United States Lifeguarding Standards Coalition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
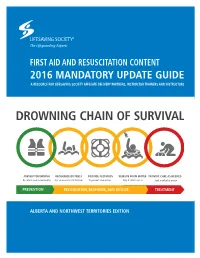
Drowning Chain of Survival
FIRST AID AND RESUSCITATION CONTENT 2016 MANDATORY UPDATE GUIDE A RESOURCE FOR LIFESAVING SOCIETY AFFILIATE DELIVERY PARTNERS, INSTRUCTOR TRAINERS AND INSTRUCTORS DROWNING CHAIN OF SURVIVAL PREVENT DROWNING RECOGNIZE DISTRESS PROVIDE FLOTATION REMOVE FROM WATER PROVIDE CARE AS NEEDED Be safe in and around water Ask someone to call for help To prevent submersion Only if safe to do so Seek medical attention PREVENTION RECOGNITION, RESPONSE, AND RESCUE TREATMENT ALBERTA AND NORTHWEST TERRITORIES EDITION FIRST AID AND RESUSCITATION CONTENT 2016 MANDATORY UPDATE GUIDE FIRST AID AND RESUSCITATION CONTENT 2016 MANDATORY UPDATE GUIDE A RESOURCE FOR LIFESAVING SOCIETY AFFILIATE DELIVERY A RESOURCE FOR Lifesaving SOCIETY AFFILIATE delivery partners, PARTNERS, INSTRUCTOR TRAINERS AND INSTRUCTORS instructor TRAINERS AND instructors Published by the Lifesaving Society, First Printing December 2018 _____________________________________________________________ Copyright 2016 by the Royal Life Saving Society Canada. Reproduction, by any means, of materials contained in this book is prohibited unless authorized by the publisher. Requests should be directed to the Alberta and Northwest Territories office (see back cover for contact information). The Lifesaving Society is Canada’s lifeguarding expert. The Society works to prevent drowning and water-related injury through its training programs, Water Smart® public education initiatives, water-incident research, aquatic safety management services, and lifesaving sport. Annually, well over 1,200,000 Canadians participate in the Society’s swimming, lifesaving, lifeguard, and leadership training programs. The Society sets the standard for aquatic safety in Canada and certifies Canada’s National Lifeguards. The Society is an independent, charitable organization educating Canadian lifesavers since the first Lifesaving Society Bronze Medallion Award was earned in 1896. -

A Guide to Coastal Public Rescue Equipment Contents
Version 1: 2007 A guide to coastal public rescue equipment Contents Foreword 3 Acknowledgements 4 Preface 5 Introduction 7 How this guide was researched 8 Getting started 10 How to use this document 13 Understanding coastal environments 14 Understanding beaches 16 Understanding rocky coasts 19 Understanding tidal inlets and estuaries 20 Understanding man-made coasts 21 Risk management for PRE 22 Selecting public rescue equipment 24 PRE for beaches 26 PRE for rocky coasts, tidal inlets and estuaries 28 PRE for man-made coasts 30 Emergency communications 32 Locating PRE and communications 34 Additional information 40 Signs and user information 42 PRE housing 44 Maintenance 46 Reducing vandalism 47 Useful reading 48 Inside back cover Useful contacts Foreword With the UK having some of Europe’s finest beaches, This guide is the first of its kind, not only in the UK, and with increasing access to other parts of the coast, but worldwide. With credible and robust research, it is unsurprising that millions of people enjoy the UK this guide is in a position to set a world benchmark coastline every year. However, with an increasing trend for coastal public rescue equipment. for recreational activity on our beaches and inshore waters, UK maritime rescue services have never been We therefore welcome and fully endorse this guide so busy helping people in difficulty. and commend all those that were involved in making it happen. Therefore, we are delighted that the RNLI, working closely with members of the National Water Safety Michael Vlasto OBE Forum and other safety organisations, has produced Chairman, National Water Safety Forum this guide for coastal public rescue equipment (PRE): Operations Director, Royal National Lifeboat Institution guidance that beach operators have requested to help manage their beaches safely. -

