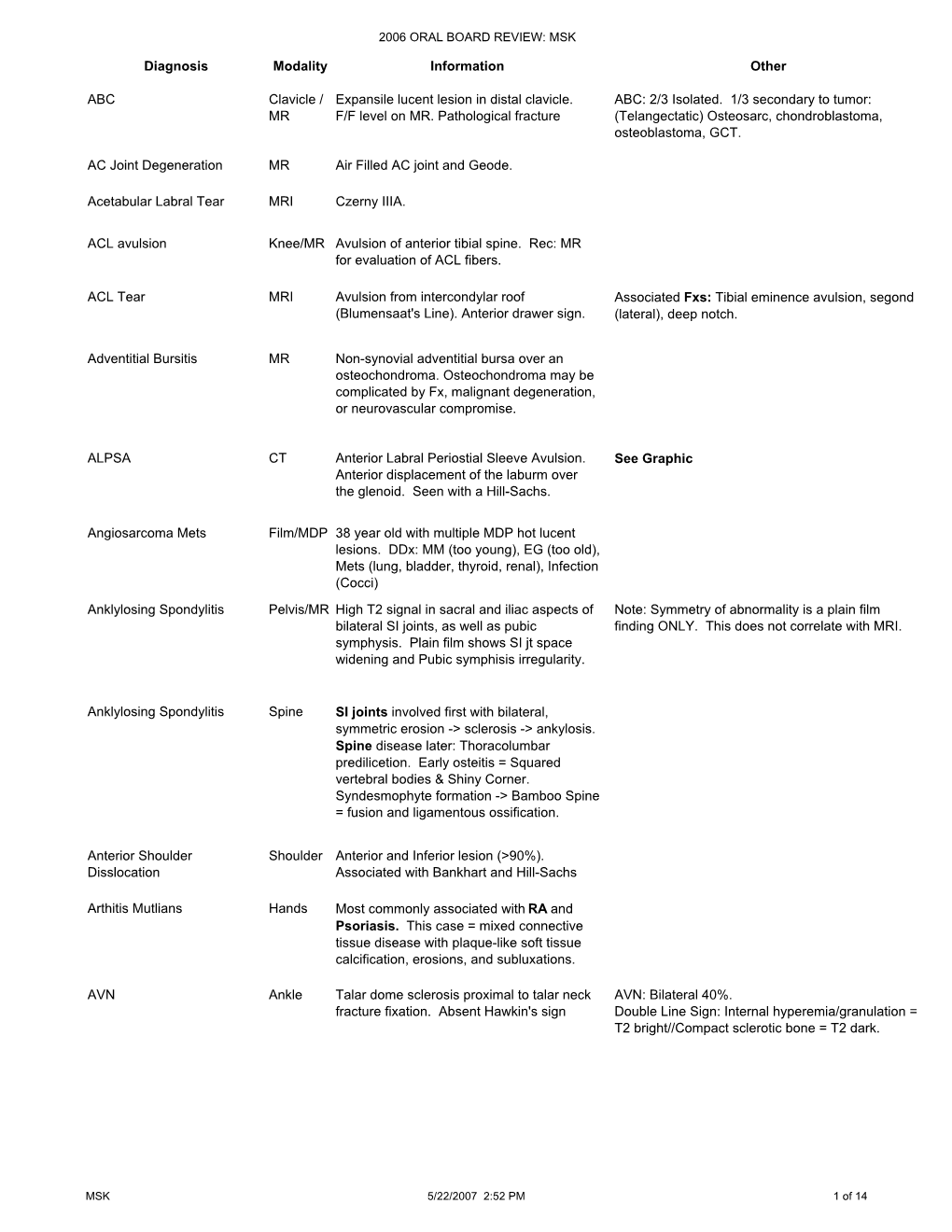
Diagnosis Modality Information Other ABC Clavicle / MR Expansile Lucent
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Elbow Arthroscopy for Osteochondral Lesions in Athletes
SPORTS SURGERY ELBOW ARTHROSCOPY FOR OSTEOCHONDRAL LESIONS IN ATHLETES – Written by Luigi Pederzini et al, Italy Several sports specific injuries of the elbow OSTEOCHONDRAL DEFECT have been well-described. For example, Definition and symptoms the prevalence of medial elbow instability Osteochondral defect is a detachment is high in throwing athletes such as of bone and cartilage in a joint that can Osteochondral baseball players. Similarly, javelin throwers, cause pain. The clinical presentation defect is a volleyball players and tennis players are is characterised by an acute or chronic frequently complaining about elbow pain. onset of symptoms. The majority of detachment of This can be the result of intensive training patients with osteochondral defects of or chronic overuse which results in an the elbow complain of pain. In some bone and cartilage acute or chronic injury. Some of these patients the defect is associated with injuries can be osteochondral lesions such a loose body, and the patient presents in a joint that as osteochondral defects, osteochondrosis clinically with pain, giving way, swelling, can cause pain... of the capitulum humeri or osteochondritis catching, clicking, crepitus and elbow dissecans (OCD). stiffness aggravated by joint movements. characterised Standard X-rays are the initial studies of choice, but sometimes are negative. by an acute or Magnetic resonance imaging (MRI) and 3D computed tomography (CT) scan can chronic onset of be extremely useful in establishing an symptoms. accurate diagnosis and to add in pre- operative planning. 210 OSTEOCHONDROSIS OF CAPITULUM HUMERI (PANNER’S DISEASE) Definition and symptoms Panner’s disease, an ostechondrosis of the capitellum, is a rare disorder that usually affects the dominant elbow in individuals younger than 10 years old. -

SAS Journal of Surgery (SASJS) Panner's Disease: About a Case
SAS Journal of Surgery (SASJS) ISSN 2454-5104 Abbreviated Key Title: SAS J. Surg. ©Scholars Academic and Scientific Publishers (SAS Publishers) A Unit of Scholars Academic and Scientific Society, India Panner's Disease: About A Case Mohamed Ben-Aissi1, Redouane Hani1, Mohammed Kadiri1, Mouad Beqqali-Hassani1, Paolo Palmari2, Moncef Boufettal1, Mohamed Kharmaz1, Moulay Omar Lamrani1, Ahmed El Bardouni1, Mustapha Mahfoud1, Mohamed Saleh Berrada1 1Orthopedic surgery and traumatology department, Ibn Sina Hospital, Rabat, Morocco 2Orthopedic surgery and traumatology departemnt, Robert Ballanger Hospital, Paris, France Abstract: Panner's disease, or osteochondrosis of the lateral condylar nucleus, is an Case Report avascular necrosis leading to subchondral bone loss, it was first described in 1927. We report a case of Panner's disease, which has been evolving since 1 month, in a child of 8 *Corresponding author years sportsman practicing karate. The evolution was favorable with restitution ad Mohamed Ben-Aissi integrum in 8 months after a short anti-inflammatory treatment and a sports rest of 3 months, without any immobilization of the neither elbow nor surgical intervention. Article History Keywords: Osteochondrosis, Panner’s disease, Treatment. Received: 03.10.2018 Accepted: 06.10.2018 INTRODUCTION Published: 30.10.2018 Panner's disease, or osteochondrosis of the lateral condylar nucleus, is an avascular necrosis leading to a loss of subchondral bone fissuring the radio-humeral DOI: articular surfaces, occurring in the hyperspottive child, in connection with an overuse of 10.21276/sasjs.2018.4.10.7 the elbow [1, 2]. It was first described in 1927 by Dane Panner, a Danish orthopedic surgeon [2, 3]. -

