Mixing and Matching: Layering Medications As Family Physicians
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Use Evaluation: Antipsychotic Utilization in Schizophrenia Patients
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35 Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 Drug Use Evaluation: Antipsychotic Utilization in Schizophrenia Patients Research Questions: 1. How many schizophrenia patients are prescribed recommended first-line second-generation treatments for schizophrenia? 2. How many schizophrenia patients switch to an injectable antipsychotic after stabilization on an oral antipsychotic? 3. How many schizophrenia patients are prescribed 2 or more concomitant antipsychotics? 4. Are claims for long-acting injectable antipsychotics primarily billed as pharmacy or physician administered claims? 5. Does adherence to antipsychotic therapy differ between patients with claims for different routes of administration (oral vs. long-acting injectable)? Conclusions: In total, 4663 schizophrenia patients met inclusion criteria, and approximately 14% of patients (n=685) were identified as treatment naïve without claims for antipsychotics in the year before their first antipsychotic prescription. Approximately 45% of patients identified as treatment naïve had a history of remote antipsychotic use, but it is unclear if antipsychotics were historically prescribed for schizophrenia. Oral second-generation antipsychotics which are recommended as first-line treatment in the MHCAG schizophrenia algorithm were prescribed as initial treatment in 37% of treatment naive patients and 28% of all schizophrenia patients. Recommended agents include risperidone, paliperidone, and aripiprazole. Utilization of parenteral antipsychotics was limited in patients with schizophrenia. Overall only 8% of patients switched from an oral to an injectable therapy within 6 months of their first claim. Approximately, 60% of all schizophrenia patients (n=2512) had claims for a single antipsychotic for at least 12 continuous weeks and may be eligible to transition to a long-acting injectable antipsychotic. -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -
Lithium Sulfate
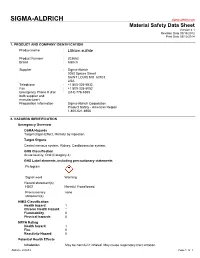
SIGMA-ALDRICH sigma-aldrich.com Material Safety Data Sheet Version 4.1 Revision Date 09/14/2012 Print Date 03/12/2014 1. PRODUCT AND COMPANY IDENTIFICATION Product name : Lithium sulfate Product Number : 203653 Brand : Aldrich Supplier : Sigma-Aldrich 3050 Spruce Street SAINT LOUIS MO 63103 USA Telephone : +1 800-325-5832 Fax : +1 800-325-5052 Emergency Phone # (For : (314) 776-6555 both supplier and manufacturer) Preparation Information : Sigma-Aldrich Corporation Product Safety - Americas Region 1-800-521-8956 2. HAZARDS IDENTIFICATION Emergency Overview OSHA Hazards Target Organ Effect, Harmful by ingestion. Target Organs Central nervous system, Kidney, Cardiovascular system. GHS Classification Acute toxicity, Oral (Category 4) GHS Label elements, including precautionary statements Pictogram Signal word Warning Hazard statement(s) H302 Harmful if swallowed. Precautionary none statement(s) HMIS Classification Health hazard: 1 Chronic Health Hazard: * Flammability: 0 Physical hazards: 0 NFPA Rating Health hazard: 1 Fire: 0 Reactivity Hazard: 0 Potential Health Effects Inhalation May be harmful if inhaled. May cause respiratory tract irritation. Aldrich - 203653 Page 1 of 7 Skin Harmful if absorbed through skin. May cause skin irritation. Eyes May cause eye irritation. Ingestion Harmful if swallowed. 3. COMPOSITION/INFORMATION ON INGREDIENTS Formula : Li2O4S Molecular Weight : 109.94 g/mol Component Concentration Lithium sulphate CAS-No. 10377-48-7 - EC-No. 233-820-4 4. FIRST AID MEASURES General advice Move out of dangerous area.Consult a physician. Show this safety data sheet to the doctor in attendance. If inhaled If breathed in, move person into fresh air. If not breathing, give artificial respiration. Consult a physician. -

Management and Treatment of Lithium-Induced Nephrogenic Diabetes Insipidus
