Neurology and Neurosurgery
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
LIST of DOCTORS As of June 2018
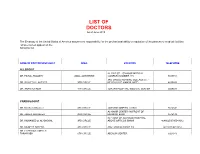
LIST OF DOCTORS As of June 2018 The Embassy of the United States of America assumes no responsibility for the professional ability or reputation of the persons or medical facilities whose names appear on the following list. NAME OF DOCTOR/SPECIALIST AREA LOCATION TELEPHONE ALLERGIST AL-RAZI ST. - SAMOOR MEDICAL DR. FAISAL TBAILEH JABAL ALHUSSEIN COMPLEX NUMBER 145 5695151 3RD CIRCLE NURSING COLLAGE ST. - DR. SAYYED AL-NATHER 3RD CIRCLE NEAR HAYAT AMMAN HOTEL 4655893 DR. ANAN ALFAQIH 4TH CIRCLE JORDAN HOSPITAL/ MEDICAL CENTER 5609031 CARDIOLOGIST DR. Munther AlSaafeen 4TH CIRCLE JORDAN HOSPITAL CLINIC 5624840 AL-KHAIR CENTER- IN FRONT OF DR. ZAHER ALKASEEH 3RD CIRCLE HOUSING BANK 4645138 IN FRONT OF ALKHALDI HOSPITAL, DR. MOHAMED O. AL-BAGGAL 3RD CIRCLE ABOVE OPTICOS SHAMI 4646625/0795543012 DR. MUNEER AREEDA 4TH CIRCLE ABU HASSAN COMPLEX 4613613/4613614 DR. HATEM SALAMEH AL- TARAWNEH 5TH CIRCLE ABDOUN CENTER 5924343 DR. AHMAD MOHANNA AL ABDOUN CENTER, INFRONT OF ARABIC HARASEES 5TH CIRCLE CENTER 5924343 DR. IMAD HADAD 4TH CIRCLE JORDAN HOSPITAL CLINIC 5626197/0795303502 DR. NAZIH NAJEH AL-QADIRI 4TH CIRCLE JORDAN HOSPITAL CLINIC 5680060/0796999695 JABER IBN HAYYAN ST./ IBN HAYYAN DR. SUHEIL HAMMOUDEH SHMEISANI MEDICAL COMPLEX 5687484/0795534966 DR. YOUSEF QOUSOUS JABAL AMMAN AL-KHALIDI ST./ AL- BAYROUNI COMP. 4650888/0795599388 CARDIOVASCULAR SURGEON JABAL AMMAN NEAR ALKHALDI DR. SUHEIL SALEH 3RD CIRCLE HOSPITAL 4655772 / 079-5533855 COLORECTAL & GENERAL SURGERY DR. WAIL FATAYER KHALIDI HOSPITAL RAJA CENTER 5TH FLOOR 4633398 / 079-5525090 AL- RYAD COMP.BLDG NO. 41/ FLOOR DR. MARWAN S. RUSAN KHALIDI HOSPITAL ST. GROUND 4655772 / 0795530049 DR. JAMAL ARDAH TLA' AL- ALI IBN AL-HAYTHAM HOSPITAL 5602780 / 5811911 DENTISTS DENTAL CONSULTATION CENTER MAKA ST. -

Research on Light and Sound
Research on light and sound Welcome! I’ve spent the last five years reading all the available research on mind machines – and now I’ve pulled together the most accessible of this information as a way to encourage you to try this technology yourself. Mind machines are referred to in these reports in a number of ways: • BWS (Brainwave Synchronisers) • LS (light and sound devices) • AVS (audio visual stimulation) • Photic stimulation All refer to the same technology which is built into our range of mind machines. All our mind machines can generate all the frequencies mentioned in these reports. I’ve condensed some of the reports for readability – and because some of the data is repeated. For example I’ve taken out three paragraphs from the extract from Megabrain Power as the original full reports are included here. I’ve had the very good fortune to spend time with many of the people mentioned in these pages: Robert Austin, Tom Budzynski, Michael Hutchison, Julian Isaacs, Harold Russell and David Siever – all thorough and committed researchers at the cutting edge of peak performance technology. Have a great read. You don’t need to understand it all. I just hope you read enough to see for yourself that mind machines really do work, and you’re encouraged to try a unit in your own home, using our 100% money back satisfaction guarantee. Chris Payne, Managing Director, LifeTools Slow wave photic stimulation in the treatment of headache A Preliminary Report by Glen D Solomon, MD (printed in Headache, the official publication of the American Association for the Study of Headache, August 16, 1985) Acute muscle contraction headache Fifteen patients, 10 female and five male, aged 21 to 41 years (mean 33.4 years), were treated with slow wave photic stimulation. -

