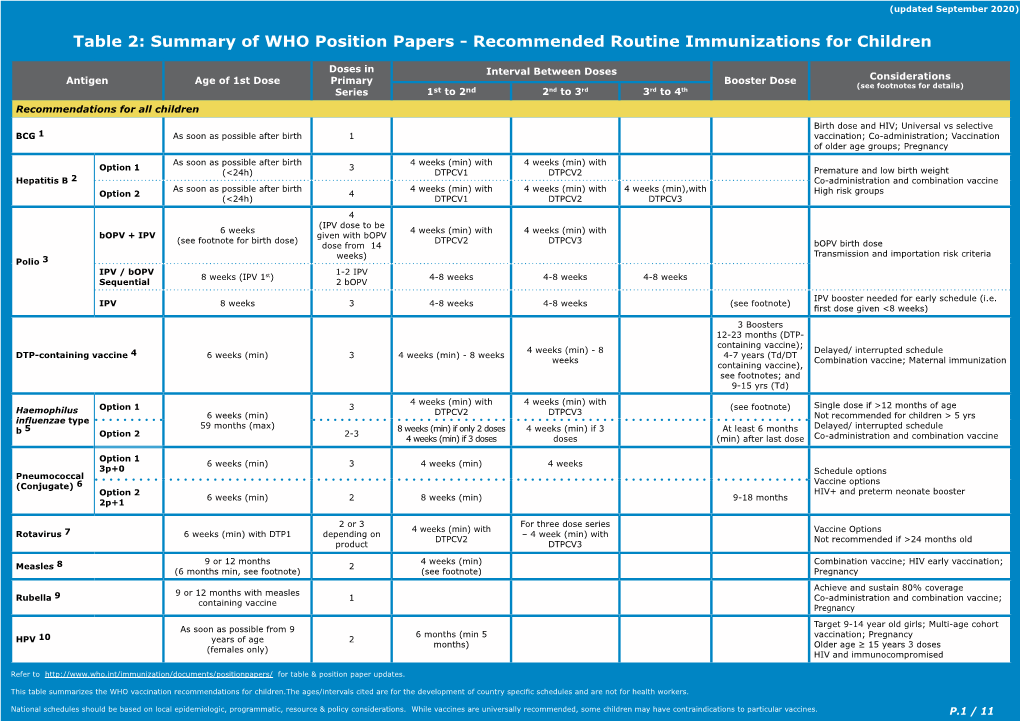
Recommended Routine Immunizations for Children
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recognizing When a Child's Injury Or Illness Is Caused by Abuse
U.S. Department of Justice Office of Justice Programs Office of Juvenile Justice and Delinquency Prevention Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE U.S. Department of Justice Office of Justice Programs 810 Seventh Street NW. Washington, DC 20531 Eric H. Holder, Jr. Attorney General Karol V. Mason Assistant Attorney General Robert L. Listenbee Administrator Office of Juvenile Justice and Delinquency Prevention Office of Justice Programs Innovation • Partnerships • Safer Neighborhoods www.ojp.usdoj.gov Office of Juvenile Justice and Delinquency Prevention www.ojjdp.gov The Office of Juvenile Justice and Delinquency Prevention is a component of the Office of Justice Programs, which also includes the Bureau of Justice Assistance; the Bureau of Justice Statistics; the National Institute of Justice; the Office for Victims of Crime; and the Office of Sex Offender Sentencing, Monitoring, Apprehending, Registering, and Tracking. Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE NCJ 243908 JULY 2014 Contents Could This Be Child Abuse? ..............................................................................................1 Caretaker Assessment ......................................................................................................2 Injury Assessment ............................................................................................................4 Ruling Out a Natural Phenomenon or Medical Conditions -

Clinical Update and Treatment of Lactation Insufficiency
Review Article Maternal Health CLINICAL UPDATE AND TREATMENT OF LACTATION INSUFFICIENCY ARSHIYA SULTANA* KHALEEQ UR RAHMAN** MANJULA S MS*** SUMMARY: Lactation is beneficial to mother’s health as well as provides specific nourishments, growth, and development to the baby. Hence, it is a nature’s precious gift for the infant; however, lactation insufficiency is one of the explanations mentioned most often by women throughout the world for the early discontinuation of breast- feeding and/or for the introduction of supplementary bottles. Globally, lactation insufficiency is a public health concern, as the use of breast milk substitutes increases the risk of morbidity and mortality among infants in developing countries, and these supplements are the most common cause of malnutrition. The incidence has been estimated to range from 23% to 63% during the first 4 months after delivery. The present article provides a literary search in English language of incidence, etiopathogensis, pathophysiology, clinical features, diagnosis, and current update on treatment of lactation insufficiency from different sources such as reference books, Medline, Pubmed, other Web sites, etc. Non-breast-fed infant are 14 times more likely to die due to diarrhea, 3 times more likely to die of respiratory infection, and twice as likely to die of other infections than an exclusively breast-fed child. Therefore, lactation insufficiency should be tackled in appropriate manner. Key words : Lactation insufficiency, lactation, galactagogue, breast-feeding INTRODUCTION Breast-feeding is advised becasue human milk is The synonyms of lactation insufficiency are as follows: species-specific nourishment for the baby, produces lactational inadequacy (1), breast milk insufficiency (2), optimum growth and development, and provides substantial lactation failure (3,4), mothers milk insufficiency (MMI) (2), protection from illness. -

