14 Glossary of Healthcare Terms
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
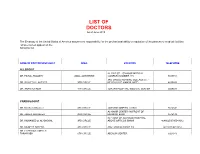
LIST of DOCTORS As of June 2018
LIST OF DOCTORS As of June 2018 The Embassy of the United States of America assumes no responsibility for the professional ability or reputation of the persons or medical facilities whose names appear on the following list. NAME OF DOCTOR/SPECIALIST AREA LOCATION TELEPHONE ALLERGIST AL-RAZI ST. - SAMOOR MEDICAL DR. FAISAL TBAILEH JABAL ALHUSSEIN COMPLEX NUMBER 145 5695151 3RD CIRCLE NURSING COLLAGE ST. - DR. SAYYED AL-NATHER 3RD CIRCLE NEAR HAYAT AMMAN HOTEL 4655893 DR. ANAN ALFAQIH 4TH CIRCLE JORDAN HOSPITAL/ MEDICAL CENTER 5609031 CARDIOLOGIST DR. Munther AlSaafeen 4TH CIRCLE JORDAN HOSPITAL CLINIC 5624840 AL-KHAIR CENTER- IN FRONT OF DR. ZAHER ALKASEEH 3RD CIRCLE HOUSING BANK 4645138 IN FRONT OF ALKHALDI HOSPITAL, DR. MOHAMED O. AL-BAGGAL 3RD CIRCLE ABOVE OPTICOS SHAMI 4646625/0795543012 DR. MUNEER AREEDA 4TH CIRCLE ABU HASSAN COMPLEX 4613613/4613614 DR. HATEM SALAMEH AL- TARAWNEH 5TH CIRCLE ABDOUN CENTER 5924343 DR. AHMAD MOHANNA AL ABDOUN CENTER, INFRONT OF ARABIC HARASEES 5TH CIRCLE CENTER 5924343 DR. IMAD HADAD 4TH CIRCLE JORDAN HOSPITAL CLINIC 5626197/0795303502 DR. NAZIH NAJEH AL-QADIRI 4TH CIRCLE JORDAN HOSPITAL CLINIC 5680060/0796999695 JABER IBN HAYYAN ST./ IBN HAYYAN DR. SUHEIL HAMMOUDEH SHMEISANI MEDICAL COMPLEX 5687484/0795534966 DR. YOUSEF QOUSOUS JABAL AMMAN AL-KHALIDI ST./ AL- BAYROUNI COMP. 4650888/0795599388 CARDIOVASCULAR SURGEON JABAL AMMAN NEAR ALKHALDI DR. SUHEIL SALEH 3RD CIRCLE HOSPITAL 4655772 / 079-5533855 COLORECTAL & GENERAL SURGERY DR. WAIL FATAYER KHALIDI HOSPITAL RAJA CENTER 5TH FLOOR 4633398 / 079-5525090 AL- RYAD COMP.BLDG NO. 41/ FLOOR DR. MARWAN S. RUSAN KHALIDI HOSPITAL ST. GROUND 4655772 / 0795530049 DR. JAMAL ARDAH TLA' AL- ALI IBN AL-HAYTHAM HOSPITAL 5602780 / 5811911 DENTISTS DENTAL CONSULTATION CENTER MAKA ST. -

The Stethoscope: Some Preliminary Investigations
695 ORIGINAL ARTICLE The stethoscope: some preliminary investigations P D Welsby, G Parry, D Smith Postgrad Med J: first published as on 5 January 2004. Downloaded from ............................................................................................................................... See end of article for Postgrad Med J 2003;79:695–698 authors’ affiliations ....................... Correspondence to: Dr Philip D Welsby, Western General Hospital, Edinburgh EH4 2XU, UK; [email protected] Submitted 21 April 2003 Textbooks, clinicians, and medical teachers differ as to whether the stethoscope bell or diaphragm should Accepted 30 June 2003 be used for auscultating respiratory sounds at the chest wall. Logic and our results suggest that stethoscope ....................... diaphragms are more appropriate. HISTORICAL ASPECTS note is increased as the amplitude of the sound rises, Hippocrates advised ‘‘immediate auscultation’’ (the applica- resulting in masking of higher frequency components by tion of the ear to the patient’s chest) to hear ‘‘transmitted lower frequencies—‘‘turning up the volume accentuates the sounds from within’’. However, in 1816 a French doctor, base’’ as anyone with teenage children will have noted. Rene´The´ophile Hyacinth Laennec invented the stethoscope,1 Breath sounds are generated by turbulent air flow in the which thereafter became the identity symbol of the physician. trachea and proximal bronchi. Airflow in the small airways Laennec apparently had observed two children sending and alveoli is of lower velocity and laminar in type and is 6 signals to each other by scraping one end of a long piece of therefore silent. What is heard at the chest wall depends on solid wood with a pin, and listening with an ear pressed to the conductive and filtering effect of lung tissue and the the other end.2 Later, in 1816, Laennec was called to a young characteristics of the chest wall. -