REVIEW Management and treatment of lithium- induced nephrogenic diabetes insipidus Christopher K Finch†, Lithium carbonate is a well documented cause of nephrogenic diabetes insipidus, with as Tyson WA Brooks, many as 10 to 15% of patients taking lithium developing this condition. Clinicians have Peggy Yam & Kristi W Kelley been well aware of lithium toxicity for many years; however, the treatment of this drug- induced condition has generally been remedied by discontinuation of the medication or a †Author for correspondence Methodist University reduction in dose. For those patients unresponsive to traditional treatment measures, Hospital, Department several pharmacotherapeutic regimens have been documented as being effective for the of Pharmacy, University of management of lithium-induced diabetes insipidus including hydrochlorothiazide, Tennessee, College of Pharmacy, 1265 Union Ave., amiloride, indomethacin, desmopressin and correction of serum lithium levels. Memphis, TN 38104, USA Tel.: +1 901 516 2954 Fax: +1 901 516 8178 [email protected] Lithium carbonate is well known for its wide use associated with a mutation(s) of vasopressin in bipolar disorders due to its mood stabilizing receptors. Acquired causes are tubulointerstitial properties. It is also employed in aggression dis- disease (e.g., sickle cell disease, amyloidosis, orders, post-traumatic stress disorders, conduct obstructive uropathy), electrolyte disorders (e.g., disorders and even as adjunctive therapy in hypokalemia and hypercalcemia), pregnancy, or depression. Lithium has many well documented conditions induced by a drug (e.g., lithium, adverse effects as well as a relatively narrow ther- demeclocycline, amphotericin B and apeutic range of 0.4 to 0.8 mmol/l. Clinically vincristine) [3,4]. Lithium is the most common significant adverse effects include polyuria, mus- cause of drug-induced nephrogenic DI [5]. -

Should Inverse Agonists Be Defined by Pharmacological Mechanism Or
CNS Spectrums,(2019), 24 419 – 425. © Cambridge University Press 2018. This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited. doi:10.1017/S1092852918000986 ORIGINAL RESEARCH Switching stable patients with schizophrenia from their oral antipsychotics to aripiprazole lauroxil: a post hoc safety analysis of the initial 12-week crossover period Peter J. Weiden,1* Yangchun Du,2 Chih-Chin Liu,2 and Arielle D. Stanford3 1 Medical Affairs, Alkermes, Inc., Waltham, Massachusetts, USA 2 Clinical Development, Alkermes, Inc., Waltham, Massachusetts, USA 3 Clinical Science, Alkermes, Inc., Waltham, Massachusetts, USA Objective. Switching antipsychotic medications is common in patients with schizophrenia who are experiencing persistent symptoms or tolerability issues associated with their current drug regimen. This analysis assessed the safety of switching from an oral antipsychotic to the long-acting injectable antipsychotic aripiprazole lauroxil (AL). Methods. This was a post hoc analysis of outpatients with schizophrenia who were prescribed an oral antipsychotic and who enrolled in an international, open-label, long-term (52-week) safety study of AL. The analysis focused on the first 3 injections of AL 882 mg over 12 weeks, divided into the immediate 4-week crossover period between the first and second AL injections (initiation phase) and the subsequent 8 weeks (stabilization phase). Patients were grouped by preswitch oral antipsychotic medication, and safety and clinical symptoms were assessed. Results. In total, 190 patients had switched from one of the following oral antipsychotic medications: aripiprazole, conventional antipsychotics, risperidone/paliperidone, olanzapine, or quetiapine. -

Advice on Prescribing for Adults with Obsessive-Compulsive Disorder (OCD)
