Successful Usage of Combination Biologic Therapy with Etanercept
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacologic Considerations in the Disposition of Antibodies and Antibody-Drug Conjugates in Preclinical Models and in Patients
antibodies Review Pharmacologic Considerations in the Disposition of Antibodies and Antibody-Drug Conjugates in Preclinical Models and in Patients Andrew T. Lucas 1,2,3,*, Ryan Robinson 3, Allison N. Schorzman 2, Joseph A. Piscitelli 1, Juan F. Razo 1 and William C. Zamboni 1,2,3 1 University of North Carolina (UNC), Eshelman School of Pharmacy, Chapel Hill, NC 27599, USA; [email protected] (J.A.P.); [email protected] (J.F.R.); [email protected] (W.C.Z.) 2 Division of Pharmacotherapy and Experimental Therapeutics, UNC Eshelman School of Pharmacy, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] 3 Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-919-966-5242; Fax: +1-919-966-5863 Received: 30 November 2018; Accepted: 22 December 2018; Published: 1 January 2019 Abstract: The rapid advancement in the development of therapeutic proteins, including monoclonal antibodies (mAbs) and antibody-drug conjugates (ADCs), has created a novel mechanism to selectively deliver highly potent cytotoxic agents in the treatment of cancer. These agents provide numerous benefits compared to traditional small molecule drugs, though their clinical use still requires optimization. The pharmacology of mAbs/ADCs is complex and because ADCs are comprised of multiple components, individual agent characteristics and patient variables can affect their disposition. To further improve the clinical use and rational development of these agents, it is imperative to comprehend the complex mechanisms employed by antibody-based agents in traversing numerous biological barriers and how agent/patient factors affect tumor delivery, toxicities, efficacy, and ultimately, biodistribution. -

Genentech Tocilizumab Letter of Authority June 24 2021
June 24, 2021 Hoffmann-La Roche, Ltd. C/O Genentech, Inc. Attention: Dhushy Thambipillai Regulatory Project Management 1 DNA Way, Bldg 45-1 South San Francisco, CA 94080 RE: Emergency Use Authorization 099 Dear Ms. Thambipillai: This letter is in response to Genentech, Inc.’s (Genentech) request that the Food and Drug Administration (FDA) issue an Emergency Use Authorization (EUA) for the emergency use of Actemra1 (tocilizumab) for the treatment of coronavirus disease 2019 (COVID-19) in certain hospitalized patients, as described in the Scope of Authorization (Section II) of this letter, pursuant to Section 564 of the Federal Food, Drug, and Cosmetic Act (the Act) (21 U.S.C. §360bbb-3). On February 4, 2020, pursuant to Section 564(b)(1)(C) of the Act, the Secretary of the Department of Health and Human Services (HHS) determined that there is a public health emergency that has a significant potential to affect national security or the health and security of United States citizens living abroad, and that involves the virus that causes coronavirus disease 2019 (COVID-19).2 On the basis of such determination, the Secretary of HHS on March 27, 2020, declared that circumstances exist justifying the authorization of emergency use of drugs and biological products during the COVID-19 pandemic, pursuant to Section 564 of the Act (21 3 U.S.C. 360bbb-3), subject to terms of any authorization issued under that section. Actemra is a recombinant humanized monoclonal antibody that selectively binds to both soluble and membrane-bound human IL-6 receptors (sIL-6R and mIL-6R) and subsequently inhibits IL- 6-mediated signaling through these receptors. -