Pediatric MSK Protocols
UT Southwestern Department of Radiology Ankle and Foot Protocols - Last Update 5-18-2015 Protocol Indications Notes Axial Coronal Sagittal Ankle / Midfoot - Routine Ankle Pain Axial = In Relation to Leg "Footprint" (Long Axis to Foot) T1 FSE PD SPAIR T1 FSE Injury, Internal Derangement Coronal = In Relation to Leg (Short Axis Foot) PD SPAIR STIR Talar OCD, Coalition Protocol Indications Notes Axial Coronal Sagittal Ankle / Midfoot - Arthritis Arthritis Axial = In Relation to Leg "Footprint" (Long Axis to Foot) PD SPAIR PD SPAIR T1 FSE Coronal = In Relation to Leg (Short Axis Foot) STIR T1 SPIR POST T1 SPIR POST Protocol Indications Notes Axial Coronal Sagittal Foot - Routine Pain, AVN Axial = In Relation to Leg "Footprint" (Long Axis to Foot) T1 FSE PD FSE T1 FSE Coronal = In Relation to Leg (Short Axis Foot) PD SPAIR PD SPAIR STIR Protocol Indications Notes Axial Coronal Sagittal Foot - Arthritis Arthritis Axial = In Relation to Leg "Footprint" (Long Axis to Foot) T1 FSE PD SPAIR STIR Coronal = In Relation to Leg (Short Axis Foot) PD SPAIR T1 SPIR POST 3D WATS T1 SPIR POST Protocol Indications Notes Axial Coronal Sagittal Great Toe / MTP Joints Turf Toe Smallest Coil Possible (Microcoil if Available) PD FSE T1 FSE PD FSE Sesamoiditis FoV = Mid Metatarsal Through Distal Phalanges PD SPAIR PD SPAIR PD SPAIR Slice thickness = 2-3 mm, 10% gap Axial = In relation to the great toe (short axis foot) Coronal = In relation to the great toe (long axis foot / footprint) Appropriate Coronal Plane for Both Ankle and Foot Imaging UT Southwestern Department -
SPR 2015 the Good, the Bad and the Ugly
SPR 2015 The Good, the Bad and the Ugly Diego Jaramillo, M.D., M.P.H. Department of Radiology Children’s Hospital of Philadelphia University of Pennsylvania Pearlman School of Medicine Variants, small abnormalities, and disease are closelyo related Little holes in the humeral head? Developmental proximal humeral cyst Posterior, adjacent to union between greater and lesser tuberosity Cyst related to rotator cuff injury (courtesy of Tal Laor, MD) • Anterior, adjacent to footprint (insertion) Intertuberosity Cysts vs. Rotator Cuff Cyts Intertuberosity Rotator Cuff Cysts Cysts Age (yr) <15 >10 Location Posterior Anterior Rotator Cuff Not usually Yes Disease Little hole in the capitellum? Osteochondral injury with loose body Acute Osteochondral Injuries • Anterior capitellum • Fragment usually detaches at o-c junction • Only acute changes in the bone Persistent pain after a fall 13-year-old competitive tennis player Osteochondritis Dissecans 6 month follow up Osteochondritis Dissecans • Anterior to inferior capitellum • Bone marrow edema • Cystic changes • Findings similar to those of OCD in the knee 8-year-old with elbow pain Panner’s Disease • Osteonecrosis of the capitellum • First decade • Repetitive trauma 17 “Pseudo Panner”: Irregular ossification variant Regarding elbow OCD and Panner’s disease, which of these statements is true: 1. Both affect the same age group 2. The trochlea is the structure most frequently affected by Panner’s disease 3. The capitellum is the structure most frequently affected by OCD 4. The articular cartilage is disrupted in Panner’s disease Regarding elbow OCD and Panner’s disease, which of these statements is true: 1. Both affect the same age group 2. -