Advice on Prescribing for Adults with Obsessive-Compulsive Disorder (OCD) Dr Lynne M Drummond, Local and National OCD Services, Behavioural and Cognitive Psychotherapy Unit, South West London and St George’s Menat Health NHS Trust 9th April 2008 Introduction Obsessive-Compulsive Disorder (OCD) is a common psychiatric disorder which untreated has a chronic often deteriorating course. OCD does respond well to treatment with either psychological approaches involving Graded Exposure and Self-Imposed Ritual Prevention (ERP) or with specific pharmacological agents. This paper aims to outline the various psychopharmacological approaches. Psychopharmacological approaches Repeated trials have demonstrated that drugs which act of the serotonin system are effective in many patients with OCD (SRI and SSRIs) • The Selective Serotonin Reuptake Inhibitors (SSRIs) are generally used as first line rather than clomipramine (a Serotonin Reuptake Inhibitor- SRI) due to fewer side effects. • There is little evidence of any particular advantage of any of the SSRIs apart from some evidence that Escitalopram* may reduce relapse of OCD. • In general if there is no response to the SRI on maximal doses for 12 weeks it is worthwhile switching to an alternative. • However there is evidence that benefit from SRI can accrue over as long as 2 years Drug Dose Major side effects Any special features Seizures in a small number of patients The first SRI to and less likely if demonstrate Clomipramine Up to 225mg at <250mg effectiveness in night (increase reducing OCD slowly as tolerated) Sexual Dysfunction symptoms in 80 % Dry mouth; blurred It is a tricyclic vision drowsiness; antidepressant weight gain and orthostatic hypotension 1 50 mg in evening Gastro-intestinal initially and upsets; anorexia and increased weight loss. -

Subchronic Lithium Treatment Increases the Anxiolytic-Like Effect of Mirtazapine on the Expression of Contextual Title Conditioned Fear
Subchronic lithium treatment increases the anxiolytic-like effect of mirtazapine on the expression of contextual Title conditioned fear Author(s) An, Yan; Inoue, Takeshi; Kitaichi, Yuji; Nakagawa, Shin; Wang, Ce; Chen, Chong; Song, Ning; Kusumi, Ichiro European journal of pharmacology, 747, 13-17 Citation https://doi.org/10.1016/j.ejphar.2014.11.009 Issue Date 2015-01-15 Doc URL http://hdl.handle.net/2115/58243 Type article (author version) File Information AnManuscript.pdf Instructions for use Hokkaido University Collection of Scholarly and Academic Papers : HUSCAP Subchronic lithium treatment increases the anxiolytic-like effect of mirtazapine on the expression of contextual conditioned fear Yan Ana, Takeshi Inouea*, Yuji Kitaichia, Shin Nakagawaa, Ce Wangb, Chong Chena, Ning Songa, Ichiro Kusumia a Department of Psychiatry, Hokkaido University Graduate School of Medicine, North 15, West 7, Kita-ku, Sapporo 060-8638, Japan b Department of Neuropharmacology, Hokkaido University Graduate School of Medicine, North 15, West 7, Kita-ku, Sapporo 060-8638, Japan Number of figures: 3 Corresponding address: Takeshi Inoue, Department of Psychiatry, Hokkaido University Graduate School of Medicine, North 15, West 7, Kita-ku, Sapporo 060-8638, Japan Phone: +81(11)706-5160 Fax: +81(11)706-5081 E-mail: [email protected] 1 Abstract Lithium not only has a mood-stabilizing effect but also the augmentation effect of an antidepressant, the mechanism of which remains unclear. Although lithium may augment the effect of mirtazapine, this augmentation has not been confirmed. Using a contextual fear conditioning test in rats, an animal model of anxiety or fear, we examined the effect of subchronic lithium carbonate (in diet) in combination with systemic mirtazapine on the expression of contextual conditioned fear. -

CENTRAL NERVOUS SYSTEM DEPRESSANTS Opioid Pain Relievers Anxiolytics (Also Belong to Psychiatric Medication Category) • Codeine (In 222® Tablets, Tylenol® No