Report of Two Cases Presenting with Acute Abdominal Symptoms
Journal of Accident and Tension pneumothorax: report of two cases presenting J Accid Emerg Med: first published as 10.1136/emj.11.1.43 on 1 March 1994. Downloaded from Emergency Medicine 1993 with acute abdominal symptoms 10, 43-44 G.W. HOLLINS,1 T. BEATTIE,1 1. HARPER2 & K. LITTLE2 Departments of Accident and Emergency 1 Aberdeen Royal Infirmary, Foresterhill, Aberdeen and 2Royal Infirmary of Edinburgh, Lauriston Place, Edinburgh INTRODUCTION diagnoses were peptic ulcer disease or acute pancreatitis. Work-up appropriate to these diag- Tension pneumothorax constitutes a medical noses was commenced. An erect chest radiograph emergency and rapid diagnosis should be possible revealed a large pneumothorax with mediastinal on the basis of history and clinical examination. shift to the left. Following drainage using a large Following treatment with the delivery of high con- bore needle there was immediate resolution of his centration oxygen and the insertion of a large bore symptoms and all abdominal signs. An intercostal needle into the pleural space of the affected side, chest drain was formally sited and full expansion of the diagnosis can be confirmed radiologically and his right lung was achieved after 36 h. He was dis- an intercostal chest drain formally sited.1'2 We report charged home after 3 days. two cases where diagnosis was not made on the basis of history and examination alone. Both cases Case 2 presented with symptoms and signs suggestive of an acute intra-abdominal pathology and the diag- A 37-year-old male computer operator presented nosis was only made on radiological grounds. with a 1-week history of general malaise associated with mild neck and back pain. -

Educators OPHTHALMOLOGY
Summer 2018 UNIVERSITY OF CINCINNATI OPHTHALMOLOGY Educators MAKING INTERNATIONAL Contributions Clinical Collaborations Outreach UNIVERSITY OF CINCINNATI Department of OPHTHALMOLOGY Karl C. Golnik, MD, MEd Professor and Chair Hisham H. Arar, MD James J. Augsburger, MD Shana Brafman, OD Chairman’s Update Sandra Brook, OD Greetings! I hope you found our last newsletter highlighting our educational program informative and exciting! David Brounley, MD Kelsey Carriere, OD In this issue we highlight our Department’s extensive international outreach, activities, and future plans. I contin- Fred Chu, MD ue in my role as Director for Education for the International Council of Ophthalmology. In addition, I am serving John S. Cohen, MD Anne L. Corn, EdD as both the Secretary for International Relations of the International Joint Com- Zelia M. Correa, MD, PhD mission on Allied Health (IJCAHPO) and as a consultant to Orbis. Our faculty Eniolami Dosunmu, MD Robert E. Foster, MD and residents also have continued their impressive international endeavors. See Mindy Call Fox, PhD inside this edition for further details. W. Michael Gaynier, DO Robert Goulet, MD Our next newsletter will highlight some of our Department’s Alumni Michael E. Gray, MD achievements and activities. Linda J. Greff MD Fumika Hamada, PhD I encourage comments and feedback regarding our newsletter. Please send Daniel Hammer, MD Michele Wyan ([email protected]) relevant information for inclusion in Michael Hater, MD Ginger Henson, MD our upcoming issues. Also, please feel free to contact me directly either at 513- Erich Hinel, OD 558-5151 or [email protected]. We are looking forward to hearing from Katherine Hogan, OD Edward J. -

