Update on Novel Shock Treatments and Approach to Utilization
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

IV-23 N. Hydroxocobalamin (Cyanokit®)
N. Hydroxocobalamin (Cyanokit®) I. Classification •Cyanide antidote II. Actions •Binds cyanide ions with more affinity than hemoglobin molecule •Cyanide ion and hydroxocobalamin form cyanocobalamin (Vitamin B12) which is then excreted in the urine. III. Indications •Known or suspected cyanide poisoning - patients at high risk (industrial accidents, fire victims with smoke inhalation, known overdose, etc) with one more more of the following symptoms: - Altered mental status, confusion, seizures, coma - Headache - Chest pain or tightness - Shortness of breath, bradypnea, tachypnea - Hypertension (early), hypotension (late), cardiovascular collapse - Nausea, vomiting - Cardiac arrest - Mydriasis (dilated pupils) IV. Contraindications •Known allergic reaction to hydroxocobalamin or cyanocobalamin V. Adverse effects A. Cardiovascular •Ventricular extrasystoles •Tachycardia •Transient hypertension B. Neurological •Memory impairment •Dizziness •Restlessness C. Respiratory •Dyspnea •Dry Throat •Throat tightness D. Gastrointestinal •Abdominal discomfort •Dysphagia •Vomiting, diarrhea •Hematochezia E. General •Allergic reaction, pruritis, anaphylaxis •Hot flush SUBJECT : PATIENT CARE GUIDELINES AND STANDING ORDERS FOR BLS AND ALS UNITS REFERENCE NO. III-01 PUBLICATION : 1/11/21 IV-23 VI. Administration A. Do not administer hydroxocobalamin through the same IV site/set as the following medications: dopamine, fentanyl, dobutamine, diazepam, nitroglycerin, pentobarbital, propofol, thiopental, sodium thiosulfate, sodium nitrite and ascorbic acid. You must start a second IV to administer hydroxocobalamin in patient’s receiving these medications. B. Adult: •5 grams IV/IO over 15 minutes (Stocked as single 5gm bottle, or two 2.5 gm bottles) -Single 5 gm Bottle - Reconstituted with 200 ml Normal Saline. -Two 2.5 gm Bottles, give over 7.5 minutes each. - Each vial reconstituted with 100 ml Normal Saline. C. Pediatric •100 mg/kg IV/IO of hydroxocobalamin (reconstituted with Normal Saline the same as adults) over 15 minutes. -

Guidelines on Food Fortification with Micronutrients
GUIDELINES ON FOOD FORTIFICATION FORTIFICATION FOOD ON GUIDELINES Interest in micronutrient malnutrition has increased greatly over the last few MICRONUTRIENTS WITH years. One of the main reasons is the realization that micronutrient malnutrition contributes substantially to the global burden of disease. Furthermore, although micronutrient malnutrition is more frequent and severe in the developing world and among disadvantaged populations, it also represents a public health problem in some industrialized countries. Measures to correct micronutrient deficiencies aim at ensuring consumption of a balanced diet that is adequate in every nutrient. Unfortunately, this is far from being achieved everywhere since it requires universal access to adequate food and appropriate dietary habits. Food fortification has the dual advantage of being able to deliver nutrients to large segments of the population without requiring radical changes in food consumption patterns. Drawing on several recent high quality publications and programme experience on the subject, information on food fortification has been critically analysed and then translated into scientifically sound guidelines for application in the field. The main purpose of these guidelines is to assist countries in the design and implementation of appropriate food fortification programmes. They are intended to be a resource for governments and agencies that are currently implementing or considering food fortification, and a source of information for scientists, technologists and the food industry. The guidelines are written from a nutrition and public health perspective, to provide practical guidance on how food fortification should be implemented, monitored and evaluated. They are primarily intended for nutrition-related public health programme managers, but should also be useful to all those working to control micronutrient malnutrition, including the food industry. -

