Medical-Surgical Nursing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Assessing the Impact of an Electronic Medical Record on Nurse
CIN: Computers, Informatics, Nursing & Vol. 26, No. 4, 234–241 & Copyright B 2008 Wolters Kluwer Health | Lippincott Williams & Wilkins FEATURE ARTICLE Assessing the Work sampling measured nurse documentation Impact of an time before and after the implementation of an electronic medical record on a medical-surgical Electronic Medical nursing unit. Documentation was separated into subprocesses of admissions, discharges, and Record on Nurse routine/daily documentations. Production rate of documentation time is defined and measured. The results indicate that there is no difference in Documentation Time documentation time between pre-electronic med- ical record and post-electronic medical record for BRIAN HAKES, MBA admissions and routine/daily documentation time. JOHN WHITTINGTON, MD Post-electronic medical record documentation time was longer than that in the pre-electronic medical record for patients discharged to a nursing home. It was demonstrated that the electronic medical record may reduce documentation time after the Healthcare today is facing constant pressure to decrease adoption of computerized physician order entry. waste and reduce cost. Improving efficiency, safety, and quality is the reason for implementing an electronic KEY WORDS medical record (EMR). However, studies have shown EMR Benefit Realization & variable impact.1–7 At OSF HealthCare System in Peoria, Information System Benefit Realization & IL, the EMR vendor, IDX Corporation (GE Healthcare, Nurse Documentation Time & 8 Seattle, WA), issued a press release stating that on Nurse Efficiency and Documentation & average, a nurse using a paper-based documentation Nurse Utilization & system spends about 30% of his/her time—more than 3 Work Sampling of Nurse Documentation Time hours out of each 12-hour shift—on documentation. -

Nursing Specialization in the UAE
Nursing Specialization in the UAE Specialization Committee Prepared by : Michelle Machon, RN, MSN Presented by: Aysha Al Mehri, RN Nursing Specialization Specialization refers to “the acquisition of a level of knowledge and skill in a particular area of nursing/ patient population which is greater than that acquired during the course of basic nursing education” (ICN, 2009) Levels of Specialty Description Education Qualification A nurse with experience in a certain area of No formal RN nursing who is recognized by the employer or education licensing authority as “specialized” in the field. Specialty specific certificate short courses e.g. one month RN wound care course Specialty nurses without general RN training (e.g. 3 year “direct RN pediatrics, psychiatry, etc.) entry” degree Post RN graduate specialty programs focusing on a 12-18 month post- Specialty RN patient population (e.g. peds, critical care, etc.) graduate diploma Specialized in a specific patient Masters level Specialty RN or population/disease process (e.g. Cardiology or program Advanced Neurosurgery Clinical Nurse Specialist) or in a Practice RN functional field of nursing (quality, education etc) “Advanced practice” nurse training resulting in Masters or PhD Advanced autonomous practitioners (Nurse level Practice RN Practitioner/Nurse Anesthetist). Possible Specialties worldwide 200 + including: Hyperbaric nursing Perioperative nursing Immunology and allergy nursing Private duty nursing Ambulatory care nursing Intravenous therapy nursing Psychiatric or mental health nursing -

Statement Comparing Anesthesiologist Assistant
STATEMENT COMPARING ANESTHESIOLOGIST ASSISTANT AND NURSE ANESTHETIST EDUCATION AND PRACTICE Committee of Origin: Anesthesia Care Team (Approved by the ASA House of Delegates on October 17, 2007, and last amended on October 17, 2012) Anesthesiologist Assistants (AA) and nurse anesthetists are both non-physician members of the Anesthesia Care Team. Their role in patient care is described in the American Society of Anesthesiologists' (ASA) Statement on the Anesthesia Care Team. The ASA document entitled Recommended Scope of Practice of Nurse Anesthetists and Anesthesiologist Assistants further details the safe limits of clinical practice. These documents state ASA's view that both AAs and anesthesia nurses have identical patient care responsibilities and technical capabilities--a view in harmony with their equivalent treatment under the Medicare Program. The proven safety of the anesthesia care team approach to anesthesia with either anesthesia nurses or AAs as the non-physician anesthetists confirms the wisdom of this view. Nevertheless, certain differences do exist between AAs and anesthesia nurses in regard to educational program prerequisites, instruction, and requirements for supervised clinical practice. Some of these differences are mischaracterized and misrepresented for the benefit of one category of provider over the other. The question that must be addressed is whether these differences in education and practice indicate superiority of one category of provider over the other in either innate ability or clinical capability. Historical Background of Nurse Anesthetists and Anesthesiologist Assistants- The Nurse Anesthesia discipline developed in the late 1800s and early 1900s out of surgeons' requests for more anesthesia providers since few physicians focused on anesthesia at that time. -
Infocus Summer 2020.Pdf
Summer 2020 The ® NCLEX & COVID-19 Inside this Issue: Practice-Academic Partnership / Member Boards Carry on During COVID-19 / The NLC & COVID-19, a Tale of Two States Summer 2020 The ® NCLEX & COVID-19 Summer 2020 Managing Editor and Writer Michael Grossenbacher | [email protected] Inside this Issue: Practice-Academic Partnership / Member Boards Carry on During COVID-19 / The NLC and COVID-19, a Tale of Two States In This Issue Contributing Editor and Writer Dawn Kappel | [email protected] 4. Practice/Academic Partnership: Designer One Answer to Prelicensure Clinical Kalona Owens | [email protected] Placements During a Pandemic 6. Lessons Learned from the Pandemic: Issues that can be Avoided if All States Founded March 15, 1978, as an independent not-for-profit organization, NCSBN was initially created to lessen the were in the NLC burdens of state governments and bring together nursing regulatory bodies (NRBs) to act and counsel together on matters of common interest. It has evolved into one of the leading voices of regulation across the world. 8. The Nurse Licensure Compact & COVID-19, NCSBN’s membership is comprised of the NRBs in the 50 a Tale of Two StatesC and COVID-19, a Tale states, the District of Columbia, and four U.S. territories — American Samoa, Guam, Northern Mariana Islands and the of Two Virgin Islands. There are three exam user members. There ® are also 27 associate members that are either NRBs or 12. The NCLEX & COVID-19 empowered regulatory authorities from other countries or territories. NCSBN and Pearson Vue Address the Mission: NCSBN empowers and supports nursing regulators in Challenges of Delivering a Valid and Secure their mandate to protect the public. -

