Molecular Engineering of Therapeutic Cytokines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Current Therapies for Chronic Hepatitis C
Southern Illinois University Edwardsville SPARK Pharmacy Faculty Research, Scholarship, and Creative Activity School of Pharmacy 1-2011 Current Therapies for Chronic Hepatitis C McKenzie C. Ferguson Southern Illinois University Edwardsville, [email protected] Follow this and additional works at: https://spark.siue.edu/pharmacy_fac Part of the Pharmacy and Pharmaceutical Sciences Commons Recommended Citation Ferguson, McKenzie C., "Current Therapies for Chronic Hepatitis C" (2011). Pharmacy Faculty Research, Scholarship, and Creative Activity. 4. https://spark.siue.edu/pharmacy_fac/4 This Article is brought to you for free and open access by the School of Pharmacy at SPARK. It has been accepted for inclusion in Pharmacy Faculty Research, Scholarship, and Creative Activity by an authorized administrator of SPARK. For more information, please contact [email protected],[email protected]. Chronic Hepatitis C & Current Therapies 1 Review of Chronic Hepatitis C & Current Therapies Reviews of Therapeutics Pharmacotherapy McKenzie C. Ferguson, Pharm.D., BCPS From the School of Pharmacy, Southern Illinois University Edwardsville, Department of Pharmacy Practice, Edwardsville, Illinois. Address for reprint requests : Southern Illinois University Edwardsville School of Pharmacy 220 University Park Drive, Ste 1037 Edwardsville, IL 62026-2000 Email: [email protected] Keywords : hepatitis C, HCV, ribavirin, interferon, peginterferon alfa-2a, peginterferon alfa-2b, albinterferon, taribavirin, telaprevir, therapeutic efficacy, safety The author received no sources of support in the form of grants, equipment, or drugs. Chronic Hepatitis C & Current Therapies 2 ABSTRACT Hepatitis C virus affects more than 180 million people worldwide and as many as 4 million people in the United States. Given that most patients are asymptomatic until late in disease progression, diagnostic screening and evaluation of patients that display high-risk behaviors associated with acquisition of hepatitis C should be performed. -

Cytokine Nomenclature
RayBiotech, Inc. The protein array pioneer company Cytokine Nomenclature Cytokine Name Official Full Name Genbank Related Names Symbol 4-1BB TNFRSF Tumor necrosis factor NP_001552 CD137, ILA, 4-1BB ligand receptor 9 receptor superfamily .2. member 9 6Ckine CCL21 6-Cysteine Chemokine NM_002989 Small-inducible cytokine A21, Beta chemokine exodus-2, Secondary lymphoid-tissue chemokine, SLC, SCYA21 ACE ACE Angiotensin-converting NP_000780 CD143, DCP, DCP1 enzyme .1. NP_690043 .1. ACE-2 ACE2 Angiotensin-converting NP_068576 ACE-related carboxypeptidase, enzyme 2 .1 Angiotensin-converting enzyme homolog ACTH ACTH Adrenocorticotropic NP_000930 POMC, Pro-opiomelanocortin, hormone .1. Corticotropin-lipotropin, NPP, NP_001030 Melanotropin gamma, Gamma- 333.1 MSH, Potential peptide, Corticotropin, Melanotropin alpha, Alpha-MSH, Corticotropin-like intermediary peptide, CLIP, Lipotropin beta, Beta-LPH, Lipotropin gamma, Gamma-LPH, Melanotropin beta, Beta-MSH, Beta-endorphin, Met-enkephalin ACTHR ACTHR Adrenocorticotropic NP_000520 Melanocortin receptor 2, MC2-R hormone receptor .1 Activin A INHBA Activin A NM_002192 Activin beta-A chain, Erythroid differentiation protein, EDF, INHBA Activin B INHBB Activin B NM_002193 Inhibin beta B chain, Activin beta-B chain Activin C INHBC Activin C NM005538 Inhibin, beta C Activin RIA ACVR1 Activin receptor type-1 NM_001105 Activin receptor type I, ACTR-I, Serine/threonine-protein kinase receptor R1, SKR1, Activin receptor-like kinase 2, ALK-2, TGF-B superfamily receptor type I, TSR-I, ACVRLK2 Activin RIB ACVR1B -