Validation of Hplc Method for Determination of Thiamine Hydrochloride, Riboflavin, Nicotinamide, and Pyridoxine Hydrochl0ride in Syrup Preparation
Canadian Journal on Scientific and Industrial Research Vol. 2 No. 7, August 20ll VALIDATION OF HPLC METHOD FOR DETERMINATION OF THIAMINE HYDROCHLORIDE, RIBOFLAVIN, NICOTINAMIDE, AND PYRIDOXINE HYDROCHL0RIDE IN SYRUP PREPARATION NOVI YANTIH*, DIAH WIDOWATI, WARTINI, TIWI ARYANI Faculty of Pharmacy, University of Pancasila Email: novi_yantih @ yahoo.com Faculty of Pharmacy, University of Pancasila, Srengseng Sawah, Jagakarsa, 12640 South Jakarta, Indonesia ABSTRACT Multivitamin syrup containing various substances of varying characteristics may have a problem in quantitative analysis. This research has developed and validated of HPLC method for determination of four vitamin components, that is thiamine hydrochloride, riboflavin, nicotinamide, and pyridoxine hydrochloride in syrup multivitamin-mineral. The chromatographic separation was achieved by using a C18 column with dimension of 3.9x300mm and particle size of l0µm. A mixture of methanol - l% acetic acid by using 7mM 1-hexane sulphonic acid sodium salt (20:80) as mobile phase with flow rate of 1 mL/min. The effluent was monitored at 280 nm. Effective separation and quantification was achieved in less than 20 min. That method was simple, accurate, precise, and could be successfully applied for the analysis of thiamine hydrochloride, riboflavin, nicotinamide, and pyridoxine hydrochloride syrup multivitamin- mineral. Keywords: Thiamine hydrochloride, riboflavin, nicotinamide, pyridoxine hydrochloride, syrup, HPLC. 269 270 INTRODUCTION Syrup multivitamin and mineral preparations containing various substances of varying characteristics may have many problems in quantitative analysis. High performance liquid chromatography (HPLC) due to its high capacity in separating a mixture of substances was applicable in determining each component in multivitamin preparations simultaneously. Several investigator have reported the used of HPLC methods for the determination of water-soluble vitamins, such as thiamine hydrochloride, riboflavin, nicotinarnide, and pyridoxine hydrochloride in pharmaceuticals preparations [l,2,3]. -

Cyanocobalamin-A Case for Withdrawal
686 Journal of the Royal Society of Medicine Volume 85 November 1992 Cyanocobalamin- a case for withdrawal: discussion paper A G Freeman MD FRCP Meadow Rise, 3 Lakeside, Swindon SN3 IQE Keywords: anaemia, pernicious; optic neuropathies; chronic cyanide intoxication; hydroxocobalamin; cyanocobalamin It seems evident that controversy still surrounds the reduced ability to detoxify the cyanide in the tobacco- treatment of pernicious anaemia and other vitamin smoke to which they are exposed'0. B12 deficiency disorders. The long quest for the 'anti- Patients with tobacco amblyopia who have normal pernicious anaemia factor' in the liver seemed to serum vitamin B12 levels need not continue therapy have ended in 1948 when pure cyanocobalamin was with intramuscular hydroxocobalamin once their isolated. This was found to be very active thera- visual acuity and visual fields have returned to peutically when given by intramuscular injection and normal providing they abstain from further smoking. was non-toxic in extremely high doses'. However, those patients who have low serum vitamin Lederle, in a recent commentary2, advocates that B12 levels or evidence of -defective vitamin B12 patients with pernicious anaemia should now be absorption will need to continue-indefinitely with treated with oral cyanocobalamin. He is not without hydroxocobalamin irrespective of their smoking support in that 40% of patients with pernicious habits as will all patients with pernicious anaemia anaemia in Sweden are being similarly treated3. and other vitamin B12 deficiency disorders who are He further states that such!- treatment is cheap at risk of developing- optic neuropathy if they and effective, produces clinical and haematological are smokers. -