National Lifeguard
National Lifeguard - Pool Option The primary role of the National Lifeguard is the prevention of emergency situations and the timely and effective resolution of emergencies. The National Lifeguard certification prepares lifeguards to fulfill this role as professional facilitators of safe, enjoyable aquatics in a pool setting. The National Lifeguard program develops the basic lifeguarding skills, principles, and decision‐making process to help lifeguards evaluate and adapt to different aquatic facilities and emergencies. Pre‐requisite: Bronze Cross, Standard First Aid and a minimum of 16 years of age. April 20‐22 & 27‐29, 2018 Fri 4‐9 PM Sat & Sun 8:00 AM – 4:30 PM Taber Aquafun Centre Cost: $351.75 For more information, please contact the Aquafun Centre. (403)223‐5544 ext.3 _________________________________________________________________________________________ Red Cross Water Safety Instructor Course The Water Safety Instructor (WSI) Course prepares candidates to instruct the Red Cross Swim programs. Candidates focus on strategies to introduce and develop fitness activities, skills and water safety, and swimming skills in the Red Cross Swim Preschool, Red Cross Swim Kids, Red Cross Swim @ School, Red Cross Swim @ Camp, Red Cross Swim for Adults & Teens, and Red Cross Swim Adapted programs. Pre-course Requirements:15 years or older by the last day of the WSI - Classroom and Pool, ability to perform Red Cross Swim Kids 10 strokes and skills, and hold one of the following certifications (not required to be current): Red Cross Assistant Lifeguard, Emergency First Aid or equivalent. Course Components, Length & Dates: May 12, 5-10 PM —Introduction & Skills Evaluation* – 5 hours, To be completed before teaching experience—Online – 14–20 hours Teaching hours to be arranged for lessons during summer sessions—min. -

Aquatic Certifications for NYS Bathing Facilities (Fact Sheet)
AQUATIC CERTIFICATIONS for NYS Bathing Facilities Fact Sheet – April 2021 (Go to www.health.ny.gov to view most current certification list) Standards for aquatic/lifeguard certifications are contained in New York State Sanitary Codes (SSC) Subpart 6-1, Section 6-1.31, Swimming Pools; Subpart 6-2, Section 6-2.20, Bathing Beaches; and Subpart 7-2, Section 7-2.5(g), Children’s Camps. When the SSC requires "lifeguard supervision" or a "qualified lifeguard" at a bathing facility, an approved lifeguard certification SPECIFIC to the type of bathing facility is required. NOTE: • All lifeguards must possess separate cardiopulmonary resuscitation (CPR) certification in an approved course listed on the NYS CPR fact sheet unless otherwise indicated in the below table. All CPR certificates are valid for 1 year from course completion, regardless of the expiration date noted on the card. • Lifeguard certifications shall be valid for the time period specified by the certifying agency, but may not exceed a con secutive 3-year period from course completion. Multiyear lifeguard certifications that include CPR require a CPR certification each year. • Children's camp lifeguards must be at least 17 years of age, except; − A maximum of 50% of the required lifeguards on duty may be 16 years of age; − Lifeguards for wilderness swimming must be at least 18 years of age. • Supervising lifeguards must possess at least Supervision Level IIb certification, be at least 18 years old, and have at least 2 seasons of lifeguarding experience. ACCEPTED COURSES SUPERVISION LEVEL Marked boxes indicate acceptability Level II b Level I Pool & Level II a PROVIDER CERTIFICATION TITLE Surf Pool Only Beach American Red Cross (ARC) Lifeguarding/First Aid/CPR/AED* X LIFEGUARDING AND FIRST AID CERTIFICATIONS ARE Lifeguarding, Waterpark Skills/First Aid/CPR/ X VALID FOR 2 YEARS FROM DATE OF ISSUANCE. -

