The Cytokine Network in Asthma and Chronic Obstructive Pulmonary Disease
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacologic Considerations in the Disposition of Antibodies and Antibody-Drug Conjugates in Preclinical Models and in Patients
antibodies Review Pharmacologic Considerations in the Disposition of Antibodies and Antibody-Drug Conjugates in Preclinical Models and in Patients Andrew T. Lucas 1,2,3,*, Ryan Robinson 3, Allison N. Schorzman 2, Joseph A. Piscitelli 1, Juan F. Razo 1 and William C. Zamboni 1,2,3 1 University of North Carolina (UNC), Eshelman School of Pharmacy, Chapel Hill, NC 27599, USA; [email protected] (J.A.P.); [email protected] (J.F.R.); [email protected] (W.C.Z.) 2 Division of Pharmacotherapy and Experimental Therapeutics, UNC Eshelman School of Pharmacy, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] 3 Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-919-966-5242; Fax: +1-919-966-5863 Received: 30 November 2018; Accepted: 22 December 2018; Published: 1 January 2019 Abstract: The rapid advancement in the development of therapeutic proteins, including monoclonal antibodies (mAbs) and antibody-drug conjugates (ADCs), has created a novel mechanism to selectively deliver highly potent cytotoxic agents in the treatment of cancer. These agents provide numerous benefits compared to traditional small molecule drugs, though their clinical use still requires optimization. The pharmacology of mAbs/ADCs is complex and because ADCs are comprised of multiple components, individual agent characteristics and patient variables can affect their disposition. To further improve the clinical use and rational development of these agents, it is imperative to comprehend the complex mechanisms employed by antibody-based agents in traversing numerous biological barriers and how agent/patient factors affect tumor delivery, toxicities, efficacy, and ultimately, biodistribution. -

Cytokine Nomenclature
RayBiotech, Inc. The protein array pioneer company Cytokine Nomenclature Cytokine Name Official Full Name Genbank Related Names Symbol 4-1BB TNFRSF Tumor necrosis factor NP_001552 CD137, ILA, 4-1BB ligand receptor 9 receptor superfamily .2. member 9 6Ckine CCL21 6-Cysteine Chemokine NM_002989 Small-inducible cytokine A21, Beta chemokine exodus-2, Secondary lymphoid-tissue chemokine, SLC, SCYA21 ACE ACE Angiotensin-converting NP_000780 CD143, DCP, DCP1 enzyme .1. NP_690043 .1. ACE-2 ACE2 Angiotensin-converting NP_068576 ACE-related carboxypeptidase, enzyme 2 .1 Angiotensin-converting enzyme homolog ACTH ACTH Adrenocorticotropic NP_000930 POMC, Pro-opiomelanocortin, hormone .1. Corticotropin-lipotropin, NPP, NP_001030 Melanotropin gamma, Gamma- 333.1 MSH, Potential peptide, Corticotropin, Melanotropin alpha, Alpha-MSH, Corticotropin-like intermediary peptide, CLIP, Lipotropin beta, Beta-LPH, Lipotropin gamma, Gamma-LPH, Melanotropin beta, Beta-MSH, Beta-endorphin, Met-enkephalin ACTHR ACTHR Adrenocorticotropic NP_000520 Melanocortin receptor 2, MC2-R hormone receptor .1 Activin A INHBA Activin A NM_002192 Activin beta-A chain, Erythroid differentiation protein, EDF, INHBA Activin B INHBB Activin B NM_002193 Inhibin beta B chain, Activin beta-B chain Activin C INHBC Activin C NM005538 Inhibin, beta C Activin RIA ACVR1 Activin receptor type-1 NM_001105 Activin receptor type I, ACTR-I, Serine/threonine-protein kinase receptor R1, SKR1, Activin receptor-like kinase 2, ALK-2, TGF-B superfamily receptor type I, TSR-I, ACVRLK2 Activin RIB ACVR1B -