SIDS and Other Sleep-Related Infant Deaths: Expansion of Recommendations for a Safe Infant Sleeping Environment
Organizational Principles to Guide and Define the Child Health Care System and/or Improve the Health of all Children POLICY STATEMENT SIDS and Other Sleep-Related Infant Deaths: Expansion of Recommendations for a Safe Infant Sleeping Environment TASK FORCE ON SUDDEN INFANT DEATH SYNDROME abstract KEY WORDS Despite a major decrease in the incidence of sudden infant death syn- SIDS, sudden infant death, infant mortality, sleep position, bed- sharing, tobacco, pacifier, immunization, bedding, sleep surface drome (SIDS) since the American Academy of Pediatrics (AAP) released ABBREVIATIONS its recommendation in 1992 that infants be placed for sleep in a non- SIDS—sudden infant death syndrome prone position, this decline has plateaued in recent years. Concur- SUID—sudden unexpected infant death rently, other causes of sudden unexpected infant death that occur AAP—American Academy of Pediatrics during sleep (sleep-related deaths), including suffocation, asphyxia, This document is copyrighted and is property of the American and entrapment, and ill-defined or unspecified causes of death have Academy of Pediatrics and its Board of Directors. All authors have filed conflict of interest statements with the American increased in incidence, particularly since the AAP published its last Academy of Pediatrics. Any conflicts have been resolved through statement on SIDS in 2005. It has become increasingly important to a process approved by the Board of Directors. The American address these other causes of sleep-related infant death. Many of the Academy of Pediatrics has neither solicited nor accepted any commercial involvement in the development of the content of modifiable and nonmodifiable risk factors for SIDS and suffocation are this publication. -

Definitions of Child Abuse and Neglect
STATE STATUTES Current Through March 2019 WHAT’S INSIDE Defining child abuse or Definitions of Child neglect in State law Abuse and Neglect Standards for reporting Child abuse and neglect are defined by Federal Persons responsible for the child and State laws. At the State level, child abuse and neglect may be defined in both civil and criminal Exceptions statutes. This publication presents civil definitions that determine the grounds for intervention by Summaries of State laws State child protective agencies.1 At the Federal level, the Child Abuse Prevention and Treatment To find statute information for a Act (CAPTA) has defined child abuse and neglect particular State, as "any recent act or failure to act on the part go to of a parent or caregiver that results in death, https://www.childwelfare. serious physical or emotional harm, sexual abuse, gov/topics/systemwide/ or exploitation, or an act or failure to act that laws-policies/state/. presents an imminent risk of serious harm."2 1 States also may define child abuse and neglect in criminal statutes. These definitions provide the grounds for the arrest and prosecution of the offenders. 2 CAPTA Reauthorization Act of 2010 (P.L. 111-320), 42 U.S.C. § 5101, Note (§ 3). Children’s Bureau/ACYF/ACF/HHS 800.394.3366 | Email: [email protected] | https://www.childwelfare.gov Definitions of Child Abuse and Neglect https://www.childwelfare.gov CAPTA defines sexual abuse as follows: and neglect in statute.5 States recognize the different types of abuse in their definitions, including physical abuse, The employment, use, persuasion, inducement, neglect, sexual abuse, and emotional abuse. -

