Care of Your Humeral (Upper Arm) Fracture
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Body Mechanics As the Rotator Cuff Gether in a Cuff-Shape Across the Greater and Lesser Tubercles the on Head of the Humerus
EXPerT CONTENT Body Mechanics by Joseph E. Muscolino | Artwork Giovanni Rimasti | Photography Yanik Chauvin Rotator Cuff Injury www.amtamassage.org/mtj WORKING WITH CLieNTS AFFecTED BY THIS COmmON CONDITION ROTATOR CUFF GROUP as the rotator cuff group because their distal tendons blend and attach to- The four rotator cuff muscles are gether in a cuff-shape across the greater and lesser tubercles on the head of the supraspinatus, infraspinatus, the humerus. Although all four rotator cuff muscles have specific concen- teres minor, and subscapularis (Fig- tric mover actions at the glenohumeral (GH) joint, their primary functional ure 1). These muscles are described importance is to contract isometrically for GH joint stabilization. Because 17 Before practicing any new modality or technique, check with your state’s or province’s massage therapy regulatory authority to ensure that it is within the defined scope of practice for massage therapy. the rotator cuff group has both mover and stabilization roles, it is extremely functionally active and therefore often physically stressed and injured. In fact, after neck and low back conditions, the shoulder is the most com- Supraspinatus monly injured joint of the human body. ROTATOR CUFF PATHOLOGY The three most common types of rotator cuff pathology are tendinitis, tendinosus, and tearing. Excessive physi- cal stress placed on the rotator cuff tendon can cause ir- ritation and inflammation of the tendon, in other words, tendinitis. If the physical stress is chronic, the inflam- matory process often subsides and degeneration of the fascial tendinous tissue occurs; this is referred to as tendinosus. The degeneration of tendinosus results in weakness of the tendon’s structure, and with continued Teres minor physical stress, whether it is overuse microtrauma or a macrotrauma, a rotator cuff tendon tear might occur. -
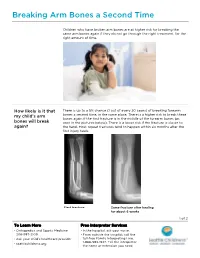
PE2812 Breaking Arm Bones a Second Time
Breaking Arm Bones a Second Time Children who have broken arm bones are at higher risk for breaking the same arm bones again if they do not go through the right treatment, for the right amount of time. How likely is it that There is up to a 5% chance (1 out of every 20 cases) of breaking forearm my child’s arm bones a second time, in the same place. There is a higher risk to break these bones again if the first fracture is in the middle of the forearm bones (as bones will break seen in the pictures below). There is a lower risk if the fracture is closer to again? the hand. Most repeat fractures tend to happen within six months after the first injury heals. First fracture Same fracture after healing for about 6 weeks 1 of 2 To Learn More Free Interpreter Services • Orthopedics and Sports Medicine • In the hospital, ask your nurse. 206-987-2109 • From outside the hospital, call the • Ask your child’s healthcare provider toll-free Family Interpreting Line, 1-866-583-1527. Tell the interpreter • seattlechildrens.org the name or extension you need. Breaking Arm Bones a Second Time How can I help my Wearing a cast for at least six weeks lowers the risk of breaking the same child lower the risk arm bones again. After wearing a cast, we recommend your child wear a brace for 4 weeks in order to protect the injured area and start improving of having a wrist movement. While your child wears a brace, we recommend they do repeated bone not participate in contact sports (e.g., soccer, football or dodge ball). -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

GLOSSARY of MEDICAL and ANATOMICAL TERMS
GLOSSARY of MEDICAL and ANATOMICAL TERMS Abbreviations: • A. Arabic • abb. = abbreviation • c. circa = about • F. French • adj. adjective • G. Greek • Ge. German • cf. compare • L. Latin • dim. = diminutive • OF. Old French • ( ) plural form in brackets A-band abb. of anisotropic band G. anisos = unequal + tropos = turning; meaning having not equal properties in every direction; transverse bands in living skeletal muscle which rotate the plane of polarised light, cf. I-band. Abbé, Ernst. 1840-1905. German physicist; mathematical analysis of optics as a basis for constructing better microscopes; devised oil immersion lens; Abbé condenser. absorption L. absorbere = to suck up. acervulus L. = sand, gritty; brain sand (cf. psammoma body). acetylcholine an ester of choline found in many tissue, synapses & neuromuscular junctions, where it is a neural transmitter. acetylcholinesterase enzyme at motor end-plate responsible for rapid destruction of acetylcholine, a neurotransmitter. acidophilic adj. L. acidus = sour + G. philein = to love; affinity for an acidic dye, such as eosin staining cytoplasmic proteins. acinus (-i) L. = a juicy berry, a grape; applied to small, rounded terminal secretory units of compound exocrine glands that have a small lumen (adj. acinar). acrosome G. akron = extremity + soma = body; head of spermatozoon. actin polymer protein filament found in the intracellular cytoskeleton, particularly in the thin (I-) bands of striated muscle. adenohypophysis G. ade = an acorn + hypophyses = an undergrowth; anterior lobe of hypophysis (cf. pituitary). adenoid G. " + -oeides = in form of; in the form of a gland, glandular; the pharyngeal tonsil. adipocyte L. adeps = fat (of an animal) + G. kytos = a container; cells responsible for storage and metabolism of lipids, found in white fat and brown fat. -