A Lifeguard's Beach Safety Tips
A Lifeguard’s Beach Safety Tips by Sgt. Ed Fisher Special to the Dispatch The writer is a 17-year veteran of the Beach patrol. In the off-season, he is an elementary school teacher in Montgomery County. The OCBP consist of over 200 men and women dedicated to ocean rescue and maintaining a safe and orderly environment on Ocean City’s beach. The Sure Rescue Technicians guard the beach seven days a week from 10 a.m. – 5:30 p.m. Studying the waves helps safety September 12, 2008 The Dispatch/Maryland Coast Dispatch Recently a kite surfer tried surfing in a hurricane and ended up getting blown into the side of a building. An accident like this does not happen because of bad luck. An accident like this happens because of poor decision making, not knowing your sport, and not respecting the elements. I mean is it really surprising that a kite that was flying in a hurricane got out of control? The idea here is that everyone entering the surf should have more common sense than this and take some basic precautions. The first precaution begins on the beach. People should spend at least 15 minutes on the beach surveying the conditions. Often people come out to the beach and see a calm ocean. As soon as they attempt to swim they find themselves confronted with a dangerous set of waves or strong currents they were not aware of. Be sure to know what the conditions are before entering the water. The daily conditions of the ocean are governed by the swell direction, wind velocity, and ocean bottom. -
Lifeguard Effectiveness: a Report of the Working Group
Lifeguard Effectiveness: A Report of the Working Group Editors: Christine M. Branche, Ph.D. Steven Stewart, M.S. Division of Unintentional Injury Prevention National Center for Injury Prevention and Control Centers for Disease Control and Prevention Department of Health and Human Services Lifeguard Effectiveness: A Report of the Working Group is a publication of the National Center for Injury Prevention and the Centers for Disease Control and Prevention Centers for Disease Control and Prevention Jeffrey P. Koplan, M.D., M.P.H., Director National Center for Injury Prevention and Control Sue Binder, M.D., Director Division of Unintentional Injury Prevention Christine M. Branche, Ph.D., Director Production services were provided by staff of the Management Analysis and Services Office, CDC. Suggested Citation: Branche CM, Stewart S. (Editors). Lifeguard Effectiveness: A Report of the Working Group. Atlanta: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2001. ii Lifeguard Effectiveness: A Report of the Working Group Table of Contents Contributing Authors ................................................................................................................... v Executive Summary.................................................................................................................... vii Introduction................................................................................................................................... 1 A Brief History and Background of Lifeguarding -

Lps 07 Fitness Testing for Lifeguards
World Water Safety INTERNATIONAL LIFE SAVING FEDERATION Gemeenteplein 26 – 3010 Leuven – Belgium Tel: (32.16) 89.60.60 – E-mail: [email protected] - Web: www.ilsf.org LIFESAVING POSITION STATEMENT - LPS 07 FITNESS TESTING FOR LIFEGUARDS NOTE: This statement is intended for those lifeguards, acting in a professional or volunteer capacity, who are trained in the techniques of water rescue and resuscitation and who assume a duty to safeguard members of the public at aquatic sites. They may be called lifeguards, lifesavers or both. This statement is not directed at members of the public trained in water safety and rescue techniques, but without a duty to respond, who may also be known, in some areas of the world, as lifesavers. The standards outlined in this position statement are the minimum that ILS recommends. ILS encourages organisations to exceed these recommended minimum standards where local conditions and/or expectations of lifeguards are warranted. BACKGROUND Experts in the field of lifeguard training and rescue believe that lifeguards need to be able to demonstrate a reasonable level of fitness. It is presumed that lifeguards would have sound swimming and water rescue skills. The ability for lifeguards to swim a specified distance within a defined amount of time has been shown to correlate. The available English language studies in the aquatic setting were reviewed. The data is cohort studies of lifeguard pre-employment assessment outcomes. Level of evidence from the research is low and not directly related to the question addressed in this review. There are no direct outcome data for lifeguards responding to victims. -