Kate Fitzgerald
In This Issue: 2020 Young Investigator Awardees pg. 3-9 In Memorium page pg. 14-15 New Member Mini-Bios pg. 19-21 Trials of Interferon Lambda pg. 31 Cytokines 2021 Hybrid Meetin pg. 24-27 Signals THE INTERNATIONAL CYTOKINE & INTERFERON SOCIETY + NEWSLETTER APRIL 2021 I VOLUME 9 I NO. 1 A NOTE FROM THE ICIS PRESIDENT Kate Fitzgerald Dear Colleagues, Greetings from the International Cytokine and Interferon Society! I hope you and your family are staying safe during these still challenging times. Thankfully 2020 is behind us now. We have lived through the COVID-19 pandemic, an event that will continue to impact our lives for some time and likely alter how we live in the future. Despite the obvious difficulties of this past year, I can’t help but marvel at the scientific advances that have been made. With everything from COVID-19 testing, to treatments and especially to the rapid pace of vaccine development, we are so better off today than even a few months back. The approval of remarkably effective COVID-19 vaccines now rolling out in the US, Israel, UK, Europe and across the globe, brings light at the end of the tunnel. The work of many of you has helped shape our understanding of the host response to Sars-CoV2 and the ability of this virus to limit antiviral immunity while simultaneously driving a cytokine driven hyperinflammatory response leading to deadly consequences for patients. The knowledge gained from all of your efforts has been put to good use to stem the threat of this deadly virus. -

THE CONCISE GUIDE to PHARMACOLOGY 2017/18 Alexander, Stephen P
University of Dundee THE CONCISE GUIDE TO PHARMACOLOGY 2017/18 Alexander, Stephen P. H.; Fabbro, Doriano; Kelly, Eamonn; Marrion, Neil V.; Peters, John A.; Faccenda, Elena Published in: British Journal of Pharmacology DOI: 10.1111/bph.13876 Publication date: 2017 Licence: CC BY Document Version Publisher's PDF, also known as Version of record Link to publication in Discovery Research Portal Citation for published version (APA): Alexander, S. P. H., Fabbro, D., Kelly, E., Marrion, N. V., Peters, J. A., Faccenda, E., Harding, S. D., Pawson, A. J., Sharman, J. L., Southan, C., Davies, J. A., & CGTP Collaborators (2017). THE CONCISE GUIDE TO PHARMACOLOGY 2017/18: Catalytic receptors. British Journal of Pharmacology, 174 (Suppl. 1), S225-S271. https://doi.org/10.1111/bph.13876 General rights Copyright and moral rights for the publications made accessible in Discovery Research Portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from Discovery Research Portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain. • You may freely distribute the URL identifying the publication in the public portal. Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Download date: 23. Sep. 2021 S.P.H. -

Pulmonary Delivery of Biological Drugs
pharmaceutics Review Pulmonary Delivery of Biological Drugs Wanling Liang 1,*, Harry W. Pan 1 , Driton Vllasaliu 2 and Jenny K. W. Lam 1 1 Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, 21 Sassoon Road, Pokfulam, Hong Kong, China; [email protected] (H.W.P.); [email protected] (J.K.W.L.) 2 School of Cancer and Pharmaceutical Sciences, King’s College London, 150 Stamford Street, London SE1 9NH, UK; [email protected] * Correspondence: [email protected]; Tel.: +852-3917-9024 Received: 15 September 2020; Accepted: 20 October 2020; Published: 26 October 2020 Abstract: In the last decade, biological drugs have rapidly proliferated and have now become an important therapeutic modality. This is because of their high potency, high specificity and desirable safety profile. The majority of biological drugs are peptide- and protein-based therapeutics with poor oral bioavailability. They are normally administered by parenteral injection (with a very few exceptions). Pulmonary delivery is an attractive non-invasive alternative route of administration for local and systemic delivery of biologics with immense potential to treat various diseases, including diabetes, cystic fibrosis, respiratory viral infection and asthma, etc. The massive surface area and extensive vascularisation in the lungs enable rapid absorption and fast onset of action. Despite the benefits of pulmonary delivery, development of inhalable biological drug is a challenging task. There are various anatomical, physiological and immunological barriers that affect the therapeutic efficacy of inhaled formulations. This review assesses the characteristics of biological drugs and the barriers to pulmonary drug delivery. -