Review Anti-Cytokine Biologic Treatment Beyond Anti-TNF in Behçet's Disease
Review Anti-cytokine biologic treatment beyond anti-TNF in Behçet’s disease A. Arida, P.P. Sfikakis First Department of Propedeutic Internal ABSTRACT and thrombotic complications (1-3). Medicine Laikon Hospital, Athens, Unmet therapeutic needs in Behçet’s Treatment varies according to type and University Medical School, Greece. disease have drawn recent attention to severity of disease manifestations. Cor- Aikaterini Arida, MD biological agents targeting cytokines ticosteroids, interferon-alpha and con- Petros P. Sfikakis, MD other than TNF. The anti-IL-17 anti- ventional immunosuppressive drugs, Please address correspondence to: body secukinumab and the anti-IL-2 such as azathioprine, cyclosporine-A, Petros P. Sfikakis, MD, receptor antibody daclizumab were not cyclophosphamide and methotrexate, First Department of Propedeutic superior to placebo for ocular Behçet’s and Internal Medicine, are used either alone or in combination Laikon Hospital, in randomised controlled trials, com- for vital organ involvement. During the Athens University Medical School, prising 118 and 17 patients, respec- last decade there has been increased use Ag Thoma, 17, tively. The anti-IL-1 agents anakinra of anti-TNF monoclonal antibodies in GR-11527 Athens, Greece. and canakinumab and the anti-IL-6 patients with BD who were refractory E-mail: [email protected] agent tocilizumab were given to iso- to conventional treatment or developed Received on June 7, 2014; accepted in lated refractory disease patients, who life-threatening complications (4, 5). revised form on September 17, 2014. were either anti-TNF naïve (n=9) or Anti-TNF treatment has been shown to Clin Exp Rheumatol 2014; 32 (Suppl. 84): experienced (n=18). -

Tocilizumab in Hospitalised Adults with Covid-19
This document has been approved for use at [ ] USE OF TOCILIZUMAB IN HOSPITALISED ADULTS WITH COVID-19 INFORMATION FOR PATIENTS, FAMILIES AND CARERS This information leaflet contains important information about the medicine called tocilizumab when used in the treatment of COVID-19. WHAT IS THE POTENTIAL BENEFIT OF It is important you provide your formal consent TOCILIZUMAB FOR COVID-19? before receiving tocilizumab. You can always change your mind about treatment with Tocilizumab belongs to a group of medicines called tocilizumab and withdraw consent at any time. monoclonal antibodies. Monoclonal antibodies are proteins, which specifically recognise and bind to unique proteins in the body to modify the way the WHAT SHOULD THE DOCTOR KNOW immune system works. Tocilizumab has effects on BEFORE TOCILIZUMAB IS USED IN the immune system that may be useful in helping COVID-19? to reduce the effects of severe COVID-19. The doctor should know about: Tocilizumab has been approved in Australia to treat any other conditions including HIV or AIDs, some immune conditions such as arthritis, cytokine tuberculosis, diverticulitis, stomach ulcers, release syndrome and giant cell arteritis. The brand diabetes, cancer, heart problems, raised name is Actemra®. blood pressure or any nerve disease such as Recent clinical trials studying the effectiveness of neuropathy tocilizumab in COVID-19 have been analysed by previous allergic reactions to any medicine Australia’s National COVID-19 Clinical Evidence all medicines including over-the-counter and Taskforce. The Taskforce makes recommendations complementary medicines e.g. vitamins, about when tocilizumab is most likely to be minerals, herbal or naturopathic medicines effective in the treatment of COVID-19. -