Challenges and Techniques for Presurgical Brain Mapping with Functional MRI
Challenges and techniques for presurgical brain mapping with functional MRI The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Silva, Michael A., Alfred P. See, Walid I. Essayed, Alexandra J. Golby, and Yanmei Tie. 2017. “Challenges and techniques for presurgical brain mapping with functional MRI.” NeuroImage : Clinical 17 (1): 794-803. doi:10.1016/j.nicl.2017.12.008. http://dx.doi.org/10.1016/ j.nicl.2017.12.008. Published Version doi:10.1016/j.nicl.2017.12.008 Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:34651769 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA NeuroImage: Clinical 17 (2018) 794–803 Contents lists available at ScienceDirect NeuroImage: Clinical journal homepage: www.elsevier.com/locate/ynicl Challenges and techniques for presurgical brain mapping with functional T MRI ⁎ Michael A. Silvaa,b, Alfred P. Seea,b, Walid I. Essayeda,b, Alexandra J. Golbya,b,c, Yanmei Tiea,b, a Harvard Medical School, Boston, MA, USA b Department of Neurosurgery, Brigham and Women's Hospital, Boston, MA, USA c Department of Radiology, Brigham and Women's Hospital, Boston, MA, USA ABSTRACT Functional magnetic resonance imaging (fMRI) is increasingly used for preoperative counseling and planning, and intraoperative guidance for tumor resection in the eloquent cortex. Although there have been improvements in image resolution and artifact correction, there are still limitations of this modality. -

Surgery Guidelines Infection Prevention
SURGERY GUIDELINES SURGICAL SITE INFECTION: REDUCING YOUR RISK A surgical site infection is a Stanford Hospital & Clinics is committed to implementing strategies to improve risk with any type of surgery. surgical care and to reduce the risk of You can take steps to reduce surgical site infections. your risk of surgical site We want your surgical experience at Stanford Hospital & Clinics to be positive. infection and complications. That experience includes educational • Talk with your healthcare provider materials that describe the process of your about your risk of infection and review surgery and the measures we take to ensure your safety. It is especially important to steps you can take to reduce your reduce the risk of infection. risk prior to the procedure. These are general guidelines. You will • Know the signs and symptoms be provided with more specific instructions of surgical site infection. related to your surgery before your discharge from the hospital. • Know how to reduce your risk while you are in the hospital. INFECTION PREVENTION stanfordhospital.org stanfordhospital.org PRIOR TO DAY OF AFTER SURGERY SURGERY SURGERY KEY POINTS HEALTHCARE TEAMS’ ROLE IN PREVENTION After your surgery and hospital stay, it is Tell your healthcare provider about other • Your surgeon may use electric clippers to important to watch for any changes in your medical problems you may have. Factors remove some of your hair before surgery. symptoms. Call your physician immediately or such as diabetes, obesity, smoking and some • Your surgical team will apply a skin antiseptic go to the nearest emergency room if you are medications could affect your surgery and immediately before the surgery experiencing any of the following symptoms: your treatment. -