Sports Injuries in Children Continued
Me d i c i n eT o d a y PEER REVIEWED ARTICLE POINTS: 2 CPD/1 PDP Sports injuries in childre n The number of children with sports injuries seen in sports medicine practices is increasing. The usual outcome is full recovery, but the consequence of a missed diagnosis of a more serious condition may be significant for the child. The important issue of encouraging children to be injuries seen in sports medicine practices appears more active in an effort to improve their overall to be actually increasing.1 , 2 health is a complex public health problem.1 , 2 Fortunately, many of the sports injuries that Childhood sports participation in Australia has occur in children are self-limited and full recovery unfortunately declined over the past few decades. is the usual outcome. However, more serious con- Some 86% of children aged 5 to 14 years were ditions may occasionally occur and the conse- active in sport in 1985, but by 2003, the level of quence of a missed diagnosis, especially during the participation had fallen to 54% for girls and 69% rapid pubertal growth phase, may be significant for boys.1 During this time period, the number of for the child. overweight and obese children has been increas- Pain in a child should not be dismissed as ‘grow- TOM CROSS ing. At the other end of the spectrum, more active ing pains’. If an informed systematic approach FACSP, MBBS, DCH children are training more intensively and for is followed, the clinical assessment of a child will longer periods of time in one or several sports. -

Childhood and Adolescent Sports-Related Overuse Injuries KYLE J
Childhood and Adolescent Sports-Related Overuse Injuries KYLE J. CASSAS, M.D., and AMELIA CASSETTARI-WAYHS, M.D., Methodist Health System, Dallas, Texas Youth sports participation carries an inherent risk of injury, includ- ing overuse injuries. Little leaguer’s shoulder, a stress fracture of the proximal humerus that presents as lateral shoulder pain, usually is self- limited. Little leaguer’s elbow is a medial stress injury; treatment con- sists of complete rest from throwing for four to six weeks followed by rehabilitation and a gradual throwing program. Spondylolysis is a stress fracture of the pars interarticularis. Diagnostic modalities include plain film radiography, bone scan, computed tomography, single photon emission computed tomography, and magnetic resonance imaging. Treatment usually is conservative. Spondylolisthesis is the forward or anterior displacement of one vertebral body over another and may be related to a history of spondylolysis. Diagnosis is made with plain film radiography and graded according to the amount of displacement. Osgood-Schlatter disease presents as anterior knee pain localized to the tibial tubercle. Diagnosis is made clinically, and most patients respond to conservative measures. Calcaneal apophysitis (or Sever’s disease) is a common cause of heel pain in young athletes, presenting as pain in the posterior aspect of the calcaneus. (Am Fam Physician 2006;73:1014-22. Copyright © 2006 American Academy of Family Physicians.) SCOTT BY ILLUSTRATION BODELL S Patient information: ach year in the United States, develop in young athletes when this growth A handout on Osgood- approximately 30 million children center is unable to meet the demands placed Schlatter disease is available online at http:// and teenagers participate in orga- on it during activity. -

