How to Choose a Neurosurgeon: Discussion with Dr. Henry Brem
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
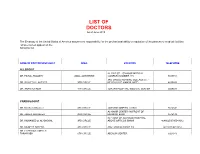
LIST of DOCTORS As of June 2018
LIST OF DOCTORS As of June 2018 The Embassy of the United States of America assumes no responsibility for the professional ability or reputation of the persons or medical facilities whose names appear on the following list. NAME OF DOCTOR/SPECIALIST AREA LOCATION TELEPHONE ALLERGIST AL-RAZI ST. - SAMOOR MEDICAL DR. FAISAL TBAILEH JABAL ALHUSSEIN COMPLEX NUMBER 145 5695151 3RD CIRCLE NURSING COLLAGE ST. - DR. SAYYED AL-NATHER 3RD CIRCLE NEAR HAYAT AMMAN HOTEL 4655893 DR. ANAN ALFAQIH 4TH CIRCLE JORDAN HOSPITAL/ MEDICAL CENTER 5609031 CARDIOLOGIST DR. Munther AlSaafeen 4TH CIRCLE JORDAN HOSPITAL CLINIC 5624840 AL-KHAIR CENTER- IN FRONT OF DR. ZAHER ALKASEEH 3RD CIRCLE HOUSING BANK 4645138 IN FRONT OF ALKHALDI HOSPITAL, DR. MOHAMED O. AL-BAGGAL 3RD CIRCLE ABOVE OPTICOS SHAMI 4646625/0795543012 DR. MUNEER AREEDA 4TH CIRCLE ABU HASSAN COMPLEX 4613613/4613614 DR. HATEM SALAMEH AL- TARAWNEH 5TH CIRCLE ABDOUN CENTER 5924343 DR. AHMAD MOHANNA AL ABDOUN CENTER, INFRONT OF ARABIC HARASEES 5TH CIRCLE CENTER 5924343 DR. IMAD HADAD 4TH CIRCLE JORDAN HOSPITAL CLINIC 5626197/0795303502 DR. NAZIH NAJEH AL-QADIRI 4TH CIRCLE JORDAN HOSPITAL CLINIC 5680060/0796999695 JABER IBN HAYYAN ST./ IBN HAYYAN DR. SUHEIL HAMMOUDEH SHMEISANI MEDICAL COMPLEX 5687484/0795534966 DR. YOUSEF QOUSOUS JABAL AMMAN AL-KHALIDI ST./ AL- BAYROUNI COMP. 4650888/0795599388 CARDIOVASCULAR SURGEON JABAL AMMAN NEAR ALKHALDI DR. SUHEIL SALEH 3RD CIRCLE HOSPITAL 4655772 / 079-5533855 COLORECTAL & GENERAL SURGERY DR. WAIL FATAYER KHALIDI HOSPITAL RAJA CENTER 5TH FLOOR 4633398 / 079-5525090 AL- RYAD COMP.BLDG NO. 41/ FLOOR DR. MARWAN S. RUSAN KHALIDI HOSPITAL ST. GROUND 4655772 / 0795530049 DR. JAMAL ARDAH TLA' AL- ALI IBN AL-HAYTHAM HOSPITAL 5602780 / 5811911 DENTISTS DENTAL CONSULTATION CENTER MAKA ST. -
Partnering with Your Transplant Team the Patient’S Guide to Transplantation
Partnering With Your Transplant Team The Patient’s Guide to Transplantation U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Health Resources and Services Administration This booklet was prepared for the Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation by the United Network for Organ Sharing (UNOS). PARTNERING WITH YOUR TRANSPLANT TEAM THE PATIENT’S GUIDE TO TRANSPLANTATION U.S. Department of Health and Human Services Health Resources and Services Administration Public Domain Notice All material appearing in this document, with the exception of AHA’s The Patient Care Partnership: Understanding Expectations, Rights and Responsibilities, is in the public domain and may be reproduced without permission from HRSA. Citation of the source is appreciated. Recommended Citation U.S. Department of Health and Human Services (2008). Partnering With Your Transplant Team: The Patient’s Guide to Transplantation. Rockville, MD: Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation. DEDICATION This book is dedicated to organ donors and their families. Their decision to donate has given hundreds of thousands of patients a second chance at life. CONTENTS Page INTRODUCTION.........................................................................................................................1 THE TRANSPLANT EXPERIENCE .........................................................................................3 The Transplant Team .......................................................................................................................4 -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