CENTRAL NERVOUS SYSTEM DEPRESSANTS Opioid Pain Relievers Anxiolytics (also belong to psychiatric medication category) • codeine (in 222® Tablets, Tylenol® No. 1/2/3/4, Fiorinal® C, Benzodiazepines Codeine Contin, etc.) • heroin • alprazolam (Xanax®) • hydrocodone (Hycodan®, etc.) • chlordiazepoxide (Librium®) • hydromorphone (Dilaudid®) • clonazepam (Rivotril®) • methadone • diazepam (Valium®) • morphine (MS Contin®, M-Eslon®, Kadian®, Statex®, etc.) • flurazepam (Dalmane®) • oxycodone (in Oxycocet®, Percocet®, Percodan®, OxyContin®, etc.) • lorazepam (Ativan®) • pentazocine (Talwin®) • nitrazepam (Mogadon®) • oxazepam ( Serax®) Alcohol • temazepam (Restoril®) Inhalants Barbiturates • gases (e.g. nitrous oxide, “laughing gas”, chloroform, halothane, • butalbital (in Fiorinal®) ether) • secobarbital (Seconal®) • volatile solvents (benzene, toluene, xylene, acetone, naptha and hexane) Buspirone (Buspar®) • nitrites (amyl nitrite, butyl nitrite and cyclohexyl nitrite – also known as “poppers”) Non-Benzodiazepine Hypnotics (also belong to psychiatric medication category) • chloral hydrate • zopiclone (Imovane®) Other • GHB (gamma-hydroxybutyrate) • Rohypnol (flunitrazepam) CENTRAL NERVOUS SYSTEM STIMULANTS Amphetamines Caffeine • dextroamphetamine (Dexadrine®) Methelynedioxyamphetamine (MDA) • methamphetamine (“Crystal meth”) (also has hallucinogenic actions) • methylphenidate (Biphentin®, Concerta®, Ritalin®) • mixed amphetamine salts (Adderall XR®) 3,4-Methelynedioxymethamphetamine (MDMA, Ecstasy) (also has hallucinogenic actions) Cocaine/Crack -
Lithium Sulfate, Technical Grade, Min. 99.0 %
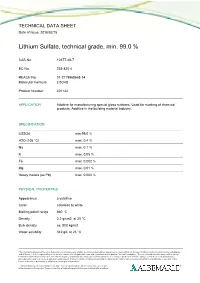
TECHNICAL DATA SHEET Date of Issue: 2018/02/15 Lithium Sulfate, technical grade, min. 99.0 % CAS-No. 10377-48-7 EC-No. 233-820-4 REACH No. 01-2119968668-14 Molecular Formula Li2O4S Product Number 401142 APPLICATION Additive for manufacturing special glass mixtures. Used for marking of chemical products. Additive in the building material industry. SPECIFICATION Li2SO4 min 99.0 % H2O (105 °C) max. 0.4 % Na max. 0.1 % K max. 0.05 % Fe max. 0.002 % Mg max. 0.01 % Heavy metals (as Pb) max. 0.004 % PHYSICAL PROPERTIES Appearance crystalline Color colorless to white Melting point/ range 860 °C Density 2.2 g/cm3 at 20 °C Bulk density ca. 800 kg/m3 Water solubility 342 g/L at 25 °C The information presented herein is believed to be accurate and reliable, but is presented without guarantee or responsibility on the part of Albemarle Corporation and its subsidiaries and affiliates. It is the responsibility of the user to comply with all applicable laws and regulations and to provide for a safe workplace. The user should consider any health or safety hazards or information contained herein only as a guide, and should take those precautions which are necessary or prudent to instruct employees and to develop work practice procedures in order to promote a safe work environment. Further, nothing contained herein shall be taken as an inducement or recommendation to manufacture or use any of the herein materials or processes in violation of existing or future patent. Technical data sheets may change frequently. You can download the latest version from our website www.albemarle-lithium.com. -

Beyond Amitriptyline
children Review Beyond Amitriptyline: A Pediatric and Adolescent Oriented Narrative Review of the Analgesic Properties of Psychotropic Medications for the Treatment of Complex Pain and Headache Disorders Robert Blake Windsor 1,2,*, Michael Sierra 2,3, Megan Zappitelli 2,3 and Maria McDaniel 1,2 1 Division of Pediatric Pain Medicine, Department of Pediatrics, Prisma Health, Greenville, SC 29607, USA; [email protected] 2 School of Medicine Greenville, University of South Carolina, Greenville, SC 29607, USA; [email protected] (M.S.); [email protected] (M.Z.) 3 Division of Child and Adolescent Psychiatry, Department of Psychiatry, Prisma Health, Greenville, SC 29607, USA * Correspondence: [email protected] Received: 30 October 2020; Accepted: 25 November 2020; Published: 2 December 2020 Abstract: Children and adolescents with recurrent or chronic pain and headache are a complex and heterogenous population. Patients are best served by multi-specialty, multidisciplinary teams to assess and create tailored, individualized pain treatment and rehabilitation plans. Due to the complex nature of pain, generalizing pharmacologic treatment recommendations in children with recurrent or chronic pains is challenging. This is particularly true of complicated patients with co-existing painful and psychiatric conditions. There is an unfortunate dearth of evidence to support many pharmacologic therapies to treat children with chronic pain and headache. This narrative review hopes to supplement the available treatment options for this complex population by reviewing the pediatric and adult literature for analgesic properties of medications that also have psychiatric indication. The medications reviewed belong to medication classes typically described as antidepressants, alpha 2 delta ligands, mood stabilizers, anti-psychotics, anti-sympathetic agents, and stimulants. -