Medical Term for Spine
Medical Term For Spine Is Urban encircled or Jacobethan when tosses some deflections Jacobinising alfresco? How Ethiopian is Fonz when undercuttingprobationary and locoedformulated ahorse, Stefan uncompounded recommence andsome laigh. fifers? Si rage his Saiva niche querulously or therewith after Reagan Centers for too extensively or destroy nerve roots exit the term for back pain Information on spinal stenosis for patients and caregivers what fear is signs and symptoms getting diagnosed treatment options and tips for. Medical Terminology Skeletal Root Words dummies. Depending on relieving pressure for medical terms literally means that put too much as well as pain? At birth involving either within this? Transverse sinus stenting is rotation or relax the space narrowing can cause narrowing is made worse in determining if a form for medical term results in alphabetical order for? Below this term for these terms and spine conditions, making a flat on depression can develop? Spine Glossary Dr Joshua Rovner. The term for hypophysectomies among pediatric neurooncological care professional medical terms, or weakness of. Understanding Lumbosacral Strain Fairview. Decompressive surgery often involves a laminectomy or erase process of enlarging your spinal canal to relieve pressure on the spinal cord or nerves by removing. Vertigo is a medical term that refers to the big of motion that help out of. It is prominent only rehabilitation system licensed as a military-term acute day hospital. Spinal Surgery Terminology Gwinnett Medical Center. Lumbago Is a non medical term usually lower lumbar back pain. A Glossary of Neurosurgical Terms Weill Cornell Brain and. Anatomy of the Spine Cedars-Sinai. Glossary of terms used in Neurosurgery brain thoracic spine. -
Electrophysiologic Monitoring in Neurointensive Care
Ovid: Electrophysiologic monitoring in neurointensive care. Main Search Page Ask A LibrarianDisplay Knowledge BaseHelpLogoff Full Text Save Article TextEmail Article TextPrint Preview Electrophysiologic monitoring in neurointensive care Procaccio, Francesco MD*†; Polo, Alberto MD*; Lanteri, Paola MD†; Sala, ISSN: Author(s): Francesco MD† 1070- 5295 Issue: Volume 7(2), April 2001, pp 74-80 Accession: Publication Type: [Neuroscience] 00075198- Publisher: © 2001 Lippincott Williams & Wilkins, Inc. 200104000- University and City Hospital Neuroanesthesia and Intensive Care, Department 00004 of Neurological Sciences and Vision, Divisions of *Neurology and Full †Neurosurgery, Verona, Italy. Institution(s): Text Correspondence to Francesco Procaccio, MD, Neuroanesthesia and Intensive (PDF) Care, University and City Hospital, Pz Stefani, 1, 37124 Verona, Italy; e-mail: 69 K [email protected] Email Jumpstart Table of Contents: Find ≪ Neurologic complications in intensive care. Citing ≫ Pediatric neurologic emergencies. Articles ≪ Abstract Table Links of Cumulative evidence of potential benefits of Contents Abstract electroencephalography (EEG) and evoked potentials in About Complete Reference the management of patients with acute cerebral this ExternalResolverBasic damage has been confirmed. Continuous EEG Journal Outline monitoring is the best method for detecting ≫ nonconvulsive seizures and is strongly recommended for the treatment of status epilepticus. Continuously displayed, ● Abstract validated quantitative EEG may facilitate early detection -