100 Years. 100 Facts
100 Years. 100 Facts. Celebrating 100 Years as the United Voice of Ohio Hospitals 1819 Daniel Drake obtains a charter for the Medical 001 College of Ohio, the forerunner of the University of Cincinnati College of Medicine. 100 Years. 100 Facts. | 3 1823 Ohio’s first hospital, the Cincinnati Commercial 002 Hospital and Lunatic Asylum, opens. 4 | Ohio Hospital Association 100 Years. 100 Facts. | 5 Starling Medical Center College/Saint 003 Francis Hospital is established on the 1849 present site of Grant Medical Center in Columbus as the first teaching hospital in the U.S. It is the forerunner for the College of Medicine at Ohio State University. 6 | Ohio Hospital Association Charity Hospital Medical Center, now 004 St. Vincent Charity Hospital, opens 1873 Cleveland’s first amphitheater for demonstration of surgery and clinical procedures. 100 Years. 100 Facts. | 7 8 | Ohio Hospital Association 1886 Mother M. Angela and Sister M. Rufina Dunn, of the 005 Congregation of the Sisters of the Holy Cross of Notre Dame, Indiana, convert a sturdy four-story red brick building to two wards, 18 private rooms and an operating room with an amphitheater. The facility is called Hawkes Hospital of Mount Carmel and eventually becomes Mount Carmel West. 100 Years. 100 Facts. | 9 A 10-bed Christ Hospital opens in 006 Cincinnati after a group of local 1889 businessmen led by James Gamble (whose prospering soap business eventually became Procter & Gamble) invited Isabella Thornburg to the city in 1888 to train deaconesses and missionaries. She soon expands beyond training to open a hospital in the west end of the city. -
Go Inside a Surgeon's Typical
HealthSigns Spring 2016 Go Inside a Surgeon’s Typical Day Top in Cancer Getting the Planet Friendly Care Picture Healthcare Earning kudos on quality More advanced imaging How we care for patients for nearly a decade tools in your community and the environment HealthSigns Spring 2016 5 10 Sustaining Going Quality Green Cancer program We’re leading the earns top national way to a healthier, award for third more sustainable time. environment. 6 11 Focused on Parking Garage Healing Near Opening General surgeon More convenient starts each day access helps with energy and patients, families endurance. and our community. 8 Easy Access to Imaging Outpatient center VISIT US ONLINE offers screenings, Stay connected to Washington Hospital at www.whhs.com diagnostics and and on Facebook. Browse our calendar of upcoming events and treatment. other happenings taking place at your community hospital. 2 | SPRING 2016 Information You Can Use MISSION STATEMENT Free, science-based diabetes education classes for people with diabetes and their families or anyone who wants to As the local Health Care District, find out more about this chronic disease affecting more our mission is to meet the than 29 million Americans. health care needs of the District Diabetes Matters residents through medical services, education and research. When: First Thursday of every month (except for July), 7 to 8 p.m. Within this scope, Washington Stay for the Diabetes Support Township Health Care District Group, 8 to 9 p.m. is committed to assuming the Location: Conrad E. Anderson, MD, Auditorium (Washington West) leadership role in improving and 2500 Mowry Ave., Fremont maintaining the health status of No registration needed. -

14 Glossary of Healthcare Terms
Premera Reference Manual Premera Blue Cross 1144 GGlloossssaarryy ooff HHeeaalltthhccaarree TTeerrmmss A Accreditation: Health plan accreditation is a rigorous, comprehensive and transparent evaluation process through which the quality of the systems, processes and results that define a health plan are assessed. Acute: A condition that begins suddenly and does not last very long (e.g., broken arm). ‘acute” is the opposite of “chronic.” Acute Care: Treatment for a short-term or episodic illness or health problem. Adequacy: The extent to which a network offers the appropriate types and numbers of providers in a designated geographic distribution according to the relative availability of such providers in the area and the needs of the plan's members. Adjudication: The process of handling and paying claims. Also see Claim. Admission Notification: Hospitals routinely notify Premera of all inpatient admissions that link members to other care coordination programs, such as readmission prevention. The process includes verification of benefits and assesses any need for case management. Advance Directives: Written instructions that describe a member’s healthcare decision regarding treatment in the event of a serious medical condition which prevents the member from communicating with his/her physician; also called Living Wills. Allied Health Personnel: Specially trained and licensed (when necessary) healthcare workers other than physicians, optometrists, dentists, chiropractors, podiatrists, and nurses. Allowable: An amount agreed upon by the carrier and the practitioner as payment for covered services. Alpha Prefix: Three characters preceding the subscriber identification number on Blue Cross and/or Blue Shield plan ID cards. The alpha prefix identifies the member’s Blue Cross and/or Blue Shield plan or national account and is required for routing claims. -