Genentech Tocilizumab Letter of Authority June 24 2021
June 24, 2021 Hoffmann-La Roche, Ltd. C/O Genentech, Inc. Attention: Dhushy Thambipillai Regulatory Project Management 1 DNA Way, Bldg 45-1 South San Francisco, CA 94080 RE: Emergency Use Authorization 099 Dear Ms. Thambipillai: This letter is in response to Genentech, Inc.’s (Genentech) request that the Food and Drug Administration (FDA) issue an Emergency Use Authorization (EUA) for the emergency use of Actemra1 (tocilizumab) for the treatment of coronavirus disease 2019 (COVID-19) in certain hospitalized patients, as described in the Scope of Authorization (Section II) of this letter, pursuant to Section 564 of the Federal Food, Drug, and Cosmetic Act (the Act) (21 U.S.C. §360bbb-3). On February 4, 2020, pursuant to Section 564(b)(1)(C) of the Act, the Secretary of the Department of Health and Human Services (HHS) determined that there is a public health emergency that has a significant potential to affect national security or the health and security of United States citizens living abroad, and that involves the virus that causes coronavirus disease 2019 (COVID-19).2 On the basis of such determination, the Secretary of HHS on March 27, 2020, declared that circumstances exist justifying the authorization of emergency use of drugs and biological products during the COVID-19 pandemic, pursuant to Section 564 of the Act (21 3 U.S.C. 360bbb-3), subject to terms of any authorization issued under that section. Actemra is a recombinant humanized monoclonal antibody that selectively binds to both soluble and membrane-bound human IL-6 receptors (sIL-6R and mIL-6R) and subsequently inhibits IL- 6-mediated signaling through these receptors. -

Kate Fitzgerald
In This Issue: 2020 Young Investigator Awardees pg. 3-9 In Memorium page pg. 14-15 New Member Mini-Bios pg. 19-21 Trials of Interferon Lambda pg. 31 Cytokines 2021 Hybrid Meetin pg. 24-27 Signals THE INTERNATIONAL CYTOKINE & INTERFERON SOCIETY + NEWSLETTER APRIL 2021 I VOLUME 9 I NO. 1 A NOTE FROM THE ICIS PRESIDENT Kate Fitzgerald Dear Colleagues, Greetings from the International Cytokine and Interferon Society! I hope you and your family are staying safe during these still challenging times. Thankfully 2020 is behind us now. We have lived through the COVID-19 pandemic, an event that will continue to impact our lives for some time and likely alter how we live in the future. Despite the obvious difficulties of this past year, I can’t help but marvel at the scientific advances that have been made. With everything from COVID-19 testing, to treatments and especially to the rapid pace of vaccine development, we are so better off today than even a few months back. The approval of remarkably effective COVID-19 vaccines now rolling out in the US, Israel, UK, Europe and across the globe, brings light at the end of the tunnel. The work of many of you has helped shape our understanding of the host response to Sars-CoV2 and the ability of this virus to limit antiviral immunity while simultaneously driving a cytokine driven hyperinflammatory response leading to deadly consequences for patients. The knowledge gained from all of your efforts has been put to good use to stem the threat of this deadly virus. -

Interleukins in Therapeutics
67 ISSN: 2347 - 7881 Review Article Interleukins in Therapeutics Anjan Khadka Department of Pharmacology, AFMC, Pune, India [email protected] ABSTRACT Interleukins are a subset of a larger group of cellular messenger molecules called cytokines, which are modulators of cellular behaviour. On the basis of their respective cytokine profiles, responses to chemokines, and interactions with other cells, these T-cell subsets can promote different types of inflammatory responses. During the development of allergic disease, effector TH2 cells produce IL-4, IL- 5, IL-9, and IL-32. IL-25, IL- 31, and IL-33 contributes to TH2 responses and inflammation. These cytokines have roles in production of allergen-specific IgE, eosinophilia, and mucus. ILs have role in therapeutics as well as diagnosis and prognosis as biomarker in various conditions. Therapeutic targeting of the IL considered to be rational treatment strategy and promising biologic therapy. Keywords: Interleukins, cytokines, Interleukin Inhibitors, Advances INTRODUCTION meaning ‘hormones’. It was Stanley Cohen in Interleukins are group of cytokines that were 1974 who for the first time introduced the term first seen to be expressed by leucocytes and ‘‘cytokine’’. It includes lymphokines, they interact between cells of the immune monokines, interleukins, and colony stimulating systems. It is termed by Dr. Vern Paetkau factors (CSFs), interferons (IFNs), tumor (University of Victoria) in1979.Interleukins (IL) necrosis factor (TNF) and chemokines. The are able to promote cell growth, differentiation, majority of interleukins are synthesized by and functional activation. The question of how helper CD4 T lymphocytes as well as through diverse cell types communicate with each monocytes, macrophages, and endothelial cells. -