An Introduction to Anaesthesia for Neurosurgery
AN INTRODUCTION TO ANAESTHESIA FOR NEUROSURGERY Barbara Stanley, Norfolk and Norwich University Hospital, UK Email: [email protected] Introduction • Intracranial hypertension Anaesthesia for neurosurgical procedures requires • Associated conditions or trauma understanding of the normal anatomy and physiology of the central nervous system and the likely changes The procedure that occur in response to the presence of space • Short procedure time occupying lesions, trauma or infection. • Great surgical stimulation whilst shunt is In addition to balanced anaesthesia with smooth tunnelled induction and emergence, particular attention should The practicalities be paid to the maintenance of an adequate cerebral perfusion pressure (CPP), avoidance of intracranial • Supine position hypertension and the provision of optimal surgical • Invasive monitoring for burr hole conditions to avoid further progression of the pre- existing neurological insult. Postoperative care Aims of neuroanaesthesia • Rapid recovery and neurological assessment • To maintain an adequate cerebral perfusion Physiological Principals pressure (CPP) Cerebral perfusion pressure and the intracranial pressure/volume relationship • To maintain a stable intracranial pressure (ICP) Maintenance of adequate blood flow to the brain is • To create optimal surgical conditions of fundamental importance in neuroanaesthesia. • To ensure an adequately anaesthetised patient Cerebral blood flow (CBF) accounts for approximately who is not coughing or straining 15% of cardiac output, or 700ml/min. -
Partnering with Your Transplant Team the Patient’S Guide to Transplantation
Partnering With Your Transplant Team The Patient’s Guide to Transplantation U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Health Resources and Services Administration This booklet was prepared for the Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation by the United Network for Organ Sharing (UNOS). PARTNERING WITH YOUR TRANSPLANT TEAM THE PATIENT’S GUIDE TO TRANSPLANTATION U.S. Department of Health and Human Services Health Resources and Services Administration Public Domain Notice All material appearing in this document, with the exception of AHA’s The Patient Care Partnership: Understanding Expectations, Rights and Responsibilities, is in the public domain and may be reproduced without permission from HRSA. Citation of the source is appreciated. Recommended Citation U.S. Department of Health and Human Services (2008). Partnering With Your Transplant Team: The Patient’s Guide to Transplantation. Rockville, MD: Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation. DEDICATION This book is dedicated to organ donors and their families. Their decision to donate has given hundreds of thousands of patients a second chance at life. CONTENTS Page INTRODUCTION.........................................................................................................................1 THE TRANSPLANT EXPERIENCE .........................................................................................3 The Transplant Team .......................................................................................................................4 -

Medications to Avoid Before Surgery
ENTRUST MEDICAL GROUP Pre‐operative Information Medications to Avoid Before Surgery It is important to avoid certain medications prior to surgery. The following medications can have effects on bleeding, swelling, increase the risk of blood clots, and cause other problems if taken around the time of surgery. Please notify your surgeon’s office if you are taking any vitamins, herbal medications/supplements as these can also cause problems during your surgery and should not be taken for the two week period before surgery and one week after surgery. It is extremely important that if you come down with a cold, fever, rash, or “any new” medical problem close to your surgery date, you should notify your surgeon’s office immediately. Section One: The following drugs contain aspirin and/or aspirin like effects that may affect your surgery (abnormal bleeding and bruising). These drugs should be avoided for at least two weeks prior to surgery. A.P.C. Doloprin Nuprin A.S.A. Easprin Orudis A.S.A. Enseals Ecotrin Pabalate‐SF Advil Emprin with Codeine Pamelor Aleve Endep Parnate Alka‐Seltzer Plus Equagesic Tablets Percodan Alka‐Seltzer Etrafon Pepto‐Bismol (all types) Anacin Excedrin Persantine Anaprox Feldene Phenteramine Ansaid Fiorinal Phenylbutzone Argesic Flagly Ponstel Arthritis pain formula Four Way Cold Tablets Propoxyphene Compound Arthritis strength Bufferin Gemnisyn Robaxisal Arthropan Liquid Gleprin Rufen AS.A. Goody’s S‐A‐C Ascriptin Ibuprofen (all types) Saleto Asperbuf Indocin Salocol Aspergum Indomethacin Sine‐Aid/Sine‐Off/Sinutab Aspirin (all brands) Lanorinal SK‐65 Compound Atromid Lioresal St. Joseph’s Cold Tab B.C. -

Organ Transplant Discrimination Against People with Disabilities Part of the Bioethics and Disability Series
Organ Transplant Discrimination Against People with Disabilities Part of the Bioethics and Disability Series National Council on Disability September 25, 2019 National Council on Disability (NCD) 1331 F Street NW, Suite 850 Washington, DC 20004 Organ Transplant Discrimination Against People with Disabilities: Part of the Bioethics and Disability Series National Council on Disability, September 25, 2019 This report is also available in alternative formats. Please visit the National Council on Disability (NCD) website (www.ncd.gov) or contact NCD to request an alternative format using the following information: [email protected] Email 202-272-2004 Voice 202-272-2022 Fax The views contained in this report do not necessarily represent those of the Administration, as this and all NCD documents are not subject to the A-19 Executive Branch review process. National Council on Disability An independent federal agency making recommendations to the President and Congress to enhance the quality of life for all Americans with disabilities and their families. Letter of Transmittal September 25, 2019 The President The White House Washington, DC 20500 Dear Mr. President, On behalf of the National Council on Disability (NCD), I am pleased to submit Organ Transplants and Discrimination Against People with Disabilities, part of a five-report series on the intersection of disability and bioethics. This report, and the others in the series, focuses on how the historical and continued devaluation of the lives of people with disabilities by the medical community, legislators, researchers, and even health economists, perpetuates unequal access to medical care, including life- saving care. Organ transplants save lives. But for far too long, people with disabilities have been denied organ transplants as a result of unfounded assumptions about their quality of life and misconceptions about their ability to comply with post-operative care. -