Tocilizumab in the Treatment of Severe and Refractory Parenchymal Neuro
TAB0010.1177/1759720X20971908Therapeutic Advances in Musculoskeletal DiseaseJ Liu, D Yan 971908research-article20202020 Therapeutic Advances in Musculoskeletal Disease Case Series Ther Adv Musculoskel Dis Tocilizumab in the treatment of severe and 2020, Vol. 12: 1–8 DOI:https://doi.org/10.1177/1759720X20971908 10.1177/ refractory parenchymal neuro-Behçet’s 1759720X20971908https://doi.org/10.1177/1759720X20971908 © The Author(s), 2020. Article reuse guidelines: syndrome: case series and literature review sagepub.com/journals- permissions Jinjing Liu* , Dong Yan*, Zhimian Wang, Yunjiao Yang, Shangzhu Zhang, Di Wu, Lingyi Peng, Zhichun Liu and Wenjie Zheng Abstract Correspondence to: Objectives: This study aimed to investigate the efficacy and safety of tocilizumab (TCZ) in Wenjie Zheng severe and refractory parenchymal neuro-Behçet’s syndrome (p-NBS). Department of Rheumatology and Clinical Methods: We retrospectively analyzed five patients with p-NBS treated with TCZ in our center Immunology, Peking Union between 2013 and 2020, and six cases from literature research with the index terms “neuro- Medical College Hospital, Chinese Academy of Behçet’s syndrome” and “tocilizumab” on PubMed NCBI. Medical Sciences & Peking Union Medical Results: A total of 11 patients with p-NBS were enrolled (5 males, 6 females), with a mean College, Key Laboratory of age of 34.5 ± 8.0 years at the onset. All the patients had parenchymal neurological lesions, Rheumatology and Clinical Rheumatology, Ministry six patients (54.5%) suffered from multiple lesions, and nine patients (81.8%) were disabled. of Education, National Clinical Research Center Before TCZ administration, all the patients had failed conventional therapy, eight patients for Dermatologic and (72.7%) received two or more immunosuppressants, and five patients showed insufficient Immunologic Diseases, No. -
Tocilizumab Preparation Risk Assessment
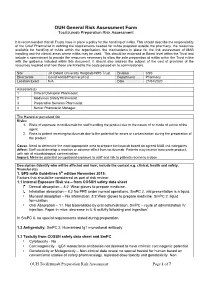
OUH General Risk Assessment Form Tocilizumab Preparation Risk Assessment It is recommended that all Trusts have in place a policy for the handling of mAbs. This should describe the responsibility of the Chief Pharmacist in defining the requirements needed for mAbs prepared outside the pharmacy, the resources available for handling of mAbs within the organisation, the mechanisms in place for the risk assessment of MAB handling and the clinical areas where mAbs may be used. This should be endorsed at Board level within the Trust and include a commitment to provide the resources necessary to allow the safe preparation of mAbs within the Trust in line with the guidance included within this document. It should also address the subject of the cost of provision of the resources required and how these are linked to the costs passed on to commissioners. Site JR Oxford University Hosptials NHS Trust Division CSS Directorate Covid wards/Pharmacy/ICU Department Pharmacy Location Exact N/A Date 21/04/2020 Assessors(s) 1 Clinical Divisional Pharmacist 2 Medicines Safety Pharmacist 3 Preparative Services Pharmacist 4 Senior Pharmacist Manager The Hazard or perceived risk Risks: 1. Risks of exposure to tocilizumab for staff handling the product due to the nature of or mode of action of the agent 2. Risks to patient receiving tocilizumab due to the potential for errors or contamination during the preparation of the product Cause: Need to determine the most appropriate area to prepare tocilizumab based on agreed MAB risk categories Affect: Staff could develop a reaction or adverse effect from tocilizumab. Patients may receive inaccurate product, with risk of microbiological contamination Impact: Minimise potential occupational exposure to staff and risk to patients receiving a dose Description (Identify who will be affected and how; include the context e.g. -

Downloaded Here
Antibodies to Watch in a Pandemic Dr. Janice M. Reichert, Executive Director, The Antibody Society August 27, 2020 (updated slides) Agenda • US or EU approvals in 2020 • Granted as of late July 2020 • Anticipated by the end of 2020 • Overview of antibody-based COVID-19 interventions in development • Repurposed antibody-based therapeutics that treat symptoms • Newly developed anti-SARS-CoV-2 antibodies • Q&A 2 Number of first approvals for mAbs 10 12 14 16 18 20 Annual first approvals in either the US or EU or US the either in approvals first Annual 0 2 4 6 8 *Estimate based on the number actually approved and those in review as of July 15, with assumption of approval on the first c first the on of approval assumption 15, with as July of review in those and approved actually number the on based *Estimate Tables of approved mAbs and antibodies in review available at at mAbs ofand available in antibodies approved review Tables 1997 98 99 2000 01 02 03 Year of first US or EU approval or EU US of first Year 04 05 06 https://www.antibodysociety.org/resources/approved 07 08 09 10 11 12 13 14 15 Non-cancer Cancer 16 - antibodies/ 17 ycl 18 e. 19 2020* First approvals US or EU in 2020 • Teprotumumab (Tepezza): anti-IGF-1R mAb for thyroid eye disease • FDA approved on January 21 • Eptinezumab (Vyepti): anti-CGRP IgG1 for migraine prevention • FDA approved on February 21 • Isatuximab (Sarclisa): anti-CD38 IgG1 for multiple myeloma • FDA approved on March 2, also approved in the EU on June 2 • Sacituzumab govitecan (Trodelvy): anti-TROP-2 ADC for triple-neg. -

