Should Trauma Surgeons Perform Neurosurgery in Emergencies?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
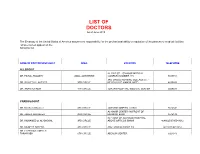
LIST of DOCTORS As of June 2018
LIST OF DOCTORS As of June 2018 The Embassy of the United States of America assumes no responsibility for the professional ability or reputation of the persons or medical facilities whose names appear on the following list. NAME OF DOCTOR/SPECIALIST AREA LOCATION TELEPHONE ALLERGIST AL-RAZI ST. - SAMOOR MEDICAL DR. FAISAL TBAILEH JABAL ALHUSSEIN COMPLEX NUMBER 145 5695151 3RD CIRCLE NURSING COLLAGE ST. - DR. SAYYED AL-NATHER 3RD CIRCLE NEAR HAYAT AMMAN HOTEL 4655893 DR. ANAN ALFAQIH 4TH CIRCLE JORDAN HOSPITAL/ MEDICAL CENTER 5609031 CARDIOLOGIST DR. Munther AlSaafeen 4TH CIRCLE JORDAN HOSPITAL CLINIC 5624840 AL-KHAIR CENTER- IN FRONT OF DR. ZAHER ALKASEEH 3RD CIRCLE HOUSING BANK 4645138 IN FRONT OF ALKHALDI HOSPITAL, DR. MOHAMED O. AL-BAGGAL 3RD CIRCLE ABOVE OPTICOS SHAMI 4646625/0795543012 DR. MUNEER AREEDA 4TH CIRCLE ABU HASSAN COMPLEX 4613613/4613614 DR. HATEM SALAMEH AL- TARAWNEH 5TH CIRCLE ABDOUN CENTER 5924343 DR. AHMAD MOHANNA AL ABDOUN CENTER, INFRONT OF ARABIC HARASEES 5TH CIRCLE CENTER 5924343 DR. IMAD HADAD 4TH CIRCLE JORDAN HOSPITAL CLINIC 5626197/0795303502 DR. NAZIH NAJEH AL-QADIRI 4TH CIRCLE JORDAN HOSPITAL CLINIC 5680060/0796999695 JABER IBN HAYYAN ST./ IBN HAYYAN DR. SUHEIL HAMMOUDEH SHMEISANI MEDICAL COMPLEX 5687484/0795534966 DR. YOUSEF QOUSOUS JABAL AMMAN AL-KHALIDI ST./ AL- BAYROUNI COMP. 4650888/0795599388 CARDIOVASCULAR SURGEON JABAL AMMAN NEAR ALKHALDI DR. SUHEIL SALEH 3RD CIRCLE HOSPITAL 4655772 / 079-5533855 COLORECTAL & GENERAL SURGERY DR. WAIL FATAYER KHALIDI HOSPITAL RAJA CENTER 5TH FLOOR 4633398 / 079-5525090 AL- RYAD COMP.BLDG NO. 41/ FLOOR DR. MARWAN S. RUSAN KHALIDI HOSPITAL ST. GROUND 4655772 / 0795530049 DR. JAMAL ARDAH TLA' AL- ALI IBN AL-HAYTHAM HOSPITAL 5602780 / 5811911 DENTISTS DENTAL CONSULTATION CENTER MAKA ST. -
Partnering with Your Transplant Team the Patient’S Guide to Transplantation
Partnering With Your Transplant Team The Patient’s Guide to Transplantation U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Health Resources and Services Administration This booklet was prepared for the Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation by the United Network for Organ Sharing (UNOS). PARTNERING WITH YOUR TRANSPLANT TEAM THE PATIENT’S GUIDE TO TRANSPLANTATION U.S. Department of Health and Human Services Health Resources and Services Administration Public Domain Notice All material appearing in this document, with the exception of AHA’s The Patient Care Partnership: Understanding Expectations, Rights and Responsibilities, is in the public domain and may be reproduced without permission from HRSA. Citation of the source is appreciated. Recommended Citation U.S. Department of Health and Human Services (2008). Partnering With Your Transplant Team: The Patient’s Guide to Transplantation. Rockville, MD: Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation. DEDICATION This book is dedicated to organ donors and their families. Their decision to donate has given hundreds of thousands of patients a second chance at life. CONTENTS Page INTRODUCTION.........................................................................................................................1 THE TRANSPLANT EXPERIENCE .........................................................................................3 The Transplant Team .......................................................................................................................4 -

