Introducing Ophthalmology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
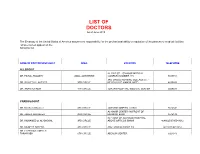
LIST of DOCTORS As of June 2018
LIST OF DOCTORS As of June 2018 The Embassy of the United States of America assumes no responsibility for the professional ability or reputation of the persons or medical facilities whose names appear on the following list. NAME OF DOCTOR/SPECIALIST AREA LOCATION TELEPHONE ALLERGIST AL-RAZI ST. - SAMOOR MEDICAL DR. FAISAL TBAILEH JABAL ALHUSSEIN COMPLEX NUMBER 145 5695151 3RD CIRCLE NURSING COLLAGE ST. - DR. SAYYED AL-NATHER 3RD CIRCLE NEAR HAYAT AMMAN HOTEL 4655893 DR. ANAN ALFAQIH 4TH CIRCLE JORDAN HOSPITAL/ MEDICAL CENTER 5609031 CARDIOLOGIST DR. Munther AlSaafeen 4TH CIRCLE JORDAN HOSPITAL CLINIC 5624840 AL-KHAIR CENTER- IN FRONT OF DR. ZAHER ALKASEEH 3RD CIRCLE HOUSING BANK 4645138 IN FRONT OF ALKHALDI HOSPITAL, DR. MOHAMED O. AL-BAGGAL 3RD CIRCLE ABOVE OPTICOS SHAMI 4646625/0795543012 DR. MUNEER AREEDA 4TH CIRCLE ABU HASSAN COMPLEX 4613613/4613614 DR. HATEM SALAMEH AL- TARAWNEH 5TH CIRCLE ABDOUN CENTER 5924343 DR. AHMAD MOHANNA AL ABDOUN CENTER, INFRONT OF ARABIC HARASEES 5TH CIRCLE CENTER 5924343 DR. IMAD HADAD 4TH CIRCLE JORDAN HOSPITAL CLINIC 5626197/0795303502 DR. NAZIH NAJEH AL-QADIRI 4TH CIRCLE JORDAN HOSPITAL CLINIC 5680060/0796999695 JABER IBN HAYYAN ST./ IBN HAYYAN DR. SUHEIL HAMMOUDEH SHMEISANI MEDICAL COMPLEX 5687484/0795534966 DR. YOUSEF QOUSOUS JABAL AMMAN AL-KHALIDI ST./ AL- BAYROUNI COMP. 4650888/0795599388 CARDIOVASCULAR SURGEON JABAL AMMAN NEAR ALKHALDI DR. SUHEIL SALEH 3RD CIRCLE HOSPITAL 4655772 / 079-5533855 COLORECTAL & GENERAL SURGERY DR. WAIL FATAYER KHALIDI HOSPITAL RAJA CENTER 5TH FLOOR 4633398 / 079-5525090 AL- RYAD COMP.BLDG NO. 41/ FLOOR DR. MARWAN S. RUSAN KHALIDI HOSPITAL ST. GROUND 4655772 / 0795530049 DR. JAMAL ARDAH TLA' AL- ALI IBN AL-HAYTHAM HOSPITAL 5602780 / 5811911 DENTISTS DENTAL CONSULTATION CENTER MAKA ST. -