Review Anti-Cytokine Biologic Treatment Beyond Anti-TNF in Behçet's Disease
Review Anti-cytokine biologic treatment beyond anti-TNF in Behçet’s disease A. Arida, P.P. Sfikakis First Department of Propedeutic Internal ABSTRACT and thrombotic complications (1-3). Medicine Laikon Hospital, Athens, Unmet therapeutic needs in Behçet’s Treatment varies according to type and University Medical School, Greece. disease have drawn recent attention to severity of disease manifestations. Cor- Aikaterini Arida, MD biological agents targeting cytokines ticosteroids, interferon-alpha and con- Petros P. Sfikakis, MD other than TNF. The anti-IL-17 anti- ventional immunosuppressive drugs, Please address correspondence to: body secukinumab and the anti-IL-2 such as azathioprine, cyclosporine-A, Petros P. Sfikakis, MD, receptor antibody daclizumab were not cyclophosphamide and methotrexate, First Department of Propedeutic superior to placebo for ocular Behçet’s and Internal Medicine, are used either alone or in combination Laikon Hospital, in randomised controlled trials, com- for vital organ involvement. During the Athens University Medical School, prising 118 and 17 patients, respec- last decade there has been increased use Ag Thoma, 17, tively. The anti-IL-1 agents anakinra of anti-TNF monoclonal antibodies in GR-11527 Athens, Greece. and canakinumab and the anti-IL-6 patients with BD who were refractory E-mail: [email protected] agent tocilizumab were given to iso- to conventional treatment or developed Received on June 7, 2014; accepted in lated refractory disease patients, who life-threatening complications (4, 5). revised form on September 17, 2014. were either anti-TNF naïve (n=9) or Anti-TNF treatment has been shown to Clin Exp Rheumatol 2014; 32 (Suppl. 84): experienced (n=18). -

Tocilizumab in Hospitalised Adults with Covid-19
This document has been approved for use at [ ] USE OF TOCILIZUMAB IN HOSPITALISED ADULTS WITH COVID-19 INFORMATION FOR PATIENTS, FAMILIES AND CARERS This information leaflet contains important information about the medicine called tocilizumab when used in the treatment of COVID-19. WHAT IS THE POTENTIAL BENEFIT OF It is important you provide your formal consent TOCILIZUMAB FOR COVID-19? before receiving tocilizumab. You can always change your mind about treatment with Tocilizumab belongs to a group of medicines called tocilizumab and withdraw consent at any time. monoclonal antibodies. Monoclonal antibodies are proteins, which specifically recognise and bind to unique proteins in the body to modify the way the WHAT SHOULD THE DOCTOR KNOW immune system works. Tocilizumab has effects on BEFORE TOCILIZUMAB IS USED IN the immune system that may be useful in helping COVID-19? to reduce the effects of severe COVID-19. The doctor should know about: Tocilizumab has been approved in Australia to treat any other conditions including HIV or AIDs, some immune conditions such as arthritis, cytokine tuberculosis, diverticulitis, stomach ulcers, release syndrome and giant cell arteritis. The brand diabetes, cancer, heart problems, raised name is Actemra®. blood pressure or any nerve disease such as Recent clinical trials studying the effectiveness of neuropathy tocilizumab in COVID-19 have been analysed by previous allergic reactions to any medicine Australia’s National COVID-19 Clinical Evidence all medicines including over-the-counter and Taskforce. The Taskforce makes recommendations complementary medicines e.g. vitamins, about when tocilizumab is most likely to be minerals, herbal or naturopathic medicines effective in the treatment of COVID-19. -