Hydroxocobalamin for Injection) for Intravenous Infusion Alternative Therapies, If Available, in Patients with Known Anaphylactic Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION -------------------------------CONTRAINDICATIONS----------------------------- These highlights do not include all the information needed to use None (4) CYANOKIT safely and effectively. See full prescribing information for CYANOKIT. ------------------------WARNINGS AND PRECAUTIONS----------------------- Risk of Anaphylaxis and Other Hypersensitivity Reactions: Consider CYANOKIT® (hydroxocobalamin for injection) for intravenous infusion alternative therapies, if available, in patients with known anaphylactic Initial U.S. Approval: 1975 reactions to hydroxocobalamin or cyanocobalamin. (5.2) Risk of Renal Injury: Acute renal failure with acute tubular necrosis, renal ----------------------------RECENT MAJOR CHANGES-------------------------- impairment and urine calcium oxalate crystals have been reported Warnings and Precautions, Risk of Renal Injury (5.3) 12/2018 following CYANOKIT therapy. Monitor renal function for 7 days Warnings and Precautions, Use of Blood Cyanide Assay (5.7) 12/2018 following CYANOKIT therapy. (5.3) Risk of Increased Blood Pressure: Substantial increases in blood pressure ----------------------------INDICATIONS AND USAGE--------------------------- may occur following CYANOKIT therapy. Monitor blood pressure during CYANOKIT is indicated for the treatment of known or suspected cyanide treatment. (5.4) poisoning. (1) -------------------------------ADVERSE REACTIONS------------------------------ ------------------------DOSAGE AND ADMINISTRATION---------------------- Most common -

Enriched Flour
PAPRIKA OLEORESIN FOR COLOR, SOY LECITHIN. Ingredients: ENRICHED FLOUR (WHEAT FLOUR, NIACIN, REDUCED IRON, THIAMIN MONONITRATE [VITAMIN B1], RIBOFLAVIN [VITAMIN B2], FOLIC ACID), VEGETABLE OIL (SOYBEAN AND PALM OIL WITH TBHQ FOR FRESHNESS), CHEESE MADE WITH SKIM MILK (SKIM MILK, WHEY PROTEIN, CHEESE CULTURES, SALT, ENZYMES, ANNATTO EXTRACT FOR COLOR), CONTAINS TWO PERCENT OR LESS OF SALT, PAPRIKA, YEAST, INGREDIENTS CRUST: WHOLE GRAIN OATS, ENRICHED FLOUR (WHEAT FLOUR, NIACIN, REDUCED IRON, VITAMIN B1 [THIAMIN MONONITRATE], VITAMIN B2 [RIBOFLAVIN], FOLIC ACID), WHOLE WHEAT FLOUR, SOYBEAN AND/OR CANOLA OIL, SOLUBLE CORN FIBER, SUGAR, DEXTROSE, FRUCTOSE, CALCIUM CARBONATE, WHEY, WHEAT BRAN, SALT, CELLULOSE, POTASSIUM BICARBONATE, NATURAL AND ARTIFICIAL FLAVOR, CINNAMON, MONO- AND DIGLYCERIDES, SOY LECITHIN, WHEAT GLUTEN, NIACINAMIDE, VITAMIN A PALMITATE, CARRAGEENAN, ZINC OXIDE, REDUCED IRON, GUAR GUM, VITAMIN B6 (PYRIDOXINE HYDROCHLORIDE), VITAMIN B1 (THIAMIN HYDROCHLORIDE), VITAMIN B2 (RIBOFLAVIN), FILLING: INVERT SUGAR, CORN SYRUP, APPLE PUREE CONCENTRATE, GLYCERIN, SUGAR, MODIFIED CORN STARCH, SODIUM ALGINATE, MALIC ACID, METHYLCELLULOSE, DICALCIUM PHOSPHATE, CINNAMON, CITRIC ACID, CARAMEL COLOR. CONTAINS WHEAT, MILK AND SOY INGREDIENTS CRUST: WHOLE GRAIN OATS, ENRICHED FLOUR (WHEAT FLOUR, NIACIN, REDUCED IRON, VITAMIN B1 [THIAMIN MONONITRATE], VITAMIN B2 [RIBOFLAVIN], FOLIC ACID), WHOLE WHEAT FLOUR, SOYBEAN AND/OR CANOLA OIL, SOLUBLE CORN FIBER, SUGAR, DEXTROSE, FRUCTOSE, CALCIUM CARBONATE, WHEY, WHEAT BRAN, SALT, CELLULOSE, POTASSIUM -

