Drowning Chain of Survival
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Assisting Drowning Victims: Effective Water Rescue Equipment for Lay-Responders
International Journal of Aquatic Research and Education Volume 10 Number 4 Article 8 2-1-2019 Triennial Scientific Review: Assisting Drowning Victims: Effective Water Rescue Equipment for Lay-responders Angela K. Beale-Tawfeeq Rowan University, [email protected] Follow this and additional works at: https://scholarworks.bgsu.edu/ijare Part of the Community Health and Preventive Medicine Commons, Exercise Science Commons, Health and Physical Education Commons, Leisure Studies Commons, Outdoor Education Commons, Sports Sciences Commons, Sports Studies Commons, and the Tourism and Travel Commons Recommended Citation Beale-Tawfeeq, Angela K. (2019) "Triennial Scientific Review: Assisting Drowning Victims: Effective Water Rescue Equipment for Lay-responders," International Journal of Aquatic Research and Education: Vol. 10 : No. 4 , Article 8. DOI: https://doi.org/10.25035/ijare.10.04.08 Available at: https://scholarworks.bgsu.edu/ijare/vol10/iss4/8 This Scientific Literature Review is brought to you for free and open access by the Journals at ScholarWorks@BGSU. It has been accepted for inclusion in International Journal of Aquatic Research and Education by an authorized editor of ScholarWorks@BGSU. Triennial Scientific Review: Assisting Drowning Victims: Effective Water Rescue Equipment for Lay-responders Cover Page Footnote Thanks to members of the aquatic sub-council of the American Red Cross Scientific Advisory Council who provided feedback and editing on this scientific er view. This scientific literature review is available in International -
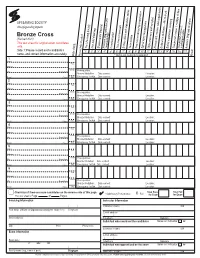
Bronze Cross (Revised 2020) This Test Sheet for Original Exam Candidates Only
Bronze Cross (Revised 2020) This test sheet for original exam candidates only. The Lifesaving Society Non-fatal drowning Shallow water blackout Assistant lifeguard roles and Communication Two-rescuer removals Surface dives and underwater swims Team search Two-rescuer drowning resuscitation Spinal injury management Object recovery and transport Rescue drill: recover submerged victim Endurance challenge – 400 m or yd. Safety supervision scanning Two-person rescue 1: multiple victims Two-person rescue 2: Assistant lifeguard situations responsibilities submerged victim Side 1: Please record each candidate’s 1* 2* 3* 4* 5* 6* 7* 8* 9* 10* 11* 12* 13* 14* 15 16 17 name, and contact information accurately. Date of birth Prerequisits checked * Items are instructor evaluated Result 1 Name Year Address Month City Postal Code Prerequisites: Bronze Medallion Date earned: Location: E-mail Phone Day Emergency 1st Aid Date earned: Location: 2 Name Year Address Month City Postal Code Prerequisites: Bronze Medallion Date earned: Location: E-mail Phone Day Emergency 1st Aid Date earned: Location: 3 Name Year Address Month City Postal Code Prerequisites: Bronze Medallion Date earned: Location: E-mail Phone Day Emergency 1st Aid Date earned: Location: 4 Name Year Address Month Prerequisites: City Postal Code Bronze Medallion Date earned: Location: E-mail Phone Day Emergency 1st Aid Date earned: Location: 5 Name Year Address Month Prerequisites: City Postal Code Bronze Medallion Date earned: Location: E-mail Phone Day Emergency 1st Aid Date earned: Location: 6 Name Year Address Month City Postal Code Prerequisites: BronzeOriginal: Medallion Bronze Medallion Date earned: Date earned: Location: E-mail Phone Day EmergencyRecert: Bronze 1st Aid Cross Date earned: Date earned: Location: Check box if there are more candidates on the reverse side of this page. -