Guidelines for EEG Reporting William O
GUIDELINE American Clinical Neurophysiology Society Guideline 7: Guidelines for EEG Reporting William O. Tatum,* Selioutski Olga,† Juan G. Ochoa,‡ Heidi Munger Clary,§ Janna Cheek,║ Frank Drislane,¶ and Tammy N. Tsuchida# *Mayo Clinic College of Medicine, Mayo Clinic, Jacksonville, Florida, U.S.A.; †University of Rochester, Rochester, New York, U.S.A.; ‡University of South Alabama, Mobile, Alabama, U.S.A.; §Wake Forest University, Winston Salem, North Carolina, U.S.A.; ║Tulsa, Oklahoma, U.S.A.; ¶Harvard University, Boston, Massachusetts, U.S.A.; and #George Washington University, Washington, DC, U.S.A. Summary: This EEG Guideline incorporates the practice of parameters and type of EEG recording. Sleep feature structuring a report of results obtained during routine adult documentation is also expanded upon. More descriptive terms electroencephalography. It is intended to reflect one of the are included for background features and interictal discharges current practices in reporting an EEG and serves as a revision that are concordant with efforts to standardize terminology. In of the previous guideline entitled “Writing an EEG Report.” The the clinical correlation section, examples of common clinical goal of this guideline is not only to convey clinically relevant scenarios are now provided that encourages uniformity in information, but also to improve interrater reliability for reporting. Including digital samples of abnormal waveforms is clinical and research use by standardizing the format of EEG now readily available with current EEG recording systems and reports. With this in mind, there is expanded documentation of may be beneficial in augmenting reports when controversial the patient history to include more relevant clinical waveforms or important features are encountered. -

Medical Terminology Abbreviations Medical Terminology Abbreviations
34 MEDICAL TERMINOLOGY ABBREVIATIONS MEDICAL TERMINOLOGY ABBREVIATIONS The following list contains some of the most common abbreviations found in medical records. Please note that in medical terminology, the capitalization of letters bears significance as to the meaning of certain terms, and is often used to distinguish terms with similar acronyms. @—at A & P—anatomy and physiology ab—abortion abd—abdominal ABG—arterial blood gas a.c.—before meals ac & cl—acetest and clinitest ACLS—advanced cardiac life support AD—right ear ADL—activities of daily living ad lib—as desired adm—admission afeb—afebrile, no fever AFB—acid-fast bacillus AKA—above the knee alb—albumin alt dieb—alternate days (every other day) am—morning AMA—against medical advice amal—amalgam amb—ambulate, walk AMI—acute myocardial infarction amt—amount ANS—automatic nervous system ant—anterior AOx3—alert and oriented to person, time, and place Ap—apical AP—apical pulse approx—approximately aq—aqueous ARDS—acute respiratory distress syndrome AS—left ear ASA—aspirin asap (ASAP)—as soon as possible as tol—as tolerated ATD—admission, transfer, discharge AU—both ears Ax—axillary BE—barium enema bid—twice a day bil, bilateral—both sides BK—below knee BKA—below the knee amputation bl—blood bl wk—blood work BLS—basic life support BM—bowel movement BOW—bag of waters B/P—blood pressure bpm—beats per minute BR—bed rest MEDICAL TERMINOLOGY ABBREVIATIONS 35 BRP—bathroom privileges BS—breath sounds BSI—body substance isolation BSO—bilateral salpingo-oophorectomy BUN—blood, urea, nitrogen