Interferon-Based Biopharmaceuticals: Overview on the Production, Purification, and Formulation
Review Interferon-Based Biopharmaceuticals: Overview on the Production, Purification, and Formulation Leonor S. Castro 1,†, Guilherme S. Lobo 1,†, Patrícia Pereira 2 , Mara G. Freire 1 ,Márcia C. Neves 1,* and Augusto Q. Pedro 1,* 1 CICECO–Aveiro Institute of Materials, Chemistry Department, University of Aveiro, Campus Universitário de Santiago, 3810-193 Aveiro, Portugal; [email protected] (L.S.C.); [email protected] (G.S.L.); [email protected] (M.G.F.) 2 Centre for Mechanical Engineering, Materials and Processes, Department of Chemical Engineering, University of Coimbra, Rua Sílvio Lima-Polo II, 3030-790 Coimbra, Portugal; [email protected] * Correspondence: [email protected] (M.C.N.); [email protected] (A.Q.P.) † These authors contributed equally to this work. Abstract: The advent of biopharmaceuticals in modern medicine brought enormous benefits to the treatment of numerous human diseases and improved the well-being of many people worldwide. First introduced in the market in the early 1980s, the number of approved biopharmaceutical products has been steadily increasing, with therapeutic proteins, antibodies, and their derivatives accounting for most of the generated revenues. The success of pharmaceutical biotechnology is closely linked with remarkable developments in DNA recombinant technology, which has enabled the production of proteins with high specificity. Among promising biopharmaceuticals are interferons, first described by Isaacs and Lindenmann in 1957 and approved for clinical use in humans nearly thirty years later. Interferons are secreted autocrine and paracrine proteins, which by regulating several biochemical Citation: Castro, L.S.; Lobo, G.S.; pathways have a spectrum of clinical effectiveness against viral infections, malignant diseases, Pereira, P.; Freire, M.G.; Neves, M.C.; and multiple sclerosis. -

Quantum of Effectiveness Evidence in FDA's Approval of Orphan Drugs
Quantum of Effectiveness Evidence in FDA’s Approval of Orphan Drugs Cataloguing FDA’s Flexibility in Regulating Therapies for Persons with Rare Disorders by Frank J. Sasinowski, M.S., M.P.H., J.D.1 Chairman of the Board National Organization for Rare Disorders One of the key underlying issues facing the development of effective for their intended uses. all drugs, and particularly orphan drugs, is what kind of evi- dence the Food and Drug Administration (FDA) requires for FDA has for many decades acknowledged that there is a need approval. The Federal Food, Drug, and Cosmetic [FD&C] Act IRUÁH[LELOLW\LQDSSO\LQJLWVVWDQGDUGIRUDSSURYDO)RUH[- provides that for FDA to grant approval for a new drug, there ample, one of FDA’s regulations states that: “FDA will ap- must be “substantial evidence” of effectiveness derived from prove an application after it determines that the drug meets the “adequate and well-controlled investigations.” This language, statutory standards for safety and effectiveness… While the which dates from 1962, provides leeway for FDA medical re- statutory standards apply to all drugs, the many kinds of drugs viewers to make judgments as to what constitutes “substantial that are subject to the statutory standards and the wide range HYLGHQFHµRIDGUXJ·VHIIHFWLYHQHVVWKDWLVRILWVEHQHÀWWR RIXVHVIRUWKRVHGUXJVGHPDQGÁH[LELOLW\LQDSSO\LQJWKHVWDQ- patients. GDUGV7KXV)'$LVUHTXLUHGWRH[HUFLVHLWVVFLHQWLÀFMXGJPHQW to determine the kind and quantity of data and information an 7KHVROHODZWKDWDSSOLHVVSHFLÀFDOO\WRRUSKDQGUXJVWKH2U- applicant is required to provide for a particular drug to meet SKDQ'UXJ$FWRISURYLGHGÀQDQFLDOLQFHQWLYHVIRUGUXJ the statutory standards.” 21 C.F.R. § 314.105(c). FRPSDQLHVWRGHYHORSRUSKDQGUXJVZKLFKLVOHJDOO\GHÀQHG as products that treat diseases that affect 200,000 or fewer )'$SXEOLFO\KDVH[SUHVVHGVHQVLWLYLW\WRDSSO\LQJWKLVÁH[- patients in the U.S. -