A Guide to Coastal Public Rescue Equipment Contents
Version 1: 2007 A guide to coastal public rescue equipment Contents Foreword 3 Acknowledgements 4 Preface 5 Introduction 7 How this guide was researched 8 Getting started 10 How to use this document 13 Understanding coastal environments 14 Understanding beaches 16 Understanding rocky coasts 19 Understanding tidal inlets and estuaries 20 Understanding man-made coasts 21 Risk management for PRE 22 Selecting public rescue equipment 24 PRE for beaches 26 PRE for rocky coasts, tidal inlets and estuaries 28 PRE for man-made coasts 30 Emergency communications 32 Locating PRE and communications 34 Additional information 40 Signs and user information 42 PRE housing 44 Maintenance 46 Reducing vandalism 47 Useful reading 48 Inside back cover Useful contacts Foreword With the UK having some of Europe’s finest beaches, This guide is the first of its kind, not only in the UK, and with increasing access to other parts of the coast, but worldwide. With credible and robust research, it is unsurprising that millions of people enjoy the UK this guide is in a position to set a world benchmark coastline every year. However, with an increasing trend for coastal public rescue equipment. for recreational activity on our beaches and inshore waters, UK maritime rescue services have never been We therefore welcome and fully endorse this guide so busy helping people in difficulty. and commend all those that were involved in making it happen. Therefore, we are delighted that the RNLI, working closely with members of the National Water Safety Michael Vlasto OBE Forum and other safety organisations, has produced Chairman, National Water Safety Forum this guide for coastal public rescue equipment (PRE): Operations Director, Royal National Lifeboat Institution guidance that beach operators have requested to help manage their beaches safely. -

National Lifeguard
National Lifeguard - Pool Option The primary role of the National Lifeguard is the prevention of emergency situations and the timely and effective resolution of emergencies. The National Lifeguard certification prepares lifeguards to fulfill this role as professional facilitators of safe, enjoyable aquatics in a pool setting. The National Lifeguard program develops the basic lifeguarding skills, principles, and decision‐making process to help lifeguards evaluate and adapt to different aquatic facilities and emergencies. Pre‐requisite: Bronze Cross, Standard First Aid and a minimum of 16 years of age. April 20‐22 & 27‐29, 2018 Fri 4‐9 PM Sat & Sun 8:00 AM – 4:30 PM Taber Aquafun Centre Cost: $351.75 For more information, please contact the Aquafun Centre. (403)223‐5544 ext.3 _________________________________________________________________________________________ Red Cross Water Safety Instructor Course The Water Safety Instructor (WSI) Course prepares candidates to instruct the Red Cross Swim programs. Candidates focus on strategies to introduce and develop fitness activities, skills and water safety, and swimming skills in the Red Cross Swim Preschool, Red Cross Swim Kids, Red Cross Swim @ School, Red Cross Swim @ Camp, Red Cross Swim for Adults & Teens, and Red Cross Swim Adapted programs. Pre-course Requirements:15 years or older by the last day of the WSI - Classroom and Pool, ability to perform Red Cross Swim Kids 10 strokes and skills, and hold one of the following certifications (not required to be current): Red Cross Assistant Lifeguard, Emergency First Aid or equivalent. Course Components, Length & Dates: May 12, 5-10 PM —Introduction & Skills Evaluation* – 5 hours, To be completed before teaching experience—Online – 14–20 hours Teaching hours to be arranged for lessons during summer sessions—min. -

International Life Saving Federation World Drowning Report 2007
International Journal of Aquatic Research and Education Volume 1 Number 4 Article 8 11-1-2007 International Life Saving Federation World Drowning Report 2007 International Life Saving Federation Follow this and additional works at: https://scholarworks.bgsu.edu/ijare Recommended Citation International Life Saving Federation (2007) "International Life Saving Federation World Drowning Report 2007," International Journal of Aquatic Research and Education: Vol. 1 : No. 4 , Article 8. DOI: https://doi.org/10.25035/ijare.01.04.08 Available at: https://scholarworks.bgsu.edu/ijare/vol1/iss4/8 This Position Statement is brought to you for free and open access by the Journals at ScholarWorks@BGSU. It has been accepted for inclusion in International Journal of Aquatic Research and Education by an authorized editor of ScholarWorks@BGSU. International Life Saving Federation: International Life Saving Federation World Drowning Report 2007 SPECIAL SECTION International Journal of Aquatic Research and Education, 2007, 1, 381-401 International Life Saving Federation World Drowning Report 2007 Edition Published September 27, 2007, by The International Life Saving Federation Gemeenteplein 26, 3010 Leuven, Belgium E-mail: [email protected] Web: www.ilsf.org The International Life Saving Federation (www.ilsf.org) is the global confederation of national nonprofit lifesaving organizations. Published by ScholarWorks@BGSU, 2007 381 1 International Journal of Aquatic Research and Education, Vol. 1, No. 4 [2007], Art. 8 382 International Life Saving Federation Preface: The International Life Saving Federation The International Life Saving Federation is a global, non-profit federation of over 100 national lifesaving organisations around the world. The Federation (ILS) leads the worldwide effort to reduce injury and death in, on, or around the water. -