2018 Department of Ophthalmology Chair Report
SAVE THE▼ DATE Department of 200 Ophthalmology Years www.NYEE.edu Anniversary SPECIALTY REPORT | FALL 2018 www.NYEE.edu Celebration Join us for 200 Years and Counting: Bicentennial Cocktail Celebration October 15, 2020 Research Breakthrough: The Plaza 768 5th Avenue Gene Transfer New York, NY Therapy Restores 200 Years and Counting: Ophthalmology Vision in Mice Symposium October 16, 2020 Stay tuned for details on tickets and registration information. Cover image: Slice of a central retina section showing all layers (ONL, INL, GCL). Red indicates rod photoreceptors, located in outer nuclear layer (ONL). Green indicates Müller glial cells, whose cell bodies are located in inner nuclear layer (INL), and their branches across all three layers. Dark blue indicates the nucleus of all cells in three layers (GCL). Icahn School of Medicine at Medical Directors Neuro-Ophthalmology Uveitis and Ocular Immunology Mount Sinai Departmental Mark Kupersmith, MD Douglas Jabs, MD, MBA Avnish Deobhakta, MD Leadership System Chief, System Chief, Uveitis and Ocular Medical Director, NYEE - Neuro-Ophthalmology, Immunology, MSHS James C. Tsai, MD, MBA East 85th Street MSHS President, NYEE Stephanie Llop, MD System Chair, Department of Robin N. Ginsburg, MD 3 Message From the System Chair of the DepartmentValerie Elmalem, of Ophthalmology MD Sophia Saleem, MD Ophthalmology, MSHS Medical Director, NYEE- Joel Mindel, MD East 102nd Street Louis4 R. Pasquale,Breaking MD New Ground in Gene Transfer Therapy to Restore Vision Affiliated Leadership Ocular Oncology Site Chair, Department of Gennady Landa, MD Paul Finger, MD Ebby Elahi, MD, MBA Ophthalmology, MSH and MSQ Medical Director, NYEE- 6 This i-Doctor Is Transforming the Field of Ophthalmology President, NYEE/MSH System Vice Chair, Translational Williamsburg and Tribeca Ophthalmic Pathology Ophthalmology Alumni Ophthalmology Research, MSHS Jodi Sassoon, MD Society Kira Manusis, MD Inside Feature Site Chair, Pathology, NYEE Medical Director, NYEE- Paul A. -

Binocular Vision and the Stroop Test
1040-5488/16/9302-0194/0 VOL. 93, NO. 2, PP. 194Y208 OPTOMETRY AND VISION SCIENCE Copyright * 2015 American Academy of Optometry REVIEW Binocular Vision and the Stroop Test Franc¸ois Daniel* and ZoB Kapoula† ABSTRACT Purpose. Recent studies report a link between optometric results, learning disabilities, and problems in reading. This study examines the correlations between optometric tests of binocular vision, namely, of vergence and accommodation, reading speed, and cognitive executive functions as measured by the Stroop test. Methods. Fifty-one students (mean age, 20.43 T 1.25 years) were given a complete eye examination. They then performed the reading test L’Alouette and the Stroop interference test at their usual reading distance. Criteria for selection were the absence of significant refractive uncorrected error, strabismus, amblyopia, color vision defects, and other neurologic findings. Results. The results show a correlation between positive fusional vergences (PFVs) at near distance and the interference effect (IE) in the Stroop test: the higher the PFV value is, the less the IE. Furthermore, the subgroup of 11 students presenting convergence insufficiency, according to Scheiman and Wick criteria (2002), showed a significantly higher IE during the Stroop test than the other students (N = 18) who had normal binocular vision without symptoms at near. Importantly, there is no correlation between reading speed and PFV either for the entire sample or for the subgroups. Conclusions. These results suggest for the first time a link between convergence capacity and the interference score in the Stroop test. Such a link is attributable to the fact that vergence control and cognitive functions mobilize the same cortical areas, for example, parietofrontal areas. -

Visual Field Test
EYE FACTS visual field test Your visual field refers to how much you can see around you, including objects in your peripheral (side) vision. This test produces a map of your field of vision. Visual field tests help your ophthalmologist (Eye M.D.) monitor any loss of vision and diagnose eye problems and disease. Visual field testing is used to monitor peripheral, or side, vision. HOW IS A VISUAL FIELD TEST PERFORMED? The test is performed with a large, bowl-shaped in- Normal visual field Severe visual loss strument called a perimeter. In order to test one eye at a time, one of your eyes is temporarily patched during the test. You will be seated and positioned comfortably in front of the perimeter and asked to look straight ahead at a fixed spot (the fixation target). The computer randomly flashes points of light around the bowl-shaped perimeter. When you see a light, press the indicator button. It is very important These grids are results of visual field tests.T he dark to always keep looking straight ahead. Do not move black shaded areas show where loss of vision has your eyes to look for the target; wait until it appears occurred. in your side vision. It is normal for some of the lights to be difficult to see. A delay in seeing a light does not necessarily mean your field of vision is damaged. If you need to rest during the test, tell the technician and they will pause the test until you are ready to continue. Your ophthalmologist will interpret the results of your test and discuss them with you. -