Overcoming Breastfeeding Concerns- Part 2
9/21/2018 OVERCOMING BREASTFEEDING Presented by: CONCERNS- PART 2 Kary Johnson, IBCLC OVERVIEW • Pacifiers • Pumping • Low Milk Supply • Feeding Multiples • Supplementation • Discharge Guidelines PICTURE FROM HTTPS://WWW.ETSY.COM/LISTING/464346270/BREAST-ENCOURAGEMENT-CARD-BREASTFEEDING 1 9/21/2018 PACIFIERS Step 9: Counsel mothers on the use and risks of feeding bottles, teats and pacifiers. What does the AAP say? •NG/Gavage •“Mothers of healthy term infants should be instructed to use pacifiers at •Hypoglycemia infant nap or sleep time after breastfeeding is well established, at Infant approximately 3 go 4 weeks of age.” •Lab draws • “Pacifier use should be limited to specific medical situations. These include Pain •Circumcision uses for pain relief, as a calming agent, or as part of a structured program •Illness for enhancing oral motor function.” •Medications Maternal •PMAD • NICU: to organize suck, swallow, breathe pattern of premature infant (in addition to reasons above) (AAP, 2012) PACIFIERS Ask yourself…what is the reason for use? Management: • All effort should be made to prevent separation of mom & baby (i.e. newborn nursery) • Avoid overuse • Be careful to not incorrectly pacify infant hunger • Non-nutritive sucking on mother’s breast is a great alternative Overuse or misuse results in: • Decreased breastfeeding duration • Reduced milk supply • Dental issues, difficulty weaning, and use well into childhood 2 9/21/2018 BREAST PUMPING Reasons a mother may need to pump: • Nipple trauma • Low milk supply • Late preterm infants -
Summary of Supportive Science Regarding Thimerosal Removal
Summary of Supportive Science Regarding Thimerosal Removal Updated December 2012 www.safeminds.org Science Summary on Mercury in Vaccines (Thimerosal Only) SafeMinds Update – December 2012 Contents ENVIRONMENTAL IMPACT ................................................................................................................................. 4 A PILOT SCALE EVALUATION OF REMOVAL OF MERCURY FROM PHARMACEUTICAL WASTEWATER USING GRANULAR ACTIVATED CARBON (CYR 2002) ................................................................................................................................................................. 4 BIODEGRADATION OF THIOMERSAL CONTAINING EFFLUENTS BY A MERCURY RESISTANT PSEUDOMONAS PUTIDA STRAIN (FORTUNATO 2005) ......................................................................................................................................................................... 4 USE OF ADSORPTION PROCESS TO REMOVE ORGANIC MERCURY THIMEROSAL FROM INDUSTRIAL PROCESS WASTEWATER (VELICU 2007)5 HUMAN & INFANT RESEARCH ............................................................................................................................ 5 IATROGENIC EXPOSURE TO MERCURY AFTER HEPATITIS B VACCINATION IN PRETERM INFANTS (STAJICH 2000) .................................. 5 MERCURY CONCENTRATIONS AND METABOLISM IN INFANTS RECEIVING VACCINES CONTAINING THIMEROSAL: A DESCRIPTIVE STUDY (PICHICHERO 2002) ...................................................................................................................................................... -

Supplemental Information and Guidance for Vaccination Providers Regarding Use of 9-Valent HPV Vaccine
Supplemental information and guidance for vaccination providers regarding use of 9-valent HPV A 9-valent human papillomavirus (HPV) vaccine (9vHPV, Gardasil 9, Merck & Co.) was licensed for use in females and males in December 2014.1,2,3,4 The 9vHPV was the third HPV vaccine licensed in the United States by the Food and Drug Administration (FDA); the other vaccines are bivalent HPV vaccine (2vHPV, Cervarix, GlaxoSmithKline), licensed for use in females, and quadrivalent HPV vaccine (4vHPV, Gardasil, Merck & Co.), licensed for use in females and males.5 In February 2015, the Advisory Committee on Immunization Practices (ACIP) recommended 9vHPV as one of three HPV vaccines that can be used for routine vaccination of females and one of two HPV vaccines for routine vaccination of males.6 After the end of 2016, only 9vHPV will be distributed in the United States. In October 2016, ACIP updated HPV vaccination recommendations regarding dosing schedules.7 CDC now recommends two doses of HPV vaccine (0, 6–12 month schedule) for persons starting the vaccination series before the 15th birthday. Three doses of HPV vaccine (0, 1–2, 6 month schedule) continue to be recommended for persons starting the vaccination series on or after the 15th birthday and for persons with certain immunocompromising conditions. Guidance is needed for persons who started the series with 2vHPV or 4vHPV and may be completing the series with 9vHPV. The information below summarizes some of the recommendations included in ACIP Policy Notes and provides additional guidance.5-7 Information about the vaccines What are some of the similarities and differences between the three HPV vaccines? y Each of the three HPV vaccines is a noninfectious, virus-like particle (VLP) vaccine. -