Tocilizumab in the Treatment of Severe and Refractory Parenchymal Neuro
TAB0010.1177/1759720X20971908Therapeutic Advances in Musculoskeletal DiseaseJ Liu, D Yan 971908research-article20202020 Therapeutic Advances in Musculoskeletal Disease Case Series Ther Adv Musculoskel Dis Tocilizumab in the treatment of severe and 2020, Vol. 12: 1–8 DOI:https://doi.org/10.1177/1759720X20971908 10.1177/ refractory parenchymal neuro-Behçet’s 1759720X20971908https://doi.org/10.1177/1759720X20971908 © The Author(s), 2020. Article reuse guidelines: syndrome: case series and literature review sagepub.com/journals- permissions Jinjing Liu* , Dong Yan*, Zhimian Wang, Yunjiao Yang, Shangzhu Zhang, Di Wu, Lingyi Peng, Zhichun Liu and Wenjie Zheng Abstract Correspondence to: Objectives: This study aimed to investigate the efficacy and safety of tocilizumab (TCZ) in Wenjie Zheng severe and refractory parenchymal neuro-Behçet’s syndrome (p-NBS). Department of Rheumatology and Clinical Methods: We retrospectively analyzed five patients with p-NBS treated with TCZ in our center Immunology, Peking Union between 2013 and 2020, and six cases from literature research with the index terms “neuro- Medical College Hospital, Chinese Academy of Behçet’s syndrome” and “tocilizumab” on PubMed NCBI. Medical Sciences & Peking Union Medical Results: A total of 11 patients with p-NBS were enrolled (5 males, 6 females), with a mean College, Key Laboratory of age of 34.5 ± 8.0 years at the onset. All the patients had parenchymal neurological lesions, Rheumatology and Clinical Rheumatology, Ministry six patients (54.5%) suffered from multiple lesions, and nine patients (81.8%) were disabled. of Education, National Clinical Research Center Before TCZ administration, all the patients had failed conventional therapy, eight patients for Dermatologic and (72.7%) received two or more immunosuppressants, and five patients showed insufficient Immunologic Diseases, No. -
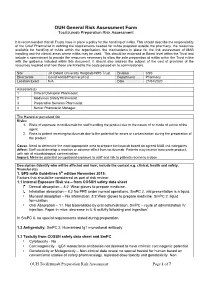
Tocilizumab Preparation Risk Assessment
OUH General Risk Assessment Form Tocilizumab Preparation Risk Assessment It is recommended that all Trusts have in place a policy for the handling of mAbs. This should describe the responsibility of the Chief Pharmacist in defining the requirements needed for mAbs prepared outside the pharmacy, the resources available for handling of mAbs within the organisation, the mechanisms in place for the risk assessment of MAB handling and the clinical areas where mAbs may be used. This should be endorsed at Board level within the Trust and include a commitment to provide the resources necessary to allow the safe preparation of mAbs within the Trust in line with the guidance included within this document. It should also address the subject of the cost of provision of the resources required and how these are linked to the costs passed on to commissioners. Site JR Oxford University Hosptials NHS Trust Division CSS Directorate Covid wards/Pharmacy/ICU Department Pharmacy Location Exact N/A Date 21/04/2020 Assessors(s) 1 Clinical Divisional Pharmacist 2 Medicines Safety Pharmacist 3 Preparative Services Pharmacist 4 Senior Pharmacist Manager The Hazard or perceived risk Risks: 1. Risks of exposure to tocilizumab for staff handling the product due to the nature of or mode of action of the agent 2. Risks to patient receiving tocilizumab due to the potential for errors or contamination during the preparation of the product Cause: Need to determine the most appropriate area to prepare tocilizumab based on agreed MAB risk categories Affect: Staff could develop a reaction or adverse effect from tocilizumab. Patients may receive inaccurate product, with risk of microbiological contamination Impact: Minimise potential occupational exposure to staff and risk to patients receiving a dose Description (Identify who will be affected and how; include the context e.g. -