Prescription Companion
PRESCRIPTION COMPANION ©2012Transitions Optical inc. ophthalmic lens technical reference JUBILEE YEAR 2012 E -Edition 7 www.norville.co.uk Introduction and Page Index The Norville Companion is a supporting publication for our Prescription Catalogue, providing further technical details, hints and ideas gleaned from everyday experiences. TOPIC Page(s) TOPIC Page(s) Index 2 - 3 Part II Rx Allsorts Lens Shapes 4 - 6 Lens Forms 49 Effective Diameter Chart 7 Base Curves 50 - 51 Simplify Rx 8 Aspherics 52 - 53 Ophthalmic Resins 9 Free-form Digital Design 54 Indices of Ophthalmic lenses - Resin 10 Compensated Lens Powers 55 - 56 Polycarbonate 11 Intelligent Prism Thinning 57 - 58 Trivex 12 - 13 Superlenti - Glass 59 Resin Photochromic Lenses 14 Superlenti - Resin 60 Transitions Availability Check List 15 V Value / Fresnels 61 Nupolar Polarising Lenses 16 E Style Bifocal / Trifocal 62 Drivewear Lenses 17 - 18 Photochromic / Glazing / Prisms 63 UV Protective Lenses 19 Lens Measures 64 Norville PLS Tints 20 Sports 65 Tinted Resin Lenses 21 3D Technology Overview 66 Mid and High Index Resins Tintability 22 Rx Ordering 67 Norlite Tint Transmission Charts 23 - 25 Order Progress 68 Norlite Speciality Tinted Resins 26 - 31 Rx Order Form 69 Norlite Mirror Coating 32 Queries 70 Reflection Free Coating 33 - 34 Optical Heritage 71 F.A.Q. Reflection Free Coatings 35 - 37 Rx House - Change afoot? 72 - 73 Indices of Ophthalmic Lenses - Glass 38 Remote Edging 74 Glass Photochromic Lenses 38 Remote edging - F.A.Q. 75 Speciality Absorbing Glass 39 Quality Assurance -
Partnering with Your Transplant Team the Patient’S Guide to Transplantation
Partnering With Your Transplant Team The Patient’s Guide to Transplantation U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Health Resources and Services Administration This booklet was prepared for the Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation by the United Network for Organ Sharing (UNOS). PARTNERING WITH YOUR TRANSPLANT TEAM THE PATIENT’S GUIDE TO TRANSPLANTATION U.S. Department of Health and Human Services Health Resources and Services Administration Public Domain Notice All material appearing in this document, with the exception of AHA’s The Patient Care Partnership: Understanding Expectations, Rights and Responsibilities, is in the public domain and may be reproduced without permission from HRSA. Citation of the source is appreciated. Recommended Citation U.S. Department of Health and Human Services (2008). Partnering With Your Transplant Team: The Patient’s Guide to Transplantation. Rockville, MD: Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation. DEDICATION This book is dedicated to organ donors and their families. Their decision to donate has given hundreds of thousands of patients a second chance at life. CONTENTS Page INTRODUCTION.........................................................................................................................1 THE TRANSPLANT EXPERIENCE .........................................................................................3 The Transplant Team .......................................................................................................................4 -