Geriatric Medicine and Why We Need Geriatricians! by Juergen H
Geriatric Medicine and why we need Geriatricians! by Juergen H. A. Bludau, MD hat is geriatric medicine? Why is there a need for 1. Heterogeneity: As people age, they become more Wthis specialty? How does it differ from general heterogeneous, meaning that they become more and more internal medicine? What do geriatricians do differently when different, sometimes strikingly so, with respect to their they evaluate and treat an older adult? These are common health and medical needs. Imagine for a moment a group questions among patients and physicians alike. Many of 10 men and women, all 40 years old. It is probably safe internists and family practitioners argue, not unjustifiably, to say that most, if not all, have no chronic diseases, do not that they have experience in treating and caring for older see their physicians on a regular basis, and take no long- patients, especially since older adults make up almost half of term prescription medications. From a medical point of all doctors visits. So do we really need another type of view, this means that they are all very similar. Compare this physician to care for older adults? It is true that geriatricians to a group of 10 patients who are 80 years old. Most likely, may not necessarily treat older patients differently per se. But you will find an amazingly fit and active gentleman who there is a very large and important difference in that the focus may not be taking any prescription medications. On the of the treatment is different. In order to appreciate how other end of the spectrum, you may find a frail, memory- significant this is, we need to look at what makes an older impaired, and wheelchair-bound woman who lives in a adult different from a younger patient. -

Acute Gastroenteritis
Article gastrointestinal disorders Acute Gastroenteritis Deise Granado-Villar, MD, Educational Gap MPH,* Beatriz Cunill-De Sautu, MD,† Andrea In managing acute diarrhea in children, clinicians need to be aware that management Granados, MDx based on “bowel rest” is outdated, and instead reinstitution of an appropriate diet has been associated with decreased stool volume and duration of diarrhea. In general, drug therapy is not indicated in managing diarrhea in children, although zinc supplementation Author Disclosure and probiotic use show promise. Drs Granado-Villar, Cunill-De Sautu, and Objectives After reading this article, readers should be able to: Granados have disclosed no financial 1. Recognize the electrolyte changes associated with isotonic dehydration. relationships relevant 2. Effectively manage a child who has isotonic dehydration. to this article. This 3. Understand the importance of early feedings on the nutritional status of a child who commentary does has gastroenteritis. contain a discussion of 4. Fully understand that antidiarrheal agents are not indicated nor recommended in the an unapproved/ treatment of acute gastroenteritis in children. investigative use of 5. Recognize the role of vomiting in the clinical presentation of acute gastroenteritis. a commercial product/ device. Introduction Acute gastroenteritis is an extremely common illness among infants and children world- wide. According to the Centers for Disease Control and Prevention (CDC), acute diarrhea among children in the United States accounts for more than 1.5 million outpatient visits, 200,000 hospitalizations, and approximately 300 deaths per year. In developing countries, diarrhea is a common cause of mortality among children younger than age 5 years, with an estimated 2 million deaths each year. -
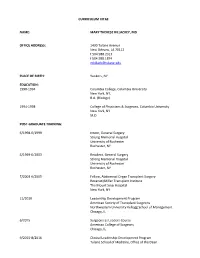
CV-Summer 2017.Pdf
CURRICULUM VITAE NAME: MARY THERESE KILLACKEY, MD OFFICE ADDRESS: 1430 Tulane Avenue New Orleans, LA 70112 t 504.988.2317 f 504.988.1874 [email protected] PLACE OF BIRTH: Yonkers, NY EDUCATION: 1990-1994 Columbia College, Columbia University New York, NY, B.A. (Biology) 1994-1998 College of Physicians & Surgeons, Columbia University New York, NY M.D. POST-GRADUATE TRAINING: 6/1998-6/1999 Intern, General Surgery Strong Memorial Hospital University of Rochester Rochester, NY 6/1999-6/2003 Resident, General Surgery Strong Memorial Hospital University of Rochester Rochester, NY 7/2003-6/2005 Fellow, Abdominal Organ Transplant Surgery Recanati/Miller Transplant Institute The Mount Sinai Hospital New York, NY 11/2010 Leadership Development Program American Society of Transplant Surgeons Northwestern University Kellogg School of Management Chicago, IL 6/2015 Surgeons as Leaders Course American College of Surgeons Chicago, IL 9/2015-8/2016 Clinical Leadership Development Program Tulane School of Medicine, Office of the Dean New Orleans, LA 12/2015 Mid-Career Women Faculty Professional Development Seminar Association of American Medical Colleges Austin, TX 6/2016 Being a Resilient Leader Association of American Medical Colleges Washington, DC 6/2017 - 4/2018 Fellow, Executive Leadership in Academic Medicine Drexel University College of Medicine Philadelphia, PA ACADEMIC APPOINTMENTS: 7/2003-6/2005 Instructor in Surgery Mount Sinai School of Medicine New York, NY 10/2006-present Assistant Professor of Surgery and Pediatrics Tulane University -