Air Stand-Up Paddle Water Rescue Table: How Can It Help to the Lifeguard?
Rev.int.med.cienc.act.fís.deporte - vol. 18 - número 69 - ISSN: 1577-0354 Palacios-Aguilar, J.; Barcala-Furelos, R.; López-García, S.; Carpentier, M. y Abelairas-Gómez, C. (2018). Tabla Air Stand-Up Paddle de rescate acuático: ¿cómo puede ayudar al socorrista? / Air Table Stand-Up Paddle Water Rescue: How Can You Help The Lifeguard? Revista Internacional de Medicina y Ciencias de la Actividad Física y el Deporte vol. 18 (69) pp. 185-197 Http://cdeporte.rediris.es/revista/revista69/arttabla880.htm DOI: https://doi.org/10.15366/rimcafd2018.69.012 ORIGINAL AIR STAND-UP PADDLE WATER RESCUE TABLE: HOW CAN IT HELP TO THE LIFEGUARD? TABLA AIR STAND-UP PADDLE DE RESCATE ACUÁTICO: ¿CÓMO PUEDE AYUDAR AL SOCORRISTA? Palacios-Aguilar, J.¹; Barcala-Furelos, R.²; López-García, S.³; Carpentier, M.⁴; Abelairas-Gómez, C.⁵ 1 Facultad de Ciencias del Deporte y la Educación Física. Universidad de A Coruña. A Coruña (Spain) [email protected] 2 Facultad de Ciencias de la Educación y del Deporte. Universidad de Vigo. Pontevedra (Spain) [email protected] 3 Facultad de Educación. Universidad Pontificia de Salamanca. Salamanca (Spain) [email protected] 4 Universidad de Brest. Brest (France) [email protected] 5 Facultad de Ciencias de la Salud. Universidad Europea del Atlántico. Santander (Spain) [email protected] Spanish-English translator: Beatriz Palacios Castillo, [email protected] Código UNESCO / UNESCO code: 3212 Salud Publica / Public Health Clasificación Consejo de Europa / Council of Europe Classification: 17. Otras (Salvamento y Socorrismo) / Other (Lifesaving). ACKNOWLEDGMENTS This work would not have been possible without the collaboration of the professional life guards from the town of Puerto del Rosario in Fuerteventura’s island and their coordinator Camilo Lorenzo. -

Annual Report2021
LIFESAVING SOUTH AFRICA ANNUAL REPORT2021 WWW.LIFESAVING.CO.ZA PAGE 3 LIFESAVING SOUTH AFRICA - ANNUAL REPORT 2021 Lifesaving South Africa is the National Authority in the effort to prevent drowning and the Our Vision promotion and delivery of Lifesaving Sport in building an active and winning lifesaving sporting nation in South Africa. Lifesaving South Africa is the National Association for Lifesaving and Lifesaving Sport Our Mission in South Africa. In these roles Lifesaving South Africa leads, supports and partners with national and international organisations committed to drowning prevention, water safety supervision, emergency response and sport. Lifesaving South Africa celebrates the life and acknowledges the passing of members who In Remembrance were part of our family. 1 April 2020 – 31 March 2021 Sally Everitt – Umhlanga Rocks Riaan Wentzel – Strandfontein Derrick Whiting – Pirates Mr Caleb – Strandfontein Farouk May – Kogel Bay Peter Rademeyer – Kings Beach Johan Wepener – Marine Geoff Grylls – Llandudno Bryce Winterburn – Marine Ryan Dunwoodie – Warnadoone Alan Brummer – Marine Haydyn Davies – Warnadoone Heather Jolly – Marine Sean Heilbuth – Warnadoone Athena Malgas – Strandfontein Barry Welsh – Warnadoone Donna Fortuin – Strandfontein Piet Bardenhorst – Warnadoone Wilma Adams – Strandfontein Brian Salmond – Warnadoone Charles Wentzel – Strandfontein LIFESAVING SOUTH AFRICA - ANNUAL REPORT 2021 PAGE 4 INDEX GOVERNMENT PARTNERS 5-6 Presidents Report Dhaya Sewduth 6 Message from the sponsor Princess Charlene of Monaco Foundation -