Optic Disc and Macular Vessel Density Measured by Optical
www.nature.com/scientificreports OPEN Optic Disc and Macular Vessel Density Measured by Optical Coherence Tomography Angiography in Open-Angle and Angle-Closure Glaucoma Tzu-Yu Hou1,2, Tung-Mei Kuang1,2, Yu-Chieh Ko1,2, Yu-Fan Chang1,2, Catherine Jui-Ling Liu1,2 & Mei-Ju Chen1,2* There is distinct pathogenesis between primary open-angle glaucoma (POAG) and primary angle- closure glaucoma (PACG). Although elevated intraocular pressure (IOP) is the major risk factor for glaucoma, non-IOP risk factors such as vascular abnormalities and lower systolic/diastolic perfusion pressure may play a role in the pathogenic process. This study aimed to compare the vessel density (VD) in the optic disc and macula using optical coherence tomography angiography (OCTA) between POAG and PACG eyes. Thirty-two POAG eyes, 30 PACG eyes, and 39 control eyes were included. All the optic disc VD parameters except the inside disc VD were signifcantly lower in glaucomatous eyes than in control eyes. Compared with PACG eyes, only the inferior temporal peripapillary VD was signifcantly lower in POAG eyes. The parafoveal VD was signifcantly lower in each quadrant in glaucomatous eyes than in control eyes. The central macular and parafoveal VD did not difer between POAG and PACG eyes. In conclusion, the inferior temporal peripapillary VD was signifcantly reduced in POAG eyes compared with PACG eyes, while PACG eyes showed a more evenly distributed reduction in the peripapillary VD. The distinct patterns of VD change may be associated with the diferent pathogenesis between POAG and PACG. Glaucoma is an optic neuropathy characterised by progressive loss of retinal ganglion cells and their axons accompanied by corresponding visual feld (VF) defects. -

Physical Eye Examination
Physical Eye Examination Kaevalin Lekhanont, MD Department of Ophthalmology Ramathibodi Hospp,ital, Mahidol Universit y Outline • Visual acuity (VA) testing – Distant VA test – Pinhole test – Near VA test • Visual field testing • Record and interpretations Outline • Penlight examination •Swingggping penli ght test • Direct ophthalmoscopy – Red reflex examination • Schiotz tonometry • RdditttiRecord and interpretations Conjunctiva, Sclera Retina Cornea Iris Retinal blood vessels Fovea Pupil AtAnteri or c ham ber Vitreous Aqueous humor Lens Optic nerve Trabecular meshwork Ciliary body Choriod and RPE Function evaluation • Visual function – Visual acuity test – Visual field test – Refraction • Motility function Anatomical evaluation Visual acuity test • Distant VA test • Near VA test Distance VA test Snellen’s chart • 20 ฟุตหรือ 6 เมตร • วัดที่ละขาง ตาขวากอนตาซาย • ออานทละตาานทีละตา แถวบนลงลแถวบนลงลางาง • บันทึกแถวลางสุดที่อานได Pinhole test VA with pinhole (PH) Refractive error emmetitropia myypopia hyperopia VA record 20/200 ผูปวยสามารถอานต ัวเลขทมี่ ี ขนาดใหญขนาดใหญพอทคนปกตพอที่คนปกติ สามารถอานไดจากท ี่ระยะ 200 ฟตฟุต แตแตผผปูปวยอานไดจากวยอานไดจาก ที่ระยะ 20 ฟุต 20/20 Distance VA test • ถาอานแถวบนสุดไไไมได ใหเดินเขาใกล chthart ทีละกาวจนอานได (10/200, 5/200) • Counting finger 2ft - 1ft - 1/2ft • Hand motion • Light projection • Light perception • No light perception (NLP) ETDRS Chart Most accurate Illiterate E chart For children age ≥ 3.5 year Near VA test Near chart •14 นวิ้ หรอื 33 เซนตเมตริ • วัดที่ละขาง ตาขวากอนตาซาย • อานทีละตา แถวบนลงลาง -