Circulatory and Urinary B-Vitamin Responses to Multivitamin Supplement Ingestion Differ Between Older and Younger Adults
nutrients Article Circulatory and Urinary B-Vitamin Responses to Multivitamin Supplement Ingestion Differ between Older and Younger Adults Pankaja Sharma 1,2 , Soo Min Han 1 , Nicola Gillies 1,2, Eric B. Thorstensen 1, Michael Goy 1, Matthew P. G. Barnett 2,3 , Nicole C. Roy 2,3,4,5 , David Cameron-Smith 1,2,6 and Amber M. Milan 1,3,4,* 1 The Liggins Institute, University of Auckland, Auckland 1023, New Zealand; [email protected] (P.S.); [email protected] (S.M.H.); [email protected] (N.G.); [email protected] (E.B.T.); [email protected] (M.G.); [email protected] (D.C.-S.) 2 Riddet Institute, Palmerston North 4474, New Zealand; [email protected] (M.P.G.B.); [email protected] (N.C.R.) 3 Food & Bio-based Products Group, AgResearch, Palmerston North 4442, New Zealand 4 High-Value Nutrition National Science Challenge, Auckland 1023, New Zealand 5 Department of Human Nutrition, University of Otago, Dunedin 9016, New Zealand 6 Singapore Institute for Clinical Sciences, Agency for Science, Technology, and Research, Singapore 117609, Singapore * Correspondence: [email protected]; Tel.: +64-(0)9-923-4785 Received: 23 October 2020; Accepted: 13 November 2020; Published: 17 November 2020 Abstract: Multivitamin and mineral (MVM) supplements are frequently used amongst older populations to improve adequacy of micronutrients, including B-vitamins, but evidence for improved health outcomes are limited and deficiencies remain prevalent. Although this may indicate poor efficacy of supplements, this could also suggest the possibility for altered B-vitamin bioavailability and metabolism in older people. -

Adult BLS Standing Orders • Ensure EMS Provider Safety, Consider HAZMAT Activation
Imperial County Public Health Department Emergency Medical Services Agency Policy/Procedure/Protocol Manual Treatment Protocols Date: 07/01/2021 Poisoning/Intoxication/Envenomation - Adult Policy #9160A Adult BLS Standing Orders • Ensure EMS provider safety, consider HAZMAT activation. Recognize, Notify, Isolate • Universal Patient Protocol • Do not approach patient or location if scene safety is in question • Obtain accurate history of incident: o Name of product or substance o Quantity ingested, and/or duration of exposure o Time elapsed since exposure o If safe and accessible, bring medications or bottles to hospital • Move victim(s) to safe environment • Externally decontaminate - PRN • Continuously monitor ECG, blood pressure, pulse oximetry, and capnography (if ALS present) PRN • Give oxygen and provide airway support per Airway Policy • Contact Poison Control Center as needed 1 (800) 222-1222 Suspected Opioid Overdose with Respirations <12 RPM • If possible, avoid the use of a supraglottic device prior to the administration of naloxone • Administer naloxone 0.1 mg/kg, max of 2 mg IN. May repeat up to three (3) times, q5min • May assist family/friends on-scene with administration of patient’s own naloxone • NOTE - Use with caution in opioid dependent pain management patients • Assess vitals, with specific attention to respiratory rate and respiratory drive • Note pupil exam • Note drug paraphernalia or medication bottles near patient Suspected Stimulant Overdose with Sudden Hypoventilation, Oxygen Desaturation, or Apnea • High flow -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