Panner Disease
Panner Disease Panner disease is a condition which affects the end of the humerus (upper arm bone). The lower arm has two bones, called the radius and ulna. Panner disease is the name for flattening of the end of the humerus where it joins with the radius. This area is called the capitellum. In children, bones grow at certain spots called growth plates. The growth plates are usually located at the end of the bone. In children with Panner disease, the growth plate at the end of the humerus loses its blood supply and the nearby bone softens and collapses. Panner disease is most often seen in children, typically boys but sometimes girls, between the ages of 5 and 10. Usually their dominant arm (i.e., right arm if they are right-handed) is affected. It usually gets better if properly treated, but can result in the child having trouble straightening out their arm completely. Causes It is unclear exactly why some children get Panner disease. The tendency to get Panner disease may run in families. One theory is that repeated mild injuries may simply add up to cause this problem; the finding that Panner disease tends to occur in the dominant elbow supports this idea. Panner disease usually affects children in the 5-10 year old age range and occurs more commonly in boys than in girls. Symptoms Panner disease leads to elbow pain. The pain tends to start out of the blue without any specific injury to the area. The pain is usually on the outer edge of the elbow, which is near where the capitellum is located. -

Pediatric Orthopedics in Practice, DOI 10.1007/978-3-662-46810-4, © Springer-Verlag Berlin Heidelberg 2015 880 Backmatter
879 Backmatter Subject Index – 880 F. Hefti, Pediatric Orthopedics in Practice, DOI 10.1007/978-3-662-46810-4, © Springer-Verlag Berlin Heidelberg 2015 880 Backmatter Subject index Bold letters: Principal article Italics: Illustrations A Acetylsalicylic acid 303, 335 Adolescent scoliosis Amyloidosis 663 Acheiropodia 804 7 Scoliosis Amyoplasia 813–814 Abducent nerve paresis 752, Achievement by proxy 10, 11 AFO 7 Ankle Foot Orthosis Anaerobes 649, 652, 657 816 Achilles tendon Aggrecan 336, 367, 762 ANA 7 antinuclear antibodies Abducted pes planovalgus – lengthening 371, 426, 431, aggressive osteomyelitis Analysis, gait 488, 490–497 433, 434, 436, 439, 443, 464, 7 osteomyelitis, aggressive 7 Gait analysis Abduction contracture 468, 475, 485, 487–490, 493, Agonist 281, 487, 492, 493, Anchor 169, 312, 550, 734 7 contracture 496, 816, 838, 840 495, 498, 664, 832, 835, 840, Andersen classification abduction pants 219–221 – shortening 358, 418, 431, 868 7 classification, Andersen Abduction splint 212, 218–221, 433, 464, 465, 467, 468, 475, Ahn classification 366 Andry, Nicolas 21, 22 248, 850 489, 496, 838 Aitken classification (congenital Anesthesia 26, 38, 135, 154, Abduction Achondrogenesis 750, 751, femoral deficiency ) 7 classi- 162, 174, 221, 243, 247, 248, – hip 195, 198, 199, 212, 213, 756, 758–760, 769 fication, femoral deficiency 255, 281, 303, 385, 386, 400, 214, 218, 219, 220, 221, Achondroplasia 56, 163, 166, Akin osteotomy 477, 479 500, 506, 559, 568, 582–585, 241–245, 247, 248, 251, 255, 242, 270, 271, 353, 409, 628, Albers-Schönberg -