Asthma Agents
APPROVED PA Criteria Initial Approval Date: July 10, 2019 Revised Date: January 20, 2021 CRITERIA FOR PRIOR AUTHORIZATION Asthma Agents BILLING CODE TYPE For drug coverage and provider type information, see the KMAP Reference Codes webpage. MANUAL GUIDELINES Prior authorization will be required for all current and future dose forms available. All medication-specific criteria, including drug-specific indication, age, and dose for each agent is defined in Table 1 below. Benralizumab (Fasenra®) Dupilumab (Dupixent®) Mepolizumab (Nucala®) Omalizumab (Xolair®) Reslizumab (Cinqair®) GENERAL CRITERIA FOR INITIAL PRIOR AUTHORIZATION: (must meet all of the following) • Must be approved for the indication, age, and not exceed dosing limits listed in Table 1. • Must be prescribed by or in consultation with a pulmonologist, allergist, or immunologist.1,2 • For all agents listed, the preferred PDL drug, which treats the PA indication, is required unless the patient meets the non-preferred PDL PA criteria. • Must have experienced ≥ 2 exacerbations within the last 12 months despite meeting all of the following (exacerbation is defined as requiring the use of oral/systemic corticosteroids, urgent care/hospital admission, or intubation: o Patient adherence to two long-term controller medications, including a high-dose inhaled corticosteroid 1,2 (ICS) and a long-acting beta2-agonist (LABA) listed in Table 2. ▪ Combination ICS/LABA and ICS/LABA/LAMA products meet the requirement of two controller medications. o Patient must have had an adequate trial (at least 90 consecutive days) of a leukotriene modifier or a long-acting muscarinic antagonist (LAMA) as a third long-term controller medication listed in Table 2. -

Cimzia (Certolizumab Pegol) AHM
Cimzia (Certolizumab Pegol) AHM Clinical Indications • Cimzia (Certolizumab Pegol) is considered medically necessary for adult members 18 years of age or older with moderately-to-severely active disease when ALL of the following conditions are met o Moderately-to-severely active Crohn's disease as manifested by 1 or more of the following . Diarrhea . Abdominal pain . Bleeding . Weight loss . Perianal disease . Internal fistulae . Intestinal obstruction . Megacolon . Extra-intestinal manifestations: arthritis or spondylitis o Crohn's disease has remained active despite treatment with 1 or more of the following . Corticosteroids . 6-mercaptopurine/azathioprine • Certollizumab pegol (see note) is considered medically necessary for persons with active psoriatic arthritis who meet criteria in Psoriasis and Psoriatic Arthritis: Biological Therapies. • Cimzia, (Certolizumab Pegol), alone or in combination with methotrexate (MTX), is considered medically necessary for the treatment of adult members 18 years of age or older with moderately-to-severely active rheumatoid arthritis (RA). • Cimzia (Certolizumab pegol is considered medically necessary for reducing signs and symptoms of members with active ankylosing spondylitis who have an inadequate response to 2 or more NSAIDs. • Cimzia (Certolizumab Pegol) is considered investigational for all other indications (e.g.,ocular inflammation/uveitis; not an all-inclusive list) because its effectiveness for indications other than the ones listed above has not been established. Notes • There are several brands of targeted immune modulators on the market. There is a lack of reliable evidence that any one brand of targeted immune modulator is superior to other brands for medically necessary indications. Enbrel (etanercept), Humira (adalimumab), Remicade (infliximab), Simponi (golimumab), Simponi Aria (golimumab intravneous), and Stelara (ustekinumab) brands of targeted immune modulators ("least cost brands of targeted immune modulators") are less costly to the plan. -

Antibodies to Watch in 2021 Hélène Kaplona and Janice M
MABS 2021, VOL. 13, NO. 1, e1860476 (34 pages) https://doi.org/10.1080/19420862.2020.1860476 PERSPECTIVE Antibodies to watch in 2021 Hélène Kaplona and Janice M. Reichert b aInstitut De Recherches Internationales Servier, Translational Medicine Department, Suresnes, France; bThe Antibody Society, Inc., Framingham, MA, USA ABSTRACT ARTICLE HISTORY In this 12th annual installment of the Antibodies to Watch article series, we discuss key events in antibody Received 1 December 2020 therapeutics development that occurred in 2020 and forecast events that might occur in 2021. The Accepted 1 December 2020 coronavirus disease 2019 (COVID-19) pandemic posed an array of challenges and opportunities to the KEYWORDS healthcare system in 2020, and it will continue to do so in 2021. Remarkably, by late November 2020, two Antibody therapeutics; anti-SARS-CoV antibody products, bamlanivimab and the casirivimab and imdevimab cocktail, were cancer; COVID-19; Food and authorized for emergency use by the US Food and Drug Administration (FDA) and the repurposed Drug Administration; antibodies levilimab and itolizumab had been registered for emergency use as treatments for COVID-19 European Medicines Agency; in Russia and India, respectively. Despite the pandemic, 10 antibody therapeutics had been granted the immune-mediated disorders; first approval in the US or EU in 2020, as of November, and 2 more (tanezumab and margetuximab) may Sars-CoV-2 be granted approvals in December 2020.* In addition, prolgolimab and olokizumab had been granted first approvals in Russia and cetuximab saratolacan sodium was first approved in Japan. The number of approvals in 2021 may set a record, as marketing applications for 16 investigational antibody therapeutics are already undergoing regulatory review by either the FDA or the European Medicines Agency. -