Novel Therapies for Eosinophilic Disorders
Novel Therapies for Eosinophilic Disorders Bruce S. Bochner, MD KEYWORDS Eosinophil Therapies Antibodies Targets Pharmacology Biomarkers KEY POINTS A sizable unmet need exists for new, safe, selective, and effective treatments for eosinophil-associated diseases, such as hypereosinophilic syndrome, eosinophilic gastrointestinal disorders, nasal polyposis, and severe asthma. An improved panel of biomarkers to help guide diagnosis, treatment, and assessment of disease activity is also needed. An impressive array of novel therapeutic agents, including small molecules and biologics, that directly or indirectly target eosinophils and eosinophilic inflammation are undergoing controlled clinical trials, with many already showing promising results. A large list of additional eosinophil-related potential therapeutic targets remains to be pursued, including cell surface structures, soluble proteins that influence eosinophil biology, and eosinophil-derived mediators that have the potential to contribute adversely to disease pathophysiology. INTRODUCTION Eosinophilic disorders, also referred to as eosinophil-associated diseases, consist of a range of infrequent conditions affecting virtually any body compartment and organ.1 The most commonly affected areas include the bone marrow, blood, mucosal sur- faces, and skin, often with immense disease- and treatment-related morbidity, Disclosure Statement: Dr Bochner’s research efforts are supported by grants AI072265, AI097073 and HL107151 from the National Institutes of Health. He has current or recent consul- ting or scientific advisory board arrangements with, or has received honoraria from, Sanofi-A- ventis, Pfizer, Svelte Medical Systems, Biogen Idec, TEVA, and Allakos, Inc. and owns stock in Allakos, Inc. and Glycomimetics, Inc. He receives publication-related royalty payments from Elsevier and UpToDate and is a coinventor on existing and pending Siglec-8-related patents and, thus, may be entitled to a share of future royalties received by Johns Hopkins University on the potential sales of such products. -

The Cytokine Network in Asthma and Chronic Obstructive Pulmonary Disease
The cytokine network in asthma and chronic obstructive pulmonary disease Peter J. Barnes J Clin Invest. 2008;118(11):3546-3556. https://doi.org/10.1172/JCI36130. Review Series Asthma and chronic obstructive pulmonary disease (COPD) are very common inflammatory diseases of the airways. They both cause airway narrowing and are increasing in incidence throughout the world, imposing enormous burdens on health care. Cytokines play a key role in orchestrating the chronic inflammation and structural changes of the respiratory tract in both asthma and COPD and have become important targets for the development of new therapeutic strategies in these diseases. Find the latest version: https://jci.me/36130/pdf Review series The cytokine network in asthma and chronic obstructive pulmonary disease Peter J. Barnes National Heart & Lung Institute, Imperial College London, London, United Kingdom. Asthma and chronic obstructive pulmonary disease (COPD) are very common inflammatory diseases of the air- ways. They both cause airway narrowing and are increasing in incidence throughout the world, imposing enormous burdens on health care. Cytokines play a key role in orchestrating the chronic inflammation and structural changes of the respiratory tract in both asthma and COPD and have become important targets for the development of new therapeutic strategies in these diseases. Introduction Inflammation in asthma and COPD The most common inflammatory diseases of the airways are Despite the similarity of some clinical features of asthma and asthma and chronic obstructive pulmonary disease (COPD), COPD, there are marked differences in the pattern of inflamma- and the incidence of both is increasing throughout the world. tion in the respiratory tract, with different inflammatory cells, The prevalence of asthma in developed countries is approxi- mediators, consequences, and responses to therapy (1). -