How to Talk with Your Family About Sjögren's LETTER from SSF CEO
Volume 32, Issue 10 November/December 2014 SjogrensSyndromeFoundation @MoistureSeekers LETTER FROM SSF CEO STEVEN TAYLOR his is the time of the year that we at the Sjögren’s Syndrome Foun- dation look back and give thanks to all of you who have supported Tus throughout the year! Thanks to your generous support, the SSF has continued to soar to new heights as we strive to conquer Sjögren’s. Patient care continues to be a focus of the SSF. With the develop- ment of the SSF’s Clinical Practice Guidelines for Sjögren’s, patients will eventually see standardized care in how healthcare providers treat, manage and monitor their Sjögren’s patients. This initiative marks the first time in the history of the disease that a roadmap for treating Sjögren’s has been developed. The SSF is proud to be the lead organization to make this happen for all Sjögren’s patients, and we couldn’t do it without the support of hundreds of healthcare profes- sionals who, along with the SSF staff, are researching the evidence, discussing the best continued page 2 t How to Talk With Your Family about Sjögren’s here is a growing body of evidence that rich social support networks are Timportant to overall health, immune function and healing. They improve quality of life and facilitate coping with chronic illness. Conversely, negative social interac- tions create a stress response that have the opposite effect. Support from family members and close friends can be one of the most important resources for you to draw on when dealing with Sjögren’s. -

Health by Numbers the Economic Burden of Preventable Chronic
HEALTH BY NUMBERS PUBLIC HEALTH MICHAEL FINE, MD DIRECTOR, RHODE ISLAND DEPARTMENT OF HEALTH EDITED BY SAMARA VINER-BROWN, MS The Economic Burden of Preventable Chronic Diseases in Rhode Island DEBORAH N. PEARLMAN, PhD; DARREN KAW, MPH; SOPHIE O’CONNELL, MA; YONGWEN JIANG, PhD; DONA GOLDMAN, RN, MPH 36 39 EN The Centers for Disease Control and Prevention (CDC) have a myocardial infarction; (2) coronary artery disease; (3) a identified seven chronic conditions where a comprehensive stroke; (4) asthma; (5) arthritis (defined in this questionnaire approach to prevention could save tremendous health care as rheumatoid arthritis, gout, lupus, or fibromyalgia); (6) dia- costs and reduce premature disability and death in the US. betes; and 7) high blood pressure. Adults ever diagnosed with These potentially “preventable” chronic diseases include asthma were asked if they still had asthma (current asthma). heart disease, stroke, some cancers, diabetes, arthritis,1 and The presence or absence of each condition was determined asthma.2 by a “yes” or “no” response, respectively. Women reporting In 2014, the Milken Institute study estimated the impact diabetes or high blood pressure only when pregnant were on the US economy of seven chronic diseases – cancer, excluded from these respective variables. diabetes, hypertension, stroke, heart disease, pulmonary Cardiovascular disease was based on a “yes” response to conditions, and mental illness – at $1.3 trillion annually.3 having one or more of the following diagnosed conditions: Projected costs were $28 billion more than that forecast in high blood pressure, myocardial infarction, coronary artery 2007.4 The leading drivers of health care costs were increas- disease, or a stroke. -
Partnering with Your Transplant Team the Patient’S Guide to Transplantation
Partnering With Your Transplant Team The Patient’s Guide to Transplantation U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Health Resources and Services Administration This booklet was prepared for the Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation by the United Network for Organ Sharing (UNOS). PARTNERING WITH YOUR TRANSPLANT TEAM THE PATIENT’S GUIDE TO TRANSPLANTATION U.S. Department of Health and Human Services Health Resources and Services Administration Public Domain Notice All material appearing in this document, with the exception of AHA’s The Patient Care Partnership: Understanding Expectations, Rights and Responsibilities, is in the public domain and may be reproduced without permission from HRSA. Citation of the source is appreciated. Recommended Citation U.S. Department of Health and Human Services (2008). Partnering With Your Transplant Team: The Patient’s Guide to Transplantation. Rockville, MD: Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation. DEDICATION This book is dedicated to organ donors and their families. Their decision to donate has given hundreds of thousands of patients a second chance at life. CONTENTS Page INTRODUCTION.........................................................................................................................1 THE TRANSPLANT EXPERIENCE .........................................................................................3 The Transplant Team .......................................................................................................................4 -