Lps 07 Fitness Testing for Lifeguards
World Water Safety INTERNATIONAL LIFE SAVING FEDERATION Gemeenteplein 26 – 3010 Leuven – Belgium Tel: (32.16) 89.60.60 – E-mail: [email protected] - Web: www.ilsf.org LIFESAVING POSITION STATEMENT - LPS 07 FITNESS TESTING FOR LIFEGUARDS NOTE: This statement is intended for those lifeguards, acting in a professional or volunteer capacity, who are trained in the techniques of water rescue and resuscitation and who assume a duty to safeguard members of the public at aquatic sites. They may be called lifeguards, lifesavers or both. This statement is not directed at members of the public trained in water safety and rescue techniques, but without a duty to respond, who may also be known, in some areas of the world, as lifesavers. The standards outlined in this position statement are the minimum that ILS recommends. ILS encourages organisations to exceed these recommended minimum standards where local conditions and/or expectations of lifeguards are warranted. BACKGROUND Experts in the field of lifeguard training and rescue believe that lifeguards need to be able to demonstrate a reasonable level of fitness. It is presumed that lifeguards would have sound swimming and water rescue skills. The ability for lifeguards to swim a specified distance within a defined amount of time has been shown to correlate. The available English language studies in the aquatic setting were reviewed. The data is cohort studies of lifeguard pre-employment assessment outcomes. Level of evidence from the research is low and not directly related to the question addressed in this review. There are no direct outcome data for lifeguards responding to victims. -

Supervised Waterfront Operations Equipment
Lifesaving Society Canada Suite 001 – 1145 Hunt Club Road, Ottawa, Ontario K1V 0Y3 Telephone: 613-746-5694 E-mail: [email protected] Web: www.lifesaving.ca Safety Standards for Canadian Swimming Pools and Waterfronts Waterfront Standard Supervised Waterfront Operations Equipment Standard Standard Owners and Operators of supervised waterfronts should ensure that appropriate equipment is available at all times for use by lifeguards on duty. Definitions Last seen marker: A small buoy with a line and anchor that is used to mark the location where a person was last seen in the water. Lifeguard: A person with a current National Lifeguard certification appointed by the owner or operator to supervise bather safety and maintain surveillance over bathers while they are on the deck or in the pool. Owner: The person or corporation who is the owner of an aquatic facility. Operator: The trained individual designated by the owner to be responsible for the day-to-day operation of an aquatic facility. Supervised Waterfront: A waterfront is an outdoor, artificial or natural shoreline alongside a body of water, that may include docks or piers, that may be used for aquatic activities such as swimming, wading, diving, or aquatic sports. A supervised waterfront is a waterfront that provides lifeguards/beach patrol as part of its operation. Rationale Lifeguards who supervise waterfront areas should have equipment that allows them to effectively supervise the designated area and respond appropriately in emergency situations. Implementation The following equipment should be available and present at all times, in good working order, checked daily for breakdowns or faults, and easily accessible in case of an emergency: Lifeguard uniforms readily identified as such. -