98796-Anatomy of the Orbit
Anatomy of the orbit Prof. Pia C Sundgren MD, PhD Department of Diagnostic Radiology, Clinical Sciences, Lund University, Sweden Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lay-out • brief overview of the basic anatomy of the orbit and its structures • the orbit is a complicated structure due to its embryological composition • high number of entities, and diseases due to its composition of ectoderm, surface ectoderm and mesoderm Recommend you to read for more details Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 3 x 3 Imaging technique 3 layers: - neuroectoderm (retina, iris, optic nerve) - surface ectoderm (lens) • CT and / or MR - mesoderm (vascular structures, sclera, choroid) •IOM plane 3 spaces: - pre-septal •thin slices extraconal - post-septal • axial and coronal projections intraconal • CT: soft tissue and bone windows 3 motor nerves: - occulomotor (III) • MR: T1 pre and post, T2, STIR, fat suppression, DWI (?) - trochlear (IV) - abducens (VI) Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Superior orbital fissure • cranial nerves (CN) III, IV, and VI • lacrimal nerve • frontal nerve • nasociliary nerve • orbital branch of middle meningeal artery • recurrent branch of lacrimal artery • superior orbital vein • superior ophthalmic vein Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. -

Morphology of the Foramen Magnum in Young Eastern European Adults
Folia Morphol. Vol. 71, No. 4, pp. 205–216 Copyright © 2012 Via Medica O R I G I N A L A R T I C L E ISSN 0015–5659 www.fm.viamedica.pl Morphology of the foramen magnum in young Eastern European adults F. Burdan1, 2, J. Szumiło3, J. Walocha4, L. Klepacz5, B. Madej1, W. Dworzański1, R. Klepacz3, A. Dworzańska1, E. Czekajska-Chehab6, A. Drop6 1Department of Human Anatomy, Medical University of Lublin, Lublin, Poland 2St. John’s Cancer Centre, Lublin, Poland 3Department of Clinical Pathomorphology, Medical University of Lublin, Lublin, Poland 4Department of Anatomy, Collegium Medicum, Jagiellonian University, Krakow, Poland 5Department of Psychiatry and Behavioural Sciences, Behavioural Health Centre, New York Medical College, Valhalla NY, USA 6Department of General Radiology and Nuclear Medicine, Medical University of Lublin, Lublin, Poland [Received 21 July 2012; Accepted 7 September 2012] Background: The foramen magnum is an important anatomical opening in the base of the skull through which the posterior cranial fossa communicates with the vertebral canal. It is also related to a number of pathological condi- tions including Chiari malformations, various tumours, and occipital dysplasias. The aim of the study was to evaluate the morphology of the foramen magnum in adult individuals in relation to sex. Material and methods: The morphology of the foramen magnum was evalu- ated using 3D computer tomography images in 313 individuals (142 male, 171 female) aged 20–30 years. Results: The mean values of the foramen length (37.06 ± 3.07 vs. 35.47 ± ± 2.60 mm), breadth (32.98 ± 2.78 vs. 30.95 ± 2.71 mm) and area (877.40 ± ± 131.64 vs. -