UCSF Ophthalmology Advice Guide Authors: Seanna Grob, MD, MAS
UCSF Ophthalmology Advice Guide Authors: Seanna Grob, MD, MAS and Neeti Parikh, MD Hello! We are excited that you are interested in ophthalmology! It is truly a special field in medicine. From saving someone’s vision after severe eye trauma, to restoring vision with cataract, retina, or cornea surgery, to preserving someone’s vision with glaucoma management and surgery, to reconstructing someone’s periocular area after trauma, burns, or tumor removal, amazing things can happen in ophthalmology. Ophthalmologists love their job and the majority say they would pick this specialty again if they had the choice. An incredible amount of job satisfaction comes from saving someone’s vision! We are here for you in the UCSF Department of Ophthalmology! We have put together this guide to help you through the process. This guide is meant to be very comprehensive. We want to make sure you are aware of all the opportunities and resources you have so that you can plan accordingly. You do not have to do everything we mention! Please feel free to reach out with questions about the specialty, how to get involved, and how to become a great ophthalmology applicant! 1 Medical School A well-rounded application is important for a successful match and any way you can prove to ophthalmology programs that you are dedicated to the field will be helpful to you. As more objective data (such as grades and board scores become less prevalent) other parts of your application will become more important. Various experiences you seek out are not only fun and educational, but will offer exposure to this wonderful field. -

The Complexity and Origins of the Human Eye: a Brief Study on the Anatomy, Physiology, and Origin of the Eye
Running Head: THE COMPLEX HUMAN EYE 1 The Complexity and Origins of the Human Eye: A Brief Study on the Anatomy, Physiology, and Origin of the Eye Evan Sebastian A Senior Thesis submitted in partial fulfillment of the requirements for graduation in the Honors Program Liberty University Spring 2010 THE COMPLEX HUMAN EYE 2 Acceptance of Senior Honors Thesis This Senior Honors Thesis is accepted in partial fulfillment of the requirements for graduation from the Honors Program of Liberty University. ______________________________ David A. Titcomb, PT, DPT Thesis Chair ______________________________ David DeWitt, Ph.D. Committee Member ______________________________ Garth McGibbon, M.S. Committee Member ______________________________ Marilyn Gadomski, Ph.D. Assistant Honors Director ______________________________ Date THE COMPLEX HUMAN EYE 3 Abstract The human eye has been the cause of much controversy in regards to its complexity and how the human eye came to be. Through following and discussing the anatomical and physiological functions of the eye, a better understanding of the argument of origins can be seen. The anatomy of the human eye and its many functions are clearly seen, through its complexity. When observing the intricacy of vision and all of the different aspects and connections, it does seem that the human eye is a miracle, no matter its origins. Major biological functions and processes occurring in the retina show the intensity of the eye’s intricacy. After viewing the eye and reviewing its anatomical and physiological domain, arguments regarding its origins are more clearly seen and understood. Evolutionary theory, in terms of Darwin’s thoughts, theorized fossilization of animals, computer simulations of eye evolution, and new research on supposed prior genes occurring in lower life forms leading to human life. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

And Minus Cylinder Subjective Refraction Techniques for Clinicians January 2016
Mark E Wilkinson, OD Plus and Minus Cylinder Subjective Refraction Techniques for Clinicians January 2016 General Refraction Techniques Prior to starting your refraction, baseline visual acuities (OD, OS and OU) must be determined. For individuals with near vision complaints, and all presbyopes, near acuity should also be documented using M notation, with the testing distance documented if different than 16 inches (40 centimeters). Accurately assessing visual acuity is important for many reasons. It allows the clinician to: § Determine best corrected acuity with refraction § Monitor the effect of treatment and/or progression of disease § Estimate the dioptric power of optical devices necessary for reading regular size print § Verify eligibility for tasks such as driving § Verify eligibility as “legally blind” When measuring distance acuity, there is no longer a need to measure visual acuity in a darkened room. In the past, when projected charts were used, the room lights had to be lowered for better contrast on the chart. Now, with high definition LCD monitor acuity charts and ETDRS charts, contrast is no longer an issue. Additionally, for some patients, particularly those with difficulties adjusting to lower lighting conditions, taking them from a normally lit waiting room into a darkened clinic or work up room will artificially lower their acuity, because they do not have enough time for their eyes to adjust to the lower light conditions. Because clinical decisions are based on these acuity measurements, accurate assessment of each person’s acuity is critically important. With this in mind, all acuity testing should be done with the overhead lights on in the exam or work up room.