About Thiamine (B1) and Thiamine Deficiency
NLOSS North London Obesity Surgery Service About Thiamine (B1) and Thiamine Deficiency What does thiamine do? Thiamine (vitamin B1) is an important nutrient for taking energy from food and turning it into energy for your brain, nerves and heart. It is needed by the body to process carbohydrates, fats, and proteins – but it is most important for how we process carbohydrates (sugars and starches). What happens if my thiamine is low/if I don’t get enough thiamine? Your body stores very little thiamine, so deficiency can happen very quickly – especially if you are not eating much or if you are vomiting for any reason. Thiamine deficiency may be called Beriberi or Wernicke’s Encephalopathy depending on how it presents. When you don’t get enough thiamine, you may first have nausea, vomiting, loss of appetite, fatigue and difficulty concentrating. You may also have weakness, sleepiness, changes in personality and memory, leg and foot cramping, burning feet, headache, constipation, and cramping. If thiamine deficiency is severe, serious problems can result including loss of hearing, permanent nerve damage, coma, permanent brain damage, heart damage, liver damage, and death. What are other symptoms? Other symptoms of thiamine deficiency include: • Blurred or double vision • Difficulty urinating • Difficulty taking/swallowing • Numb/painful hands/feet • Facial weakness • Foot drop, leg weakness • Amnesia, memory loss, dementia • Clumsiness, loss of balance, • Rapid heartbeat falling • Faintness on standing up • Loss of muscle • Leg swelling Where can I get thiamine? Thiamine is found throughout the diet, but fortified cereals, beans/peas, nuts and pork are very good sources. Other sources are also milk, cheese, fresh and dried fruit, and eggs. -
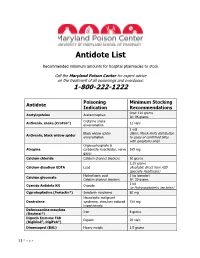
Antidote List
Antidote List Recommended minimum amounts for hospital pharmacies to stock Call the Maryland Poison Center for expert advice on the treatment of all poisonings and overdoses: 1-800-222-1222 Poisoning Minimum Stocking Antidote Indication Recommendations Oral: 120 grams Acetylcysteine Acetaminophen IV: 96 grams Crotaline snake Antivenin, snake (CroFab®) 12 vials envenomation 1 vial Black widow spider (Note: Merck limits distribution Antivenin, black widow spider envenomation to cases of confirmed bites with symptoms only) Organophosphate & Atropine carbamate insecticides, nerve 165 mg gases Calcium chloride Calcium channel blockers 10 grams 2.25 grams Calcium disodium EDTA Lead (Available direct from ASD Specialty Healthcare) Hydrofluoric acid 1 kg (powder) Calcium gluconate Calcium channel blockers IV: 30 grams 1 kit Cyanide Antidote Kit Cyanide (or Hydroxocobalamin, see below) Cyproheptadine (Periactin®) Serotonin syndrome 80 mg Neuroleptic malignant Dantrolene syndrome, stimulant-induced 720 mg hyperthermia Deferoxamine mesylate Iron 8 grams (Desferal®) Digoxin Immune FAB Digoxin 20 vials (Digibind®, DigiFab®) Dimercaprol (BAL) Heavy metals 1.5 grams 1 | P a g e Maryland Poison Center Antidote List – continued Poisoning Minimum Stocking Antidote Indication Recommendations DMSA (Succimer, Chemet®) Heavy metals 2000 mg Folic acid Methanol IV: 150 mg Flumazenil (Romazicon®) Benzodiazepines 10 mg Fomepizole (Antizol®) Ethylene glycol, methanol 12 grams Beta blockers, Glucagon 50 mg calcium channel blockers Hydroxocobalamin (Cyanokit®) Cyanide -

Cyanocobalamin Decision Document
Cyanocobalamin Decision Document Drug Cyanocobalamin (Vitamin B12) Brands Cyanocobalamin (all preparations including Cytacon tablets, Cytamen Injection) Decision West Essex CCG does not commission cyanocobalamin. Date 29th August 2019 Evidence Vitamins were included in the NHS England - Conditions for which over the counter items should not routinely be prescribed in primary care: Guidance for CCGs (29 March 2018) Vitamins and minerals should not be routinely prescribed in primary care due to limited evidence of clinical effectiveness. Exceptions: Medically diagnosed deficiency, including for those patients who may have a lifelong or chronic condition or have undergone surgery that results in malabsorption. Continuing need should however be reviewed on a regular basis. NB maintenance or preventative treatment is not an exception. Calcium and vitamin D for osteoporosis. Malnutrition including alcoholism (see NICE guidance) Patients suitable to receive Healthy start vitamins for pregnancy or children between the ages 6 months to their fourth birthday. (NB this is not on prescription but commissioned separately) British National Formulary Anaemia, megalobastic – overview Most megaloblastic anaemias result from a lack of either vitamin B12 or folate, and it is essential to establish in every case which deficiency is present and the underlying cause. In emergencies, when delay might be dangerous, it is sometimes necessary to administer both substances after the bone marrow test while plasma assay results are awaited. Normally, however, appropriate treatment should not be instituted until the results of tests are available. One cause of megaloblastic anaemia in the UK is pernicious anaemia in which lack of gastric intrinsic factor resulting from an autoimmune gastritis causes malabsorption of vitamin B12.