Aquatic Leadership
Aquatic Leadership Looking for an exciting and rewarding job? Join our team by taking the leadership courses listed below: Swim Patrol: Rookie, Ranger Star Bronze Star pg. 58 pg. 58 8-12 years of age* Swim Patrol experience recommended* Steps to Becoming a Steps to Becoming a Lifeguard Swimming Instructor Important Swimming Info Bronze Medallion Red Cross Water Safety pg. 58 & Emergency First Aid (EFA) pg. 58 Instructor (WSI) Prerequisite: 13 years of age or Bronze Prerequisite: 15 years of age, Bronze What to Wear in the Pool Shower Before Swimming Star Cross and Emergency First Aid LEADERSHIP Proper bathing attire means clothing used for All swimmers must shower thoroughly before swimming only. Children who are not toilet- entering the pool to help keep the water clean for trained must wear swimmer pull-ups. NO your swimming enjoyment. and/or DIAPERS, disposable or cloth, are permitted. Change Room Requirements Bronze Cross & Standard First Lifesaving Society Lifesaving Slide & Therapy Pool Information Children six years of age or older are required to pg. 58 Aid (SFA) Summer Instructor (LSI) The two-storey water slide enters into the use the change room of their own gender. If this Prerequisite: Bronze Medallion & EFA 2019 Prerequisite: 16 years of age and Bronze Therapy Pool and is 90 feet in length. The slide is not suitable or you are not able to accompany Cross operates during public swim times, except where your child into their gender-specific change room, noted otherwise. Must be 48” tall to ride. please make use of the family/special needs change room. -

Explore the New Bronze Med Al a W Ards
What’s new for Affiliates? The Lifesaving Society has updated its Bronze medal awards: • To reflect the Society’s current research into drowning in Canada including the incidence and consequences of non-fatal drowning. • To focus on the core areas of competency in water rescue: skills, knowledge, fitness and judgment. • To improve skill progressions for a logical and seamless flow into National Lifeguard. • To set candidates up for success as they move through the Society’s lifesaving, assistant lifeguard, and lifeguard continuum. Key changes • Bronze Star content focuses on swimming proficiency, lifesaving skill and personal fitness. • Bronze Medallion includes swimming strokes in the curriculum. • Bronze Cross contains fundamental lifeguarding skills and concepts needed by those responsible for safety supervision. • First aid items are restricted to content that relates directly to water rescue. Drowning resuscitation remains the central focus throughout the Bronze medal awards. • Standardization of Bronze Medallion and Bronze Cross recertification exams. Strokes are back – by popular demand: We heard loud and clear from parents, instructors, and affiliates that young swimmers need opportunities to continue to develop their swim strokes in lifesaving classes. In the new Bronze Star and Bronze Medallion, participants will hone front and back crawl, breaststroke and lifesaving kicks. Bronze Cross is assistant lifeguard training: Now more than ever, the new Bronze Cross prepares candidates for responsibilities as assistant lifeguards. Bronze Cross features more lifeguarding content with an emphasis on the principles and techniques of active surveillance (including scanning) in aquatic facilities. Candidate assessment includes Assistant Lifeguard Situations. First aid focused on water rescue: The Bronze medal awards emphasize aquatic-related first aid and resuscitation skills. -
United States Lifeguarding Standards Coalition
United States Lifeguard Standards Page 2 of 67 January 2011 ACKNOWLEDGMENTS Sincere appreciation is extended to all of the individuals who dedicated their time and expertise to the development of the first outcomes and recommendations of the United States Lifeguard Standards Coalition. Special thanks is extended to the National Swimming Pool Foundation, Colorado Springs, Co., for the generous donation that funded this project. The contributions and commitment to excellence by all involved made this project possible. United States Lifeguard Standards Page 3 of 67 January 2011 CONTENTS INTRODUCTION The Problem History of Collaboration Establishment of the Coalition Participants and Responsibilities Scope of the Process PROCESS AND METHODOLOGY Evidence-Based Process Scientific Review and Evidence Grading Review Process EVIDENCE EVALUATIONS: THE QUESTIONS Scanning Techniques Vigilance Inattentional Blindness Visual and Behavioral Cues Breaks (Interruptions of Duty) Age Hearing Vision Physical Competency Use of Equipment Airway Suction Cervical Spine Injury Oxygen Online Learning REFERENCES United States Lifeguard Standards Page 4 of 67 January 2011 Abbreviations ABC Airway, breathing, and circulation AED Automated external defibrillator AHA American Heart Association ARC American Red Cross BLS Basic life support CI Confidence interval COI Conflict of interest CoSTR Consensus on Resuscitation Science and Treatment Recommendations CPR Cardiopulmonary resuscitation EMS Emergency medical systems EMT Emergency medical technician ILCOR International