Supervised Waterfront Operations Equipment
Lifesaving Society Canada Suite 001 – 1145 Hunt Club Road, Ottawa, Ontario K1V 0Y3 Telephone: 613-746-5694 E-mail: [email protected] Web: www.lifesaving.ca Safety Standards for Canadian Swimming Pools and Waterfronts Waterfront Standard Supervised Waterfront Operations Equipment Standard Standard Owners and Operators of supervised waterfronts should ensure that appropriate equipment is available at all times for use by lifeguards on duty. Definitions Last seen marker: A small buoy with a line and anchor that is used to mark the location where a person was last seen in the water. Lifeguard: A person with a current National Lifeguard certification appointed by the owner or operator to supervise bather safety and maintain surveillance over bathers while they are on the deck or in the pool. Owner: The person or corporation who is the owner of an aquatic facility. Operator: The trained individual designated by the owner to be responsible for the day-to-day operation of an aquatic facility. Supervised Waterfront: A waterfront is an outdoor, artificial or natural shoreline alongside a body of water, that may include docks or piers, that may be used for aquatic activities such as swimming, wading, diving, or aquatic sports. A supervised waterfront is a waterfront that provides lifeguards/beach patrol as part of its operation. Rationale Lifeguards who supervise waterfront areas should have equipment that allows them to effectively supervise the designated area and respond appropriately in emergency situations. Implementation The following equipment should be available and present at all times, in good working order, checked daily for breakdowns or faults, and easily accessible in case of an emergency: Lifeguard uniforms readily identified as such. -

Aquatic Leadership
Aquatic Leadership Looking for an exciting and rewarding job? Join our team by taking the leadership courses listed below: Swim Patrol: Rookie, Ranger Star Bronze Star pg. 58 pg. 58 8-12 years of age* Swim Patrol experience recommended* Steps to Becoming a Steps to Becoming a Lifeguard Swimming Instructor Important Swimming Info Bronze Medallion Red Cross Water Safety pg. 58 & Emergency First Aid (EFA) pg. 58 Instructor (WSI) Prerequisite: 13 years of age or Bronze Prerequisite: 15 years of age, Bronze What to Wear in the Pool Shower Before Swimming Star Cross and Emergency First Aid LEADERSHIP Proper bathing attire means clothing used for All swimmers must shower thoroughly before swimming only. Children who are not toilet- entering the pool to help keep the water clean for trained must wear swimmer pull-ups. NO your swimming enjoyment. and/or DIAPERS, disposable or cloth, are permitted. Change Room Requirements Bronze Cross & Standard First Lifesaving Society Lifesaving Slide & Therapy Pool Information Children six years of age or older are required to pg. 58 Aid (SFA) Summer Instructor (LSI) The two-storey water slide enters into the use the change room of their own gender. If this Prerequisite: Bronze Medallion & EFA 2019 Prerequisite: 16 years of age and Bronze Therapy Pool and is 90 feet in length. The slide is not suitable or you are not able to accompany Cross operates during public swim times, except where your child into their gender-specific change room, noted otherwise. Must be 48” tall to ride. please make use of the family/special needs change room. -