Successful Usage of Combination Biologic Therapy with Etanercept
Case Report Nov Tech Arthritis Bone Res Volume 2 Issue 4 - Febeuary 2018 Copyright © All rights are reserved by Yoon Kam Hon DOI: 10.19080/NTAB.2017.02.555592 Successful Usage of Combination Biologic Therapy with Etanercept and Actemra for the Treatment of TNF Inhibitor Failure Patients with Rheumatoid Arthritis: A Report of 2 Cases Yoon Kam Hon Department of Arthritis and Rheumatism Specialist Medical Centre, Singapore Submission: January 15, 2018; Published: February 02, 2018 *Corresponding author: Yoon Kam Hon, Consultant Physician And Rheumatologist, El Shaddai Arthritis and Rheumatism Specialist Medical Centre, Block 102 #01-258 Towner Road, Singapore 322102, Tel: +6581258239; Email: Abstract In the treatment of patients with rheumatoid arthritis with anti-tumour necrosis factor therapy, it is not uncommon for some patients to be unresponsive or relapse with treatment. We report the successful usage of combination biologic therapy with etanercept and tocilizumab in two factor and anti-interleukin 6 cytokine therapy in the treatment of rheumatoid arthritis. patients with moderately severe rheumatoid arthritis who failed etanercept therapy. This is the first report of combination anti-tumour necrosis Keywords: Rheumatoid arthritis; Combination biologic therapy; Etanercept; Tocilizumab Introduction therapy inadequate response (IR) RA patients in the RADIATE Rheumatoid arthritis (RA) is a complex chronic autoimmune trial. 50% of patients achieved ACR20 response at week 24, arthritis where many cytokines and chemokines including but only 20% achieved ACR50 response [5]. In the SUMMACTA Tumour Necrosis Factor (TNF), and Interleukin-6 (IL-6) play trial, it was shown that the intravenous (IV) form given at 8mg/ important roles in the pathophysiology of RA. -

Pulmonary Delivery of Biological Drugs
pharmaceutics Review Pulmonary Delivery of Biological Drugs Wanling Liang 1,*, Harry W. Pan 1 , Driton Vllasaliu 2 and Jenny K. W. Lam 1 1 Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, 21 Sassoon Road, Pokfulam, Hong Kong, China; [email protected] (H.W.P.); [email protected] (J.K.W.L.) 2 School of Cancer and Pharmaceutical Sciences, King’s College London, 150 Stamford Street, London SE1 9NH, UK; [email protected] * Correspondence: [email protected]; Tel.: +852-3917-9024 Received: 15 September 2020; Accepted: 20 October 2020; Published: 26 October 2020 Abstract: In the last decade, biological drugs have rapidly proliferated and have now become an important therapeutic modality. This is because of their high potency, high specificity and desirable safety profile. The majority of biological drugs are peptide- and protein-based therapeutics with poor oral bioavailability. They are normally administered by parenteral injection (with a very few exceptions). Pulmonary delivery is an attractive non-invasive alternative route of administration for local and systemic delivery of biologics with immense potential to treat various diseases, including diabetes, cystic fibrosis, respiratory viral infection and asthma, etc. The massive surface area and extensive vascularisation in the lungs enable rapid absorption and fast onset of action. Despite the benefits of pulmonary delivery, development of inhalable biological drug is a challenging task. There are various anatomical, physiological and immunological barriers that affect the therapeutic efficacy of inhaled formulations. This review assesses the characteristics of biological drugs and the barriers to pulmonary drug delivery. -

Modifications to the Harmonized Tariff Schedule of the United States To
U.S. International Trade Commission COMMISSIONERS Shara L. Aranoff, Chairman Daniel R. Pearson, Vice Chairman Deanna Tanner Okun Charlotte R. Lane Irving A. Williamson Dean A. Pinkert Address all communications to Secretary to the Commission United States International Trade Commission Washington, DC 20436 U.S. International Trade Commission Washington, DC 20436 www.usitc.gov Modifications to the Harmonized Tariff Schedule of the United States to Implement the Dominican Republic- Central America-United States Free Trade Agreement With Respect to Costa Rica Publication 4038 December 2008 (This page is intentionally blank) Pursuant to the letter of request from the United States Trade Representative of December 18, 2008, set forth in the Appendix hereto, and pursuant to section 1207(a) of the Omnibus Trade and Competitiveness Act, the Commission is publishing the following modifications to the Harmonized Tariff Schedule of the United States (HTS) to implement the Dominican Republic- Central America-United States Free Trade Agreement, as approved in the Dominican Republic-Central America- United States Free Trade Agreement Implementation Act, with respect to Costa Rica. (This page is intentionally blank) Annex I Effective with respect to goods that are entered, or withdrawn from warehouse for consumption, on or after January 1, 2009, the Harmonized Tariff Schedule of the United States (HTS) is modified as provided herein, with bracketed matter included to assist in the understanding of proclaimed modifications. The following supersedes matter now in the HTS. (1). General note 4 is modified as follows: (a). by deleting from subdivision (a) the following country from the enumeration of independent beneficiary developing countries: Costa Rica (b).