele, Governor Central Business District, Garki, www.cbn.gov.ng HCIB Abuja 2 Nigeria Deposit Insurance Alhaji Umaru Ibrahim, MNI, Managing Plot 447/448, Constitution http://ndic.org.ng/ Corporation FCIB Director/Chief Avenue, Central Business Executive District, Garki, Abuja 3 Access Bank PLC Mr. Herbert Wigwe, FCA Group Managing 1665, Oyin Jolayemi Street, www.accessbankplc.com Director/Chief Victoria Island, Lagos Executive 4 Diamond Bank PLC Mr. Uzoma Dozie, FCIB Group Managing Plot 1261 Adeola Hopewell www.diamondbank.com Director/Chief Street, Victoria Island, Lagos, Executive Lagos , 5 Ecobank Nigeria PLC Mr. Patrick Akinwuntan Group Managing Plot 21, Ahmadu Bello Way, www.ecobank.com Director/Chief Victoria Island, Lagos Executive 6 First City Monument Bank PLC Mr. Adam Nuru Managing Primrose Towers, 6-10 www.fcmb.com Director/Chief Floors ,17A, Tinubu Square, Executive Officer Lagos 7 Fidelity Bank PLC Nnamdi J. Okonkwo Managing 2, Kofo Abayomi Street, Victoria www.fidelitybankplc.com Director/Chief Island, Lagos Executive 8 First Bank Of Nigeria Limited Dr. Adesola Kazeem Group Managing 35, Marina, Lagos www.firstbanknigeria.com Adeduntan, FCA Director/Chief Executive Officer 9 Guaranty Trust Bank PLC (GT Bank) Mr. Olusegun Agbaje, Managing Plot 1669, Oyin Jolayemi Street, www.gtbplc.com HCIB Director/Chief Victoria Island, Lagos Executive 10 Citibank Nigeria Limited Mr. Akin Dawodu MD/CEO Charles S. Sankey House,27 www.citigroup.com Kofo Abayomi Street, Victoria Island, Lagos 11 Keystone Bank LTD Mr. Hafiz Olalade Bakare Managing 1, Keystone Bank Crescent, www.keystonebankng.com Director/Chief Victoria Island Executive Page 1 Bank Directory 12 Polaris Bank PLC Mr. -

Anambra Imo River Basin Development
FEDERAL MINISTRY OF WATER RESOURCES ANAMBRA IMO RIVER BASIN DEVELOPMENT AUTHORITY KM 10, OWERRI-ABA ROAD, OWERRI REQUEST FOR EXPRESSION OF INTEREST/INVITATION TO TENDER FOR PROJECTS UNDER THE 2021 APPROPRIATION 1. INTRODUCTION The Anambra Imo River Basin Development Authority, a Parastatal under the Federal Ministry of Water Resources wishes to notify the General Public of her intended procurement under its 2021 Appropriation Act. To achieve this, the Authority hereby invites Technical and Financial bids from interested, qualified, and competent Companies/Firms, including Joint Ventures (JVs) for the execution of the projects listed below: 2. SCOPE OF WORK The projects earmarked for execution/supervision are categorized as follows: CATEGORY A WORKS Gully Erosion Works In Enuagu, Enugwu-Ukwu Together with Estimated 5km Road Leading to The Erosion Site Lot W(A1) which Begins from Enuagu to Umuakwu Lot W(A2a) Erosion Control Projects in Njikoka Anambra State Lot W(A2b) Erosion Control Projects in Idemili Lgas, Anambra State Erosion Control Works and Construction of Side Drains at Government Secondary School Ibagwe Girls, Igbo-Eze Lot W(A3) South Lot W(A4) Erosion Control Work On Obinagu/Dike Street Erosion Site, Anambra State Lot W(A5) Umuogu Road Spur Okija Erosion Control Works Lot W(A6) Construction of Roads in Odoakpu and American Quarters in Onitsha North And South Lga, Anambra State Erosion Control Works At T-Junction To Ezinne-Agu/ Eziowelle Road, Mgbuke Village, Umunnachi Dunukofia Lga, Lot W(A7) Anambra Central Senatorial District