Neurology and Neurosurgery
NYU Langone Medical Center 550 First Avenue, New York, NY 10016 nyulmc.org NEUROLOGY AND NEUROSURGERY 2014 YEAR IN REVIEW CONTENTS 1 Message from the Chairs 2 Facts & Figures 4 New & Noteworthy 8 Clinical Care 9 Cerebrovascular Surgery 24 Multiple Sclerosis Center 12 Stroke Center 26 Parkinson’s and Movement 13 Neuro ICU Disorders Center 14 Brain Tumor Center 28 Neuromodulation 16 Center for Advanced 30 Center for Cognitive Neurology Radiosurgery 32 Pediatrics 18 Concussion Center 34 Neurogenetics 19 Neuro-Ophthalmology 36 Neuromuscular 20 Comprehensive Epilepsy Center 37 Dysautonomia Center 23 Neurophysiology 38 Spine and Peripheral Nerve 23 Neuropsychology 39 General Neurology and Neuropsychiatry 40 Research 42 Education & Training 46 Publications Design: Ideas On Purpose, www.ideasonpurpose.com 51 Leadership Produced by: Office of Communications and Marketing, NYU Langone Medical Center NYU LANGONE MEDICAL CENTER / NEUROLOGY AND NEUROSURGERY / 2014 PAGE 1 MESSAGE FROM THE CHAIRS Dear Colleagues and Friends, We are pleased to present this inaugural annual report from the Departments of Neurology and Neurosurgery at NYU Langone Medical Center. This publication marks a time of significant growth for our departments: Patient volume has risen steadily, we have added stellar faculty members in key strategic areas, and our research and educational programs continue to expand. Today, all of our subspecialties are staffed by physician leaders, including many nationally and internationally recognized clinicians and researchers. Our divisions include one of the largest, most sophisticated epilepsy centers in the nation; the leading brain, skull-base, and cerebrovascular surgery programs in the New York area; nationally known centers for the treatment of multiple STEVEN L. -

The Impaired Surgeon
The Impaired Surgeon Ranjan Sudan, MD*, Keri Seymour, DO KEYWORDS Impaired Physician Alcohol Drugs KEY POINTS Impaired physicians commonly refers to those who suffer from substance use disorders (SUDs). The annual prevalence is approximately 10% to 12%. Treatment is available through physician health programs (PHPs). Prognosis for recovery and preservation of the ability to practice medicine are excellent for more than 70% of the participants. BACKGROUND According to the American Medical Association (AMA), an impaired physician is one whose physical or mental health interferes with their ability to engage safely in profes- sional activities.1 Such impairment can be the result of a substance use disorder (SUD), mental health issues, or physical health problems. Although by this definition “physician impairment” can be used broadly, it is more commonly used to describe a physician who has a SUD and is the focus of this article. Previously, substance abuse and substance dependence were 2 separate diag- nostic categories. The Diagnostic and Statistical Manual of Mental Disorders (Fifth Edi- tion), however, combined them into a single disorder that is measured on a continuum from mild to severe, and each specific substance use is addressed separately (eg, alcohol use disorder). To diagnose SUDs, 11 symptoms are assessed that relate to impaired control, social impairment, risky use, and pharmacologic criteria, such as tolerance and withdrawal. In general, a mild SUD is suggested by the presence of 2 to 3 symptoms, moderate by 4 to 5 symptoms, and severe by 6 or more symptoms. These include taking the substance in larger amounts and for longer period than intended; wanting to cut down or stop using the substance but not being able to; spending a lot of time getting or recovering from use of the substance; craving and urges to use the substance; not keeping up with work or school because of substance Disclosure Statement: The authors have nothing to disclose. -
Introducing Ophthalmology
introducing ophthalmology a p r i m e r for off ice st a f f Third Edition 655 Beach Street P.O. Box 7424 San Francisco, CA 94120-7424 introducing ophthalmology: a primer for office staff ophthalmology liaisons committee academy staff Samuel P. Solish, MD, Chair Richard A. Zorab, Vice President, Richard C. Allen, MD, PhD Ophthalmic Knowledge Amy S. Chomsky, MD Hal Straus, Director of Print Publications JoAnn A. Giaconi, MD Susan R. Keller, Acquisitions Editor Humeyra Karacal, MD Kimberly A. Torgerson, Publications Editor Martha P. Schatz, MD D. Jean Ray, Production Manager John Michael Williams Sr, MD Debra Marchi, CCOA, Administrative Assistant Kyle Arnoldi-Jolley, CO, COMT Annquinetta F. Dansby-Kelly, RN, CRNO Diana J. Shamis, COMT © 2013 American Academy of Ophthalmology All rights reserved. ii Preface iv contents 1 IntroductIon to oPhthalmology 1 2 d how oes the eye work? 7 3 d why o we need eyeglasses? 15 4 t wha can go wrong wIth the eye? 22 5 m the edIcal eye examInatIon 33 6 offIce etIquette and ethIcs 40 glossary 47 common oPhthalmIc abbrevIatIons 51 suggested resources 54 Chinese spectacles with tangerine skin case, ca 1780 (Courtesy Museum of Vision, Foundation of the American Academy of Ophthalmology) iii preface This edition of Introducing Ophthalmology: A Primer for Office Staff has been reviewed for currency, updated, and converted to a digital format. The primary audience for this book is new office staff who need understanding of basic concepts in ophthalmology. New office staff will gain insights into the eye health terms and concepts they encounter. -