The Cytokine Network in Asthma and Chronic Obstructive Pulmonary Disease
The cytokine network in asthma and chronic obstructive pulmonary disease Peter J. Barnes J Clin Invest. 2008;118(11):3546-3556. https://doi.org/10.1172/JCI36130. Review Series Asthma and chronic obstructive pulmonary disease (COPD) are very common inflammatory diseases of the airways. They both cause airway narrowing and are increasing in incidence throughout the world, imposing enormous burdens on health care. Cytokines play a key role in orchestrating the chronic inflammation and structural changes of the respiratory tract in both asthma and COPD and have become important targets for the development of new therapeutic strategies in these diseases. Find the latest version: https://jci.me/36130/pdf Review series The cytokine network in asthma and chronic obstructive pulmonary disease Peter J. Barnes National Heart & Lung Institute, Imperial College London, London, United Kingdom. Asthma and chronic obstructive pulmonary disease (COPD) are very common inflammatory diseases of the air- ways. They both cause airway narrowing and are increasing in incidence throughout the world, imposing enormous burdens on health care. Cytokines play a key role in orchestrating the chronic inflammation and structural changes of the respiratory tract in both asthma and COPD and have become important targets for the development of new therapeutic strategies in these diseases. Introduction Inflammation in asthma and COPD The most common inflammatory diseases of the airways are Despite the similarity of some clinical features of asthma and asthma and chronic obstructive pulmonary disease (COPD), COPD, there are marked differences in the pattern of inflamma- and the incidence of both is increasing throughout the world. tion in the respiratory tract, with different inflammatory cells, The prevalence of asthma in developed countries is approxi- mediators, consequences, and responses to therapy (1). -

Biologics in Asthma
Biologics in Asthma: Present andPresenter Future of Flavia Hoyte,Reproduction MD Associate Professorfor of Medicine FellowshipProperty Training Program Director DivisionNot of Allergy and Immunology National Jewish Health and University of Colorado Disclosures Clinical investigator for GSK, TEVA, and Astra‐ Zeneca. Presenter of Reproduction for Property Not Learning objectives 1. Discuss current approaches to the management of moderate to severe asthma in adult patients. Presenter of 2. Describe new and emergingReproduction biologics for for the managementProperty of moderate to severe asthma. Not Asthma: A Highly Prevalent and Often Inadequately Controlled Disease 24+ million people in the US have asthma.1 17.72 million adults have asthma.Presenter1 of Reproduction 8.86 million adults havefor inadequately 39% of adults with Propertycontrolled asthma.2 1.33 million adults active asthma use Not have inadequately long‐term control controlled asthma medications.3 with eosinophilia.4 1. Centers for Disease Control and Prevention (CDC). Most Recent Asthma Data (2014 data). Accessed June 2016. 2. CDC. Uncontrolled asthma among persons with current asthma. Accessed June 2016. 3. CDC. Use of long‐term control medication among persons with active asthma. Accessed June 2016. 4. McGrath KW et al. Am J Respir Crit Care Med. 2012;185:612‐619. Paradigm Shift to a More Personalized Approach to Asthma Therapy Presenter of Reproduction for Property Not Dunn RM and Wechsler ME. Clinical Pharmacology and Therapeutics 2015; 97(1): 55‐65. Immunopathology of Asthma Presenter of Reproduction for Property Not Pelaia G, et al. Mediators Inflamm 2015:879783. doi: 10.1155/2015/879783. Epub 2015 Mar 23. Presenter of Reproduction for Property Not Katial et al.