Xiii CONTENTS 1. Skeletal Development, Anatomy, and Function
CONTENTS 1. Skeletal Development, Anatomy, and Function . 1 Development . 1 Ossification. 1 Bone Structure . 14 Extracellular Matrix: Molecular Organization. 14 Gross Anatomy and Histology. 17 Bone Cell Types . 28 Osteoblasts . 29 Osteocytes . 32 Osteoclasts. 33 Cartilage . 33 The General Approach to Orthopedic Diseases . 45 2. Imaging of Non-Neoplastic Musculoskeletal Disorders . 55 Radiography. 55 Nuclear Medicine. 60 Sonography. 63 Computerized Tomography. 66 Magnetic Resonance Imaging . 70 3. Inherited and Developmental Bone Diseases. 85 Normal Anatomy and Histology of the Growth Plate. 86 Pathologic Assessment: General Guidelines . 87 Growth Abnormalities Primarily Affecting Shape . 90 Gaucher Disease. 90 Niemann-Pick Disease. 98 Sickle Cell Disease. 100 Hemochromatosis. 108 Growth Abnormalities Primarily Affecting Size. 113 Hypopituitarism. 114 Nutritional Dwarfism. 116 Acromegaly and Gigantism . 117 Growth Abnormalities Affecting Both Size and Shape . 120 Skeletal Dysplasias . 120 Disproportionate Short Stature with Extremities Shorter than Trunk. 124 Thanatophoric Dysplasia. 124 Achondroplasia . 139 Pseudoachondroplasia . 146 xiii Non-Neoplastic Diseases of Bones and Joints Campomelic Dysplasia. 152 Diastrophic Dysplasia . 156 Disproportionate Short Stature with Extremities Longer than Trunk. 160 Mucopolysaccharidoses . 160 Limb Reduction Abnormalities/Limb Deficiencies/Dysmelia. 171 Amelia/Phocomelia. 171 Proximal Femoral Focal Deficiency (Femur-Fibula-Ulna) Syndrome . 178 Supernumerary Digits/Polydactyly . 183 Lipid Storage -

Abt—Letterer—Siwe Disease 400 Accessory Bones 4 Acetabular
1105 Index A osteophytes 950 cervical spinous processes 631 atelosteogenesis 6 productive bone changes 69 cervical vertebrae 599, 626, 629, atheroma, calcified of calvarium 405 Abt—Letterer—Siwe disease 400 sesamoid bones 1091 631, 632 athyrosis, sella turcica 453 accessory bones 4 acromioclavicular joint 287–91 double trolley back 704 atlanto-occipital joint 572 acetabular index 816 anomalies 287–8 lumbar vertebrae 702–6 arthritis 599 depth-to-width 817, 818 calcification 287, 290 occipitoatlantoaxial joints 600 dislocation 596, 597 acetabulum degenerative change 290 sacroiliitis 755–6 dysplasia 622 accessory bones 821–2, 823 dislocation 280, 288, 289 thoracic vertebrae 662, 663 motion 573 accessory fossa 824 fractures 288, 289 triple trolley back 704 osteoarthritis 601 anatomy 811, 813, 814 inflammation 290 ankylosis synostosis 435, 588–9 apophyses joint space widening 290, 302 acquired bony 27–8 atlanto-occipital membrane, anterior marginal 804, 806–7 necrosis 289–90 apophyseal joint spaces 612, 613 603 persistence 821–2 normal variants 287–8 carpal inflammatory 131 atlantoaxial joint persistent accessory 807 osteoarthritis 290, 291 cervical spine 629, 630 fusions 589 bony defect 824 posttraumatic ossification 289 sacroiliac joint 758 osteoarthritis 601, 602 center—edge angle of Wiberg 817, pseudodislocation 288, 289 thoracic vertebrae 662–3 rotational analysis 574 818 rheumatic disorders 290 annulus fibrosus 558 atlantoaxial segmentation, irregular components 804 subluxation 288, 289 calcification 721, 722, 723 590 congenital dislocation -