Importance of Cytokines in Murine Allergic Airway Disease and Human Asthma Fred D
Importance of Cytokines in Murine Allergic Airway Disease and Human Asthma Fred D. Finkelman, Simon P. Hogan, Gurjit K. Khurana Hershey, Marc E. Rothenberg and Marsha Wills-Karp This information is current as of September 29, 2021. J Immunol 2010; 184:1663-1674; ; doi: 10.4049/jimmunol.0902185 http://www.jimmunol.org/content/184/4/1663 Downloaded from References This article cites 257 articles, 63 of which you can access for free at: http://www.jimmunol.org/content/184/4/1663.full#ref-list-1 Why The JI? Submit online. http://www.jimmunol.org/ • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average by guest on September 29, 2021 Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2010 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Importance of Cytokines in Murine Allergic Airway Disease and Human Asthma ,†,‡ x { Fred D. Finkelman,*x Simon P. Hogan, Gurjit K. Khurana Hershey, Marc E. Rothenberg, and Marsha Wills-Karp‡ Asthma is a common, disabling inflammatory respira- lymphocytosis and mastocytosis; alternative macrophage ac- tory disease that has increased in frequency and severity tivation; epithelial cell proliferation with goblet cell hyper- in developed nations. -
NMMC West Point CDM.Xlsx
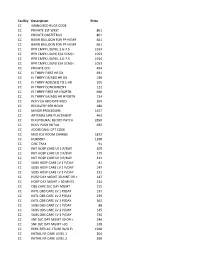
Facility Description Price CC SWING BED RUGS CODE CC PRIVATE 1ST WEST 861 CC PRIVATE OBSTETRICS 861 CC BAKRI BALLOON FOR PP HEMR 661 CC BAKRI BALLOON FOR PP HEMR 661 CC RPR CMPX LID/N/L 2.6‐7.5 1914 CC RPR CMPX LID/N/ E/A 5CM/< 1053 CC RPR CMPX LID/N/L 2.6‐7.5 1914 CC RPR CMPX LID/N/ E/A 5CM/< 1053 CC PRIVATE ECU 494 CC IV THRPY FIRST HR DX 691 CC IV THRPY EA/ADD HR DX 190 CC IV THRPY ADD/SEQ TO 1 HR 205 CC IV THRPY CONCURRENT 122 CC IV THRPY FIRST HR HYDRTN 690 CC IV THRPY EA/ADD HR HYDRTN 134 CC INJ IV EA ADD DIFF MED 269 CC RECOVERY PER HOUR 280 CC MINOR PROCEDURE 1627 CC ARTERIAL LINE PLACEMENT 463 CC INJ EPIDURAL BLOOD PATCH 2850 CC INJ IV PUSH INITIAL 692 CC ADDITIONAL CPT CODE CC MED ICU ROOM CHARGE 1872 CC NURSERY 1200 CC CIRC TRAY 91 CC INIT HOSP CARE LV 1 P/DAY 205 CC INIT HOSP CARE LV 2 P/DAY 279 CC INIT HOSP CARE LV 3 P/DAY 412 CC SUBS HOSP CARE LV 1 P/DAY 81 CC SUBS HOSP CARE LV 2 P/DAY 147 CC SUBS HOSP CARE LV 3 P/DAY 212 CC HOSP DAY MGMT 30 MNT OR < 147 CC HOSP DAY MGMT > 30 MNTS 214 CC OBS CARE D/C DAY MGMT 155 CC INITL OBS CARE LV 1 P/DAY 197 CC INITL OBS CARE LV 2 P/DAY 239 CC INITL OBS CARE LV 3 P/DAY 362 CC SUBS OBS CARE LV 1 P/DAY 88 CC SUBS OBS CARE LV 2 P/DAY 145 CC SUBS OBS CARE LV 3 P/DAY 236 CC SNF D/C DAY MGMT 30 OR < 240 CC SNF D/C DAY MGMT >30 318 CC PERC REPLAC J TUBE W/O FL 1948 CC INITIAL NF CARE LEVEL 1 204 CC INITIAL NF CARE LEVEL 2 290 CC INITIAL NF CARE LEVEL 3 368 CC SUBSQENT NF CARE LEVEL 197 CC SUBSQENT NF CARE LEVEL 2 151 CC SUBSQENT NF CARE LEVEL 3 198 CC SUBSQENT NF CARE LEVEL 4 295 CC OBS OR I/P -

Monitoring and Mathematical Modeling of in Vitro Human Megakaryocyte Expansion and Maturation Dynamics
YOUNES LEYSI-DERILOU MONITORING AND MATHEMATICAL MODELING OF IN VITRO HUMAN MEGAKARYOCYTE EXPANSION AND MATURATION DYNAMICS Thèse présentée à la Faculté des études supérieures de l’Université Laval dans le cadre du programme de doctorat en génie chimique pour l’obtention du grade de Philosophiae doctor (Ph.D.) DEPARTMENT DE GÉNIE CHIMIQUE FACULTÉ DE SCIENCES ET GÉNIE UNIVERSITÉ LAVAL QUÉBEC 2011 © Younes Leysi-Derilou, 2011 ii Résumé La mégakaryopoïèse est un processus complexe, qui prend naissance à partir des cellules souches hématopoïétiques (HSC). Ces dernières se différencient par étapes successives en mégakaryocytes (MKs) qui, suite à leur maturation, libèrent les plaquettes. Afin de modéliser le sort des HSCs lors de la mégakaryopoïèse en culture, un nouveau modèle mathématique a été développé, basé sur un programme de différenciation tridimensionnelle (3-D) où chaque sous-population est représentée par un compartiment. Dans le but d’évaluer la prolifération, la différenciation des MKs immatures puis matures, la cinétique de mort cellulaire ainsi que le nombre de plaquettes produites, à partir des cellules de sang de cordon (CB) ombilical enrichies en CD34+, un ensemble d'équations différentielles a été déployé. Les cellules CD34+ ont été placées en culture dans un milieu optimisé pour la différenciation mégakaryocytaire. Les paramètres cinétiques ont été estimés pour deux températures d'incubation (37°C versus 39°C). Les résultats des régressions ont été validés par l'évaluation de l'estimabilité des paramètres, en utilisant des analyses de sensibilité locale et globale, puis la détermination d'un intervalle de confiance. Ceux-ci ont été comparés par le biais de tests statistiques et d’analyses en composante principale (ACP).