Pediatric Respiratory Rates Age Rate (Breaths Per Minute)
Pediatric Respiratory Rates Age Rate (breaths per minute) Infant (birth–1 year) 30–60 Toddler (1–3 years) 24–40 Preschooler (3–6 years) 22–34 School-age (6–12 years) 18–30 Adolescent (12–18 years) 12–16 Pediatric Pulse Rates Age Low High Infant (birth–1 year) 100 160 Toddler (1–3 years) 90 150 Preschooler (3–6 years) 80 140 School-age (6–12 years) 70 120 Adolescent (12–18 years) 60 100 Pulse rates for a child who is sleeping may be 10 percent lower than the low rate listed. Low-Normal Pediatric Systolic Blood Pressure Age* Low Normal Infant (birth–1 year) greater than 60* Toddler (1–3 years) greater than 70* Preschooler (3–6 years) greater than 75 School-age (6–12 years) greater than 80 Adolescent (12–18 years) greater than 90 *Note: In infants and children aged three years or younger, the presence of a strong central pulse should be substituted for a blood pressure reading. Pediatric CUPS Assessment Category Assessment Actions Example Critical Absent airway, Perform rapid initial Severe traumatic injury breathing, or interventions and transport with respiratory arrest or circulation simultaneously cardiac arrest Unstable Compromised airway, Perform rapid initial Significant injury with breathing, or interventions and transport respiratory distress, circulation with simultaneously active bleeding, shock; altered mental status near-drowning; unresponsiveness Potentially Normal airway, Perform initial assessment Minor fractures; unstable breathing, circulation, with interventions; transport pedestrian struck by car and mental status BUT -

Pediatric Immunizations: Immunization Current Recommended Chedule and Ecommendations Immunization Schedule
Online Continuing Education for Nurses Linking Learning to Performance INSIDE THIS COURSE PEDIATRIC IMMUNIZATIONS: IMMUNIZATION CURRENT RECOMMENDED SCHEDULE AND RECOMMENDATIONS IMMUNIZATION SCHEDULE ................ 1 ROUTINE IMMUNIZATIONS ............. 2 COMBINATION VACCINES .............. 6 2.27 Contact Hours VACCINATION ADMINISTRATION ......... 7 Written By: Erin Azuse, RN, BSN VACCINATION REACTIONS ................ 8 CONTRAINDICATIONS TO OBJECTIVES RECEIVING VACCINATIONS ............... 9 1. List the current recommended schedule of MISCONCEPTIONS ABOUT VACCINATIONS ................................ 9 immunizations per the CDC and discuss how the list is updated. THE FUTURE FOR PEDIATRIC IMMUNIZATIONS ............................. 10 2. Identify 10 preventable diseases for which REFERENCES ................................ 11 children routinely receive immunizations. CE EXAM...................................... 13 3. Discuss symptoms and complications of these EVALUATION ................................. 16 diseases. 4. Be familiar with combination vaccines and their components. 5. Explain the proper nursing procedure for administering vaccinations. 6. Identify the potential reactions that may occur from immunizations. 7. Describe any contraindications to receiving immunizations. 8. Identify common misconceptions about vaccinations and describe the nurse’s role in changing this. CURRENT RECOMMENDED IMMUNIZATION SCHEDULE The Centers for Disease Control and Prevention (CDC) recommends a schedule of routine vaccinations to protect against -

Vaccine Hesitancy
WHY CHILDREN WORKSHOP ON IMMUNIZATIONS ARE NOT VACCINATED? VACCINE HESITANCY José Esparza MD, PhD - Adjunct Professor, Institute of Human Virology, University of Maryland School of Medicine, Baltimore, MD, USA - Robert Koch Fellow, Robert Koch Institute, Berlin, Germany - Senior Advisor, Global Virus Network, Baltimore, MD, USA. Formerly: - Bill & Melinda Gates Foundation, Seattle, WA, USA - World Health Organization, Geneva, Switzerland The value of vaccination “The impact of vaccination on the health of the world’s people is hard to exaggerate. With the exception of safe water, no other modality has had such a major effect on mortality reduction and population growth” Stanley Plotkin (2013) VACCINES VAILABLE TO PROTECT AGAINST MORE DISEASES (US) BASIC VACCINES RECOMMENDED BY WHO For all: BCG, hepatitis B, polio, DTP, Hib, Pneumococcal (conjugated), rotavirus, measles, rubella, HPV. For certain regions: Japanese encephalitis, yellow fever, tick-borne encephalitis. For some high-risk populations: typhoid, cholera, meningococcal, hepatitis A, rabies. For certain immunization programs: mumps, influenza Vaccines save millions of lives annually, worldwide WHAT THE WORLD HAS ACHIEVED: 40 YEARS OF INCREASING REACH OF BASIC VACCINES “Bill Gates Chart” 17 M GAVI 5.6 M 4.2 M Today (ca 2015): <5% of children in GAVI countries fully immunised with the 11 WHO- recommended vaccines Seth Berkley (GAVI) The goal: 50% of children in GAVI countries fully immunised by 2020 Seth Berkley (GAVI) The current world immunization efforts are achieving: • Equity between high and low-income countries • Bringing the power of vaccines to even the world’s poorest countries • Reducing morbidity and mortality in developing countries • Eliminating and eradicating disease WHY CHILDREN ARE NOT VACCINATED? •Vaccines are not available •Deficient health care systems •Poverty •Vaccine hesitancy (reticencia a la vacunacion) VACCINE HESITANCE: WHO DEFINITION “Vaccine hesitancy refers to delay in acceptance or refusal of vaccines despite availability of vaccination services. -