Bone Limb Upper
Shoulder Pectoral girdle (shoulder girdle) Scapula Acromioclavicular joint proximal end of Humerus Clavicle Sternoclavicular joint Bone: Upper limb - 1 Scapula Coracoid proc. 3 angles Superior Inferior Lateral 3 borders Lateral angle Medial Lateral Superior 2 surfaces 3 processes Posterior view: Acromion Right Scapula Spine Coracoid Bone: Upper limb - 2 Scapula 2 surfaces: Costal (Anterior), Posterior Posterior view: Costal (Anterior) view: Right Scapula Right Scapula Bone: Upper limb - 3 Scapula Glenoid cavity: Glenohumeral joint Lateral view: Infraglenoid tubercle Right Scapula Supraglenoid tubercle posterior anterior Bone: Upper limb - 4 Scapula Supraglenoid tubercle: long head of biceps Anterior view: brachii Right Scapula Bone: Upper limb - 5 Scapula Infraglenoid tubercle: long head of triceps brachii Anterior view: Right Scapula (with biceps brachii removed) Bone: Upper limb - 6 Posterior surface of Scapula, Right Acromion; Spine; Spinoglenoid notch Suprspinatous fossa, Infraspinatous fossa Bone: Upper limb - 7 Costal (Anterior) surface of Scapula, Right Subscapular fossa: Shallow concave surface for subscapularis Bone: Upper limb - 8 Superior border Coracoid process Suprascapular notch Suprascapular nerve Posterior view: Right Scapula Bone: Upper limb - 9 Acromial Clavicle end Sternal end S-shaped Acromial end: smaller, oval facet Sternal end: larger,quadrangular facet, with manubrium, 1st rib Conoid tubercle Trapezoid line Right Clavicle Bone: Upper limb - 10 Clavicle Conoid tubercle: inferior -

Trapezius Origin: Occipital Bone, Ligamentum Nuchae & Spinous Processes of Thoracic Vertebrae Insertion: Clavicle and Scapul
Origin: occipital bone, ligamentum nuchae & spinous processes of thoracic vertebrae Insertion: clavicle and scapula (acromion Trapezius and scapular spine) Action: elevate, retract, depress, or rotate scapula upward and/or elevate clavicle; extend neck Origin: spinous process of vertebrae C7-T1 Rhomboideus Insertion: vertebral border of scapula Minor Action: adducts & performs downward rotation of scapula Origin: spinous process of superior thoracic vertebrae Rhomboideus Insertion: vertebral border of scapula from Major spine to inferior angle Action: adducts and downward rotation of scapula Origin: transverse precesses of C1-C4 vertebrae Levator Scapulae Insertion: vertebral border of scapula near superior angle Action: elevates scapula Origin: anterior and superior margins of ribs 1-8 or 1-9 Insertion: anterior surface of vertebral Serratus Anterior border of scapula Action: protracts shoulder: rotates scapula so glenoid cavity moves upward rotation Origin: anterior surfaces and superior margins of ribs 3-5 Insertion: coracoid process of scapula Pectoralis Minor Action: depresses & protracts shoulder, rotates scapula (glenoid cavity rotates downward), elevates ribs Origin: supraspinous fossa of scapula Supraspinatus Insertion: greater tuberacle of humerus Action: abduction at the shoulder Origin: infraspinous fossa of scapula Infraspinatus Insertion: greater tubercle of humerus Action: lateral rotation at shoulder Origin: clavicle and scapula (acromion and adjacent scapular spine) Insertion: deltoid tuberosity of humerus Deltoid Action: -

The Skull O Neurocranium, Form and Function O Dermatocranium, Form
Lesson 15 ◊ Lesson Outline: ♦ The Skull o Neurocranium, Form and Function o Dermatocranium, Form and Function o Splanchnocranium, Form and Function • Evolution and Design of Jaws • Fate of the Splanchnocranium ♦ Trends ◊ Objectives: At the end of this lesson, you should be able to: ♦ Describe the structure and function of the neurocranium ♦ Describe the structure and function of the dermatocranium ♦ Describe the origin of the splanchnocranium and discuss the various structures that have evolved from it. ♦ Describe the structure and function of the various structures that have been derived from the splanchnocranium ♦ Discuss various types of jaw suspension and the significance of the differences in each type ◊ References: ♦ Chapter: 9: 162-198 ◊ Reading for Next Lesson: ♦ Chapter: 9: 162-198 The Skull: From an anatomical perspective, the skull is composed of three parts based on the origins of the various components that make up the final product. These are the: Neurocranium (Chondocranium) Dermatocranium Splanchnocranium Each part is distinguished by its ontogenetic and phylogenetic origins although all three work together to produce the skull. The first two are considered part of the Cranial Skeleton. The latter is considered as a separate Visceral Skeleton in our textbook. Many other morphologists include the visceral skeleton as part of the cranial skeleton. This is a complex group of elements that are derived from the ancestral skeleton of the branchial arches and that ultimately gives rise to the jaws and the skeleton of the gill -
Osteoma of Occipital Bone
© 2003 Indian Journal of Surgery www.indianjsurg.comCase Report Effective treatment is crucial for avoiding recurrent Low-grade chondrosarcoma in an extremity can be incidence and depends on excising all tissues with treated with limited surgery. carcinoma. As the tumour is radio-resistant, complete removal is the only treatment of choice. A wide excision REFERENCES for low-grade chondrosarcoma is generally advised. Following open biopsy, local excision or, if required, 1. Bovee JVMG, van der Heul RO, Taminiau AHM, Hogendoorn PCW, reconstruction is advised.5 Chondrosarcoma of the phalanx: A locally aggressive lesion with minimal metastatic potential. Cancer 1999;86:1724-32. 2. Evans HL, Ayala AG, Romsdahl MM, Prognostic factors in chond- In our case, we think that the removal of the tumoral rosarcoma of bone. Cancer 1977;40:818-31. tissue from the normal tissue margin is the treatment 3. Dahlin DC, Beabout JW, Dedifferentiation of low-grade chondro- sarcomas. Cancer 1971;28:461-6. of choice. Our case is a young case that had Grade 1 4. Damron TA, Rock MG, Unni KK, Subcutaneous involvement after chondrosarcoma in his fourth and fifth finger and fifth a metacarpal chondrosarcoma: Case report and review of litera- metatarsal diaphysis. The difference of our case from ture. Clin Orthop 1995;316:189-94. 5. Ogose A, Unni KK, Swee RG, May GK, Rowland CM, Sim FH. the ones reported in literature is that he was young Chondrosarcoma of small bones of the hands and feet. Cancer (18-year-old) and had a lesion involving two different 1997;80:50-9. compartments synchronously as localization. -