A BRI H IEF HISTO Howard R. C ORY of TH the Champion, K HE
A BRIEF HISTORY OF THE FOUNDING OF THE EASTERN ASSOCIATION FOR THE SURGERY OF TRAUMA (EAST) Howard R. Champion, Kimball I. Maull, Lenworth M. Jacobs, Burton H. Harris A BRIEF HISTORY OF THE FOUNDING OF THE EASTERN ASSOCIATION FOR THE SURGERY OF TRAUMA (EAST) Howard R. Champion, Kimball I. Maull, Lenworth M. Jacobs, Burton H. Harris The Eastern Association for the Surgery of Trauma (EAST) was founded by a group of surgeons each of whom had somewhat established themselves in the field of trauma and surgical critical care by the early 1980s and were in the process of developing these disciplines and mentoring young surgeons. EAST has widely exceeded the original aspirations of that group of then-young surgeons. To understand why EAST was created and why it succeeded, it is necessary to glance back to the mid 1980s. The notion of EAST occurred in 1985 within a context of a growing demand for organized trauma care but no appropriate opportunities for young aspiring trauma surgeons to exchange knowledge, discuss advances in patient care, or develop their careers in this field within the discipline of surgery. No vehicle adequately nurtured young surgeons into the field of trauma. Today, EAST is an established and respected surgical organization reaching its 25-year mark with membership (Figure 1) of 1363 now exceeding that of the premier global trauma organization, the American Association for the Surgery of Trauma (AAST) (1227 members). Then The world of the young trauma surgeon in the early to mid 1980s was a very different place than it is more than 25 years later. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

History of Cardiac Trauma Surgery
History of cardiac trauma surgery A J Nicol, MB ChB, FCS (SA), PhD; P H Navsaria, MB ChB, FCS (SA), MMed (Surg); D Kahn, MB ChB, FCS (SA), ChM Department of Surgery, Groote Schuur Hospital, Cape Town, South Africa Corresponding author: A Nicol ([email protected]) The ancient Egyptians, although realising the diaphragm, of the small intestine, of the coronary artery and that blood in the the anatomical importance of the heart, stomach and of the liver is deadly.’[8,9] Aristotle pericardial sac could compress the heart and were largely responsible for the aura of (384 - 322 BC) wrote that ‘The heart again restrict its movement.[17] mysticism and superstition that enveloped is the only one of the viscera, and indeed the heart for centuries. The Egyptian Book the only part of the body, that is unable to The nihilism surrounding cardiac injuries of the Dead (c. 1567 BC) describes how, on tolerate any serious affection. This is but what continued and in 1804 John Bell published entry to the underworld, the jackal-headed might reasonably be expected. For, if the his Discourses of Nature and Care of Wounds, Anubis weighed the heart of the deceased primary or dominant part be diseased, there declaring that ‘there is so little to be done … against a statue of the goddess of truth and is nothing from which the other parts which and the signs and consequences are so clear, justice.[1,2] If the heart weighed the same, the depend upon it can derive sucour’.[10,11] Celsus that it is a waste of time to speak longer of dead person was admitted ‘to the company (1st century AD) recognised the clinical wounds of the heart’.[5,18] of Osiris and the blessed; if not, if his heart features of shock associated with a cardiac was heavy and laden with sin, it was cast to injury when he wrote in De Medicina that, There is dispute over who should be named the devouring beast Ammit’.[3] ‘When the heart is wounded much blood as the first modern cardiac surgeon. -

Trauma, Surgical Critical Care and Acute Care Surgery Services
Trauma, Surgical Critical Care and Acute Care Surgery Services Region’s most experienced nationally verified Level I trauma center The University of Kansas Hospital is the largest regional resource for trauma and acute care surgery. Our multidisciplinary team provides expert care from the time of injury or illness through the patient’s post-hospitalization rehabilitation. The University of Kansas Hospital focuses this specialty practice on the 3 facets of acute care surgery: emergency surgery, trauma surgery and surgical critical care. Our trauma and acute care specialists are in the hospital 24 hours a day, 7 days a week, providing expert surgical care. We specialize in high-acuity surgical and trauma patients with multisystem injuries and complex surgical conditions. • Because we see a large volume of patients, we excel at providing care to surgical and trauma patients. • Our comprehensive approach to care involves a multidisciplinary team that specifically specializes in caring for acute surgical and trauma patients. • As part of an academic medical center, we are active in surgical research, forging new techniques that lead to improved care and recovery. • We are continually focused on quality improvement for optimal outcomes. PB200320120 Specialized care team Level I trauma care Trauma, critical and acute care Concussion management Trauma and acute care surgery patients The Level I Trauma Center at The University of Our surgeons are board-certified in general Timely and effective concussion treatment receive comprehensive treatment from a Kansas Hospital serves the highest volume of surgery and surgical critical care. They provide is important for recovery. Our concussion multidisciplinary team of professionals, each trauma patients in the region. -