Hepatitis B Vaccination Schedule and PVS Guidance for Infants Born to Hepatitis B Positive Women
Hepatitis B Vaccination Schedule and PVS Guidance for Infants Born to Hepatitis B Positive Women Pediatric Hepatitis B Vaccination Schedule and Product Options Following the birth dose of hepatitis B vaccine and HBIG, the infant needs either two doses of monovalent hepatitis B vaccine or three doses of a hepatitis B-containing combination vaccine to complete the hepatitis B vaccine series. In particular, please note: . Pediarix should not be administered before 6 weeks of age. The final dose of hepatitis B vaccine (either the third or fourth dose) should be given on or after 6 months of age. Do not give it before 24 weeks of age. Comvax is not approved for use in infants born to hepatitis B positive women OPTION 1: Monovalent hepatitis B vaccine schedule (Energix or Recombivax) Dose Timing Dose 1 (given with HBIG) Within 12 hours after birth Dose 2 1-2 months of age Dose 3 6 months of age Post-vaccination serology (HBsAg and anti-HBs) 1-2 months after last dose, but not before 9 months of age OPTION 2: Pediarix vaccine schedule Dose Timing Dose of monovalent hep B vaccine (given with HBIG) Within 12 hours after birth Dose 2 6 weeks to 2 months of age (do not administer before 6 weeks of age) Dose 3 4 months of age Dose 4 6 months of age Post-vaccination serology (HBsAg and anti-HBs) 1-2 months after last dose, but not before 9 months of age Post-vaccination Serology (PVS) Results and Recommended Follow-up Serology result Follow-up needed HBsAg negative None. -

Recommended Adult Immunization Schedule
Recommended Adult Immunization Schedule UNITED STATES for ages 19 years or older 2021 Recommended by the Advisory Committee on Immunization Practices How to use the adult immunization schedule (www.cdc.gov/vaccines/acip) and approved by the Centers for Disease Determine recommended Assess need for additional Review vaccine types, Control and Prevention (www.cdc.gov), American College of Physicians 1 vaccinations by age 2 recommended vaccinations 3 frequencies, and intervals (www.acponline.org), American Academy of Family Physicians (www.aafp. (Table 1) by medical condition and and considerations for org), American College of Obstetricians and Gynecologists (www.acog.org), other indications (Table 2) special situations (Notes) American College of Nurse-Midwives (www.midwife.org), and American Academy of Physician Assistants (www.aapa.org). Vaccines in the Adult Immunization Schedule* Report y Vaccines Abbreviations Trade names Suspected cases of reportable vaccine-preventable diseases or outbreaks to the local or state health department Haemophilus influenzae type b vaccine Hib ActHIB® y Clinically significant postvaccination reactions to the Vaccine Adverse Event Hiberix® Reporting System at www.vaers.hhs.gov or 800-822-7967 PedvaxHIB® Hepatitis A vaccine HepA Havrix® Injury claims Vaqta® All vaccines included in the adult immunization schedule except pneumococcal 23-valent polysaccharide (PPSV23) and zoster (RZV) vaccines are covered by the Hepatitis A and hepatitis B vaccine HepA-HepB Twinrix® Vaccine Injury Compensation Program. Information on how to file a vaccine injury Hepatitis B vaccine HepB Engerix-B® claim is available at www.hrsa.gov/vaccinecompensation. Recombivax HB® Heplisav-B® Questions or comments Contact www.cdc.gov/cdc-info or 800-CDC-INFO (800-232-4636), in English or Human papillomavirus vaccine HPV Gardasil 9® Spanish, 8 a.m.–8 p.m.