Improving the Accuracy of Medical Diagnosis with Causal Machine Learning ✉ Jonathan G
ARTICLE https://doi.org/10.1038/s41467-020-17419-7 OPEN Improving the accuracy of medical diagnosis with causal machine learning ✉ Jonathan G. Richens 1 , Ciarán M. Lee1,2 & Saurabh Johri 1 Machine learning promises to revolutionize clinical decision making and diagnosis. In medical diagnosis a doctor aims to explain a patient’s symptoms by determining the diseases causing them. However, existing machine learning approaches to diagnosis are purely associative, 1234567890():,; identifying diseases that are strongly correlated with a patients symptoms. We show that this inability to disentangle correlation from causation can result in sub-optimal or dangerous diagnoses. To overcome this, we reformulate diagnosis as a counterfactual inference task and derive counterfactual diagnostic algorithms. We compare our counterfactual algorithms to the standard associative algorithm and 44 doctors using a test set of clinical vignettes. While the associative algorithm achieves an accuracy placing in the top 48% of doctors in our cohort, our counterfactual algorithm places in the top 25% of doctors, achieving expert clinical accuracy. Our results show that causal reasoning is a vital missing ingredient for applying machine learning to medical diagnosis. 1 Babylon Health, 60 Sloane Ave, Chelsea, London SW3 3DD, UK. 2 University College London, Gower St, Bloomsbury, London WC1E 6BT, UK. ✉ email: [email protected] NATURE COMMUNICATIONS | (2020)11:3923 | https://doi.org/10.1038/s41467-020-17419-7 | www.nature.com/naturecommunications 1 ARTICLE NATURE COMMUNICATIONS | https://doi.org/10.1038/s41467-020-17419-7 roviding accurate and accessible diagnoses is a fundamental Since its formal definition31, model-based diagnosis has been challenge for global healthcare systems. -

General Surgery
- 1 - KALEIDA HEALTH Name: ___________________________________ Date: ____________________________ DELINEATION OF PRIVILEGES - GENERAL SURGERY PLEASE NOTE: Please check the box for each privilege requested. Do not use an arrow or line to make selections. We will return applications that ignore this directive. GENERAL STATEMENTS - Privileges in Adult Surgery are separated into the following divisions: General Surgery and Plastic Surgery. Applicants desiring procedure privileges in more than one division must complete separate forms for each. Procedures designated with an asterisk (*) indicate that Moderate or Deep Sedation may be required. If you do not have Moderate or Deep Sedation privileges, you must invite a Kaleida Health anesthesiologist to participate in the procedure. Procedures are also separated into levels of complexity (Level I-A, Level I-B, Level I, Level II, and Level III), which require increasing levels of education and experience. In general, procedures learned during residency are grouped in Level I-A or Level I and are granted upon evidence of successful completion of residency training. Level II procedures may or may not require evidence of additional training beyond residency. Documentation of additional training and/or experience is required for all Level III procedures. LEVEL I-A PRIVILEGES Procedures which involve primarily wound care, can be done under local anesthetic and occasionally involve application of temporary skin coverage or application of agents to expedite wound healing. Can be performed by any competent