Trauma Surgery (PDF)
Edward Via College of Osteopathic Medicine 4th Year Clinical Rotation: Surgical Critical Care MED 8305: Surgical Selective Clinical Rotation COURSE SYLLABUS Chair Contact Information Michael Breiner, MD Phone: 540-231-0600 Chair of Surgery - VC Email: [email protected] Tom Lindsay, DO Phone: 864-327-9842 Associate Chair of Surgery - CC Email: [email protected] Paul Brisson, MD Phone: 334-442-4023 Chair of Surgery - AC Email: [email protected] I. Rotation Description Students will gain hands-on experience in the diagnosis and management of critically injured and acutely ill general surgery, neurosurgery, and trauma patients. Students function as an integral part of the surgical critical care team. The team is responsible for all aspects of critical care including bedside procedures, ventilatory and post-surgical management. Students will present patients on daily ward rounds and take call. II. Rotation Goals The goal of this rotation is to acquire the knowledge and skills necessary to manage patients with problems unique to the surgical intensive care setting. Additionally, students will appreciate the differences in management strategies between the surgical and medical intensive care units. Bedside teaching and procedure training will occur as part of the daily workrounds. a. Basic knowledge that is needed for the resuscitation, diagnosis and treatment of Surgical Critical Care, including General Surgery, Trauma, and Neurosurgery patients b. Instruction in the basic clinical skills needed to treat Surgical Critical Care, including General Surgery, Trauma, and Neurosurgery patients c. An understanding of the continuum of care involved in the treatment of trauma patients from the resuscitation bay through discharge from the ICU. -
World Journal of Critical Care Medicine
World Journal of W J C C M Critical Care Medicine Submit a Manuscript: http://www.wjgnet.com/esps/ World J Crit Care Med 2015 August 4; 4(3): 240-243 Help Desk: http://www.wjgnet.com/esps/helpdesk.aspx ISSN 2220-3141 (online) DOI: 10.5492/wjccm.v4.i3.240 © 2015 Baishideng Publishing Group Inc. All rights reserved. MINIREVIEWS Intensive care organisation: Should there be a separate intensive care unit for critically injured patients? Tim K Timmers, Michiel HJ Verhofstad, Luke PH Leenen Tim K Timmers, Luke PH Leenen, Department of Surgery, care units with an “open format” setting. However, there University Medical Center Utrecht, 3508 GA Utrecht, The are still questions whether surgical patients benefit from Netherlands a general mixed ICU. Trauma is a significant cause of morbidity and mortality throughout the world. Major or Michiel HJ Verhofstad, Department of Surgery, Erasmus severe trauma requiring immediate surgical intervention Medical Center Rotterdam, 3000 CA Rotterdam, The Netherlands and/or intensive care treatment. The role and type of the ICU has received very little attention in the literature Author contributions: Timmers TK designed the research; Timmers TK and Leenen LPH performed the research; Timmers when analyzing outcomes from critical injuries. Severely TK, Verhofstad MHJ and Leenen LPH wrote the paper. injured patients require the years of experience in complex trauma care that only a surgery/trauma ICU Conflict-of-interest statement: The authors declared that they can provide. Should a trauma center have the capability have no competing interests. of a separate specialized ICU for trauma patients (“closed format”) next to its standard general mixed ICU? Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external Key words: Intensive trauma care; Trauma intensive reviewers. -

100 Years. 100 Facts
100 Years. 100 Facts. Celebrating 100 Years as the United Voice of Ohio Hospitals 1819 Daniel Drake obtains a charter for the Medical 001 College of Ohio, the forerunner of the University of Cincinnati College of Medicine. 100 Years. 100 Facts. | 3 1823 Ohio’s first hospital, the Cincinnati Commercial 002 Hospital and Lunatic Asylum, opens. 4 | Ohio Hospital Association 100 Years. 100 Facts. | 5 Starling Medical Center College/Saint 003 Francis Hospital is established on the 1849 present site of Grant Medical Center in Columbus as the first teaching hospital in the U.S. It is the forerunner for the College of Medicine at Ohio State University. 6 | Ohio Hospital Association Charity Hospital Medical Center, now 004 St. Vincent Charity Hospital, opens 1873 Cleveland’s first amphitheater for demonstration of surgery and clinical procedures. 100 Years. 100 Facts. | 7 8 | Ohio Hospital Association 1886 Mother M. Angela and Sister M. Rufina Dunn, of the 005 Congregation of the Sisters of the Holy Cross of Notre Dame, Indiana, convert a sturdy four-story red brick building to two wards, 18 private rooms and an operating room with an amphitheater. The facility is called Hawkes Hospital of Mount Carmel and eventually becomes Mount Carmel West. 100 Years. 100 Facts. | 9 A 10-bed Christ Hospital opens in 006 Cincinnati after a group of local 1889 businessmen led by James Gamble (whose prospering soap business eventually became Procter & Gamble) invited Isabella Thornburg to the city in 1888 to train deaconesses and missionaries. She soon expands beyond training to open a hospital in the west end of the city. -