What Is a Surgical Resident? for the Patient: a Guide to Surgical Training and the Professionals Who Will Take Care of You
What is a surgical resident? For the patient: A guide to surgical training and the professionals who will take care of you Attending Chief Resident The attending surgeon has finished all Chief residents are in their final year of training and is fully qualified in surgery. residency training. Chief residents may be The attending is in charge of your surgical just months away from being in practice care and supervises the team that takes care on their own. They will have participated of you. This team includes residents, medical in many hundreds of operations by the students, and other health professionals. time they finish residency. Because of The attending is in charge of training the their experience and time in training, chief residents, and of making sure that graduating residents lead the team of residents and residents are fully prepared to perform make many decisions. surgery on their own. While the residents and medical students may rotate on and off the team, an attending surgeon will always be responsible for managing your care. Surgical Training: The Team Over the course of your surgical experience, a team of many individuals will be contributing to your care. Trainees—medical students and residents— may be part of that team. We want you and your family to understand who is helping with your surgical care and the role each Resident person plays. Medical Student Residents are doctors who have completed Medical students have completed a four-year medical school. Residents are training in a college degree and are enrolled in medical surgical specialty. Surgical residency lasts school, which lasts four years. -

Should Trauma Surgeons Perform Neurosurgery in Emergencies?
Commentary 87 Should Trauma Surgeons Perform Neurosurgery in Emergencies? Paritosh Pandey1 1Consultant Neurosurgeon, Manipal Hospitals, Bengaluru, Address for correspondence Paritosh Pandey, Consultant Karnataka, India Neurosurgeon, Manipal Hospitals, 98, HAL Old Airport Rd, Kodihalli, Bengaluru, Karnataka 560017, India (e-mail: [email protected]). Indian J Neurotrauma 2019;16:87 Trauma is one of the most common causes of death and However, there are many caveats to this approach. First of disability, and the burden of trauma in the community is all, the authors suggest undergoing a 3-year trauma surgery increasing with rising population, vehicles, and other factors. course so that the surgeons can be trained in trauma surgery Even though great progress has been made in the institution including neurosurgery. However, just as neurosurgeons, many of resources, hospitals, and staff in the country, the main of these graduates will also settle down in big universities and issues of undersupply and maldistribution of trained doctors cities and would likely not settle down in areas where there is are unlikely to change. This is true for developed countries low availability of neurosurgeons. If there are such trauma sur- too; however, the condition is especially acute in India, with geons working in an institution that also has neurosurgeons, a huge population, a low number of specialists, and their con- then there would be an unfortunate conflict of interest between centration in urban areas. The need for equitable distribution the two specialists. With 200 to 300 neurosurgical specialists of specialists is a utopian idea, and hence there needs to be passing out every year, it would be better for the neurosurgi- a different idea to improve the availability of services and cal specialists to provide neurosurgical and neurotrauma care manpower in areas where there is a paucity of availability. -

So You Want to Be a Surgeon? What Does a Surgeon
So you want to be a surgeon? What does a surgeon do? When you hear about surgery and surgeons do you think of what you see on TV in dramas and soaps? In reality surgery is not always so glamorous or dramatic – but it is definitely as exciting. Surgery is challenging, varied, and rewarding but also entails hard work and dedication. Many surgeons say they enjoy the intellectual challenges of their job and its quick results and active approach to the treatment of disease, which is almost unique in medicine. They say that to perform an operation and see a patient's life improve almost immediately is a privilege and enormously satisfying. But a surgeon's life isn't confined to the operating theatre. Surgeons divide their time between several activities, including: Ward rounds: daily visits to check on the condition patients under their care, liaise with nursing staff and colleagues and teach junior doctors. Operating: working on pre-booked elective operations or emergency cases. The operating team includes other surgeons, anaesthetists, technicians, nurses and administrators all working together to ensure the best possible care and outcome for patients. Outpatient clinics: meeting with patients and family members and/or carers to discuss treatment options and explain procedures. Surgeons will also undertake tests and arrange x- rays and scans to decide if an operation is needed or prepare a patient for the procedure. Surgeons meet with patients again after an operation, to monitor and support their recovery. Administration: paperwork is necessary and helps to make sure patients get the right treatment at the right time.