Training Manual FOREWORD
SICOT Training Manual FOREWORD Maps and guides are essential to all who seek destinations, who know where they want to go but who need help to get there. All trainees determined to become successful surgeons need similar maps in the form of educational objectives which will help them reach their destinations. Maps, as with educational objectives, must be kept up-to-date when necessary, as new knowledge becomes available. SICOT is dedicated to the improvement of orthopaedic surgery throughout the world. The most certain way of achieving its goal is to help in the education of surgeons. We have borrowed the Educational Objectives of the Canadian Orthopaedic Association to help us in our task. These objectives provide a guide to a basic orthopaedic training or education. They set a standard for trainees to achieve and assure the trainee of an acceptable level of knowledge. They can inform examiners of what a candidate should know at the end of training. Regional and local knowledge requirements can be added to reflect the incidence of endemic disease. It is our hope that these Educational Objectives will form a part of the training in most SICOT member countries and help to provide a common link between universities or teaching hospitals in all our nations. ACKNOWLEDGEMENTS SICOT is pleased to acknowledge the generosity of the Canadian Orthopaedic Association in providing the material for this publication. Special thanks go to Dr Garth Johnston and Dr Merv Letts of Ottawa, Canada. Anthony J. Hall , Secretary General of SICOT, 1993-2002 Charles -

Osteochondritis Dissecans
CLINICAL Osteochondritis Dissecans REVIEW Indexing Metadata/Description › Title/condition: Osteochondritis Dissecans › Synonyms:Osteochondrosis dissecans; dissecans, osteochondritis; dissecans, osteochondrosis › Anatomical location/body part affected: Curved articular surfaces of most joints in the upper and lower extremities/glenoid fossa of shoulder, capitellum of elbow, femoral condyle of knee, talar dome of ankle, metatarsal head in foot › Area(s) of specialty: Orthopedic Rehabilitation, Pediatric Rehabilitation, Sports Rehabilitation › Description • Osteochondritis dissecans (OCD) is an idiopathic disorder of subchondral bone and articular cartilage in which a segment of the subchondral bone separates from the surrounding bone. Progression of the defect can result in varying degrees of fragmentation from the articular surface and surrounding cartilage.(19) The osteochondral defects are associated with joint pain, inflammation, catching/locking, and impaired functional mobility • If the growth plate has fused, OCD is defined as adult. If the growth plate has not fused, OCD is defined as juvenile(19) • The joints most commonly affected are the following:(3) –Roughly 75% of OCD cases involve the knee, especially the medial femoral condyle, and 75–80% of cases are unilateral –Elbow (6%) (humeral capitellum) –Ankle (4%) (talus) –Combination of other joints (15%) • Despite the suffix “itis,” inflammation has not been shown to be of significance in OCD. Osteochondrosis or osteochondral lesion may be a more appropriate term to describe this