Surf Lifeguard Training Manual
Surf Lifeguard Training Manual 2017 Begin In 1910 Surf Lifeguards began providing beach patrols. It wasn’t just about making our beaches safer, it was about the increasing popularity of our beaches for recreation. There has been a lot of change in the last 100 years and today Surf Life Saving is about more than just patrolling between the flags. Coastal development has opened up new beaches and new walk ways lead people to different parts of our beaches today. Windsurfers, surfing, boogie boards – even wetsuits which we take for granted today, have all had a significant impact on when and how people use our beaches. Today we provide patrols at more than 80 of New Zealand’s most popular beaches, but it’s just part of what we do. Public education, event safety services, search and rescue and working with councils to ensure effective and consistent signage are all part of our Lifesaving plan to achieve our purpose. Membership Today there are nearly 18,000 members across 74 Clubs. Each year more than 800 new Lifeguards are qualified. Behind every Lifeguard, a coach, an instructor, and committee members all have an important role to play. The oppurtunities available to you as a member of a surf lifesaving club are extraordinary. Once you have your Lifeguard Award, you can advance through the lifeguard programme in which ever direction you choose – First Aid, Inflatable Rescue Boat (IRB), Lifeguard development. You are also able to participate in our sport programme and put your skills on the line against others – be it beach sprints, swimming, surf boats or IRBs. -
Lifesaving Standard Operating Procedures
STANDARD OPERATING PROCEDURES Lifesaving Services Version 6, December 2019 Signature of Endorsement – December 2019 Steven Pearce AFSM Chief Executive Officer Surf Life Saving New South Wales Australian Lifeguard Services (NSW) Joel Wiseman Director of Lifesaving Surf Life Saving New South Wales The registered office of Surf Life Saving NSW is situated at the 3 Narabang Way, Belrose NSW 2085 Australia. ABN 93 827 748 379. © 2019 Surf Life Saving New South Wales (SLSNSW). This publication is copyright. Apart from any fair dealing for the purposes of private study, research, criticism or review as permitted under the Copyright Act, no part may be reproduced by any process without the written permission of SLSNSW.” Whilst all care has been taken in the preparation of this publication, no responsibility is accepted by the authors or SLSNSW for any errors, omissions or inaccuracies. The information in this publication is current as at 1 December 2019. The publication is of a general nature only and is not intended to be relied upon nor as a substitute for detailed professional advice. No responsibility can be accepted by the authors or SLSNSW for loss occasioned to any person as a result of the material in this publication. STANDARD OPERATING PROCEDURES LIFESAVING SERVICES V.6 | 1 FOREWORD Date: December 2019 Dear All, It is with pleasure that I present you with the SLSNSW Standard Operating Procedures – Version 6 (2019). This manual outlines policies, procedures and guidelines to assist lifesaving services in the management and delivery of their operations as a capable aquatic rescue organisation, prepared to meet our future challenges. -

Lifesaving South Africa Patrol Guidelines 2020
PATROL GUIDELINES - 2020 LIFESAVING SOUTH AFRICA PATROL GUIDELINES 2020 www.lifesaving.co.za www.lifesaving.co.za LIFESAVING SOUTH AFRICA LIFESAVING SA GUIDELINES FOR PATROL’S A Patrollers primary duty is to ensure the safety of persons within an area which has been deemed safe for public swimming. All communities have an expectation of safe water use. LSA has a responsibility to meet the challenge of this expectation by patrolling and supplying a lifesaving service, and administering first aid as required. Members joining the association need to be made aware of their responsibility in the maintaining efficient duties. Your knowledge of rescue techniques and the training in these skills will ensure safe bathing for the community. In addition, lifeguards must act as good ambassadors for the Association. All members required to do duty in a club should be allocated into squads so that everyone is aware of when it is their turn to protect the bathers. At the head of each squad is the Squad Leader. He should be a responsible, experienced lifeguard who can control the aquatic facility, beach, pool, open water or leisure park facility, and deal with people, both public and squad members. He controls the allocation of the squad members to their duties. The safe swimming area must be carefully checked by the duty squad for possible danger spots; once a safe area has been identified clear bathing signs must be displayed. The size of the safe swimming area depends on the duty squad, number of swimmers and the environment PATROL ACTIVITIES Various patrol activities may be employed in the efforts to ensure the safety of the swimmers: Traditional method: Between the red and yellow flags This is the most common type of patrol and simply requires the setting of the flags at the safest place on the beach.