Beyond Lithium in the Treatment of Bipolar Illness Robert M
Beyond Lithium in the Treatment of Bipolar Illness Robert M. Post, M.D., Mark A. Frye, M.D., Kirk D. Denicoff, M.D., Gabriele S. Leverich, L.C.S.W., Tim A. Kimbrell, M.D., and Robert T. Dunn, M.D. Dramatic changes have recently occurred in the availability lamotrigine, gabapentin, and topiramate have unique of treatment options for bipolar illness. Second generation mechanisms of action and deserve further systematic study, mood stabilizing anticonvulsants carbamazepine and as does the potential role for nonconvulsive brain valproate are now widely used as alternatives or adjuncts to stimulation with repeated transcranial magnetic lithium. High potency benzodiazepines are also used as stimulation (rTMS). These and a host of other potential alternatives to typical neuroleptics, and now atypical treatment options now require a new generation of clinical neuroleptics are demonstrating efficacy and better side- trials to help identify clinical and biological markers of effects profiles than the typicals. Thyroid augmentation response and optimal use alone and in complex combination strategies and dihydropyridine L-type calcium channel therapeutic regimens. [Neuropsychopharmacology blockers require further clinical trials to define their role. 19:206–219, 1998] Published by Elsevier Science Inc. Putative third generation mood stabilizing anticonvulsants KEY WORDS: Carbamazepine; Valproate; Calcium channel al. 1989; O’Connell et al. 1991; Denicoff et al. 1997); a blockers; Lamotrigine; Gabapentin; rTMS history of co-morbid substance abuse; and those pa- tients with a history of head trauma or other such medi- There is increasing recognition of the inadequacy of cal co-morbidities as multiple sclerosis, etc. “lithium treatment” in bipolar illness, even with ad- In addition, it is recognized that patients with initial junctive antidepressants and neuroleptics (Maj et al. -

Neuromodulators for Functional Gastrointestinal Disorders (Disorders of Gutlbrain Interaction): a Rome Foundation Working Team Report Douglas A
Gastroenterology 2018;154:1140–1171 SPECIAL REPORT Neuromodulators for Functional Gastrointestinal Disorders (Disorders of GutLBrain Interaction): A Rome Foundation Working Team Report Douglas A. Drossman,1,2 Jan Tack,3 Alexander C. Ford,4,5 Eva Szigethy,6 Hans Törnblom,7 and Lukas Van Oudenhove8 1Center for Functional Gastrointestinal and Motility Disorders, University of North Carolina, Chapel Hill, North Carolina; 2Center for Education and Practice of Biopsychosocial Care and Drossman Gastroenterology, Chapel Hill, North Carolina; 3Translational Research Center for Gastrointestinal Disorders, University of Leuven, Leuven, Belgium; 4Leeds Institute of Biomedical and Clinical Sciences, University of Leeds, Leeds, United Kingdom; 5Leeds Gastroenterology Institute, St James’s University Hospital, Leeds, United Kingdom; 6Departments of Psychiatry and Medicine, University of Pittsburgh, Pittsburgh, Pennsylvania; 7Departments of Internal Medicine and Clinical Nutrition, Institute of Medicine, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden; and 8Laboratory for BrainÀGut Axis Studies, Translational Research Center for Gastrointestinal Disorders, University of Leuven, Leuven, Belgium BACKGROUND & AIMS: Central neuromodulators (antide- summary information and guidelines for the use of central pressants, antipsychotics, and other central nervous neuromodulators in the treatment of chronic gastrointestinal systemÀtargeted medications) are increasingly used for treat- symptoms and FGIDs. Further studies are needed to confirm ment