Surgical Critical Care Skills
Parkland SICU and Parkland MICU Skills and Assessments The program is designed to give the Fellow in-depth instruction in the many aspects of surgical critical care. The multi-disciplinary nature of the Fellowship with rotations in Burn Surgery, Neurosurgery and Pediatric Surgery allows application of knowledge and skills across multiple disciplines. This is further ensured through the delivery of critical care to a large volume of patients. I. Cardiopulmonary Systems/Monitoring and Medical Instrumentation Knowledge Skills Assessment 1. Understand pathophysiology Insert pulmonary artery, central Faculty observation associated with different causes of venous and arterial lines and obtain during rounds, skills hemodynamic instability. Examples hemodynamic data; interpret data and courses (PA Catheter, include types of shock, cardiac arrest. initiate therapy. Instruct junior ICU Ultrasound) and residents in insertion of invasive resuscitation as monitors and interpretation of data. documented on Resuscitate patients from shock and evaluations. cardiac arrest. 2. Know and apply treatments for Recognize and treat ischemia and Observation during arrhythmias, congestive heart failure, arrhythmia on ECG. Utilize correct rounds, MCCKAP as acute ischemia and pulmonary edema. class of anti-arrhythmic, vasodilators noted on evaluation. and diuretics as they pertain to cardiac disease. Be able to interpret and instruct current ACLS guidelines. 3. Understand factors associated with Ability to assess preoperative risk Observation during assessment of preoperative surgical risk. based on history, physical exam, rounds, MCCKAP as Examples include evaluation of the high laboratory and radiographic data. noted on evaluation. risk cardiac patient undergoing non- Correctly interpret data and optimize cardiac surgery. the high-risk cardiopulmonary patient for surgery. 4.Understand pathophysiology Proficiency and ability to instruct in Direct observation; case associated with respiratory failure. -
Go Inside a Surgeon's Typical
HealthSigns Spring 2016 Go Inside a Surgeon’s Typical Day Top in Cancer Getting the Planet Friendly Care Picture Healthcare Earning kudos on quality More advanced imaging How we care for patients for nearly a decade tools in your community and the environment HealthSigns Spring 2016 5 10 Sustaining Going Quality Green Cancer program We’re leading the earns top national way to a healthier, award for third more sustainable time. environment. 6 11 Focused on Parking Garage Healing Near Opening General surgeon More convenient starts each day access helps with energy and patients, families endurance. and our community. 8 Easy Access to Imaging Outpatient center VISIT US ONLINE offers screenings, Stay connected to Washington Hospital at www.whhs.com diagnostics and and on Facebook. Browse our calendar of upcoming events and treatment. other happenings taking place at your community hospital. 2 | SPRING 2016 Information You Can Use MISSION STATEMENT Free, science-based diabetes education classes for people with diabetes and their families or anyone who wants to As the local Health Care District, find out more about this chronic disease affecting more our mission is to meet the than 29 million Americans. health care needs of the District Diabetes Matters residents through medical services, education and research. When: First Thursday of every month (except for July), 7 to 8 p.m. Within this scope, Washington Stay for the Diabetes Support Township Health Care District Group, 8 to 9 p.m. is committed to assuming the Location: Conrad E. Anderson, MD, Auditorium (Washington West) leadership role in improving and 2500 Mowry Ave., Fremont maintaining the health status of No registration needed. -

14 Glossary of Healthcare Terms
Premera Reference Manual Premera Blue Cross 1144 GGlloossssaarryy ooff HHeeaalltthhccaarree TTeerrmmss A Accreditation: Health plan accreditation is a rigorous, comprehensive and transparent evaluation process through which the quality of the systems, processes and results that define a health plan are assessed. Acute: A condition that begins suddenly and does not last very long (e.g., broken arm). ‘acute” is the opposite of “chronic.” Acute Care: Treatment for a short-term or episodic illness or health problem. Adequacy: The extent to which a network offers the appropriate types and numbers of providers in a designated geographic distribution according to the relative availability of such providers in the area and the needs of the plan's members. Adjudication: The process of handling and paying claims. Also see Claim. Admission Notification: Hospitals routinely notify Premera of all inpatient admissions that link members to other care coordination programs, such as readmission prevention. The process includes verification of benefits and assesses any need for case management. Advance Directives: Written instructions that describe a member’s healthcare decision regarding treatment in the event of a serious medical condition which prevents the member from communicating with his/her physician; also called Living Wills. Allied Health Personnel: Specially trained and licensed (when necessary) healthcare workers other than physicians, optometrists, dentists, chiropractors, podiatrists, and nurses. Allowable: An amount agreed upon by the carrier and the practitioner as payment for covered services. Alpha Prefix: Three characters preceding the subscriber identification number on Blue Cross and/or Blue Shield plan ID cards. The alpha prefix identifies the member’s Blue Cross and/or Blue Shield plan or national account and is required for routing claims.