Evaluation of Humeral and Glenoid Bone Deformity in Glenohumeral Arthritis 5
Evaluation of Humeral and Glenoid Bone Deformity 1 in Glenohumeral Arthritis Brian F. Grogan and Charles M. Jobin Introduction glenoid bone wear helps the surgeon formulate a successful treatment plan and surgical goals Glenohumeral arthritis is the sequela of a vari- to address the pathoanatomy and improve the ety of pathologic shoulder processes, most durability of shoulder arthroplasty. The evalu- commonly degenerative osteoarthritis, but may ation of humeral and glenoid bone deformity also be secondary to post-traumatic conditions, in glenohumeral arthritis has profound surgical inflammatory arthritis, rotator cuff tear arthrop- implications and is fundamental to successful athy, and postsurgical conditions most com- shoulder arthroplasty. monly post-capsulorrhaphy arthritis. Patients with glenohumeral arthritis commonly demon- strate patterns of bony deformity on the glenoid Glenoid Deformity in Osteoarthritis and humerus that are caused by the etiology of the arthritis. For example, osteoarthritis com- Glenoid deformity and glenohumeral subluxation monly presents with posterior glenoid wear, are commonly seen in the setting of primary osteo- secondary glenoid retroversion, and posterior arthritis of the glenohumeral joint. The glenoid humeral head subluxation, while inflammatory wear tends to occur posteriorly and may be best arthritis routinely causes concentric glenoid viewed on axial radiographs or computed tomog- wear with central glenoid erosion. A thorough raphy (CT) axial images. Glenoid erosion, as first history and physical, as well as laboratory and characterized by Walch, is noted to be either central radiographic workup, are keys to understanding or posterior, with varying degrees of wear and pos- the etiology of arthritis and understanding the terior subluxation of the humerus [1, 2] (Fig. -

Avulsion Fracture of Brachioradialis Muscle Origin: an Exceedingly Rare Entity: a Case Report
10-039_OA1 8/13/16 5:34 PM Page 50 Malaysian Orthopaedic Journal 2016 Vol 10 No 2 Behera G, et al http://dx.doi.org/10.5704/MOJ.1607.010 Avulsion Fracture of Brachioradialis Muscle Origin: An Exceedingly Rare Entity: A Case Report Behera G, DNB, Balaji G, MS Ortho, Menon J, MRCS (Edin.), Sharma D, MCH, Komuravalli VK, DNB Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry, India Date of submission: March 2016 Date of acceptance: June 2016 ABSTRACT lateral supracondylar ridge just proximal to the lateral epicondyle. He had restriction of active terminal elbow Avulsion fracture of the brachioradialis origin at its proximal extension by 10 degrees with near normal active elbow attachment on the lateral supracondylar ridge of the distal flexion, pronation and supination. Active flexion and humerus is exceedingly rare, and only two cases have been extension at wrist were painful along with the painful reported in the literature so far. In this article, we present a terminal elbow extension. There was significant pain at the 38 years old patient who sustained a closed avulsion fracture lateral distal humerus when active elbow flexion against of the lateral supracondylar ridge of left humerus at the resistance was performed in the mid-pronated position of the proximal attachment of brachioradialis following a fall forearm. There was no distal neurovascular deficit. backwards on outstretched hand after being struck by a lorry from behind while riding on a two-wheeler (motorcycle). He Antero-posterior (AP) plain radiograph of the left elbow was managed with above elbow plaster for four weeks showed a fracture of the lateral distal humerus at the followed by elbow and wrist mobilization.