A Methodology for Developing a Nursing Education Minimum Dataset Aziza A
University of South Florida Scholar Commons Graduate Theses and Dissertations Graduate School 11-10-2005 A Methodology for Developing a Nursing Education Minimum Dataset Aziza A. Rajab University of South Florida Follow this and additional works at: https://scholarcommons.usf.edu/etd Part of the American Studies Commons Scholar Commons Citation Rajab, Aziza A., "A Methodology for Developing a Nursing Education Minimum Dataset" (2005). Graduate Theses and Dissertations. https://scholarcommons.usf.edu/etd/826 This Dissertation is brought to you for free and open access by the Graduate School at Scholar Commons. It has been accepted for inclusion in Graduate Theses and Dissertations by an authorized administrator of Scholar Commons. For more information, please contact [email protected]. A Methodology for Developing a Nursing Education Minimum Dataset by Aziza A. Rajab A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy College of Nursing University of South Florida Major Professor: Mary E. Evans, Ph.D. Patricia Burns, Ph.D. Arthur Shapiro, Ph.D. Jason Beckstead, Ph.D. Date of Approval: November 10, 2005 Keywords: coding scheme, classification systems, Delphi, focus group, nursing database, nursing data element, nursing education, online survey, ontology, taxonomy, unified nursing language © Copyright 2005, Aziza A. Rajab Acknowledgments Thanks goes first to God Almighty, Allah the most merciful, compassionate, and gracious, for granting me the health and ability to conduct this study. A very special thank you goes to my advisor, chair, and Associate Dean for Research & Doctoral Study in the College of Nursing, Dr. Mary E. Evans for her guidance, supervision, and instruction throughout my doctoral studies and this research. -

Men in Nursing
Men in Nursing GUIDING PRINCIPLES Advancing nurse leadership 1800 061 660 acn.edu.au ACKNOWLEDGEMENTS Thanks to the Men in Nursing Working Party members: Ariel Yokota MACN Ben Chiarella MACN Ben Jenkins MACN Chris Hinder MACN Daryn Mitford MACN David Stanley MACN Haydon Cunninghame MACN Jacob Roberts MACN Kate Barnewall MACN Kylie Hasse MACN Luke Yokota MACN Chair Lee Poole MACN Deputy Chair Nick Hayward MACN Prachi Javalekar MACN Sean Woolford MACN Shauna Wilson MACN Tammie Breneger MACN ACN would also like to acknowledge the following for their contributions to developing these Guiding Principles: Adjunct Professor Kylie Ward FACN Dr Jacqui Hoepner Dr Carolyn Stapleton FACN Electronic ISBN: 978-1-925913-80-4 Print ISBN: 978-1-925913-81-1 Initial release December 2020 Second version March 2021 Third version June 2021 16.06.21 2 Australian College of Nursing FOREWORD Creating value through inclusion The Australian College of Nursing (ACN) is committed Working in the nursing profession, I am all too aware to ensuring Australia has an inclusive nursing of the outdated stereotypes and prejudice men workforce that promotes gender equity and reflects in nursing can face on a day-to-day basis. While Australia’s diverse population. At ACN, we believe things are slowly changing for the better, more work providing compassionate, empathic, high-quality and needs to be done to overcome these barriers. From person-centred care is not gendered. an early age, we need to teach boys that it’s okay for men to care. Over the past four years ACN has established various social impact initiatives to provide a platform for I am thrilled to have been the Chair of the Men nurses to make a difference to the profession and in Nursing Working Party. -

Rnlpnbyendorsementappinstru
Nevada State Board of NURSING Nevada State Board of Nursing, 5011 Meadowood Mall Way, Suite 300, Reno, NV 89502-6547 Fax: (775) 687-7707 or (702) 486-4803, Email: [email protected] www.nevadanursingboard.org; Toll Free (888) 590-6726 To practice as an nurse in Nevada, you must hold an active Nevada license. Registered Nurse/License Practical Nurse by Endorsement Requirements You must submit items 1-4 Application Instructions: 1. A completed application submitted via the Nevada Nurse Portal, including a fee of $95 (LPN) $105 (RN) (MasterCard™, Visa™, Discover™, or AmericanExpress™ debit or credit card). Fees are not refundable. 2. A copy of evidence of graduation from your nursing education program. The document you submit must indicate a nursing degree and graduation date. * All graduates of nursing programs in the United States: * If you are an RN applicant, you must submit a copy of your diploma or official transcript issued directly from the registrar to the student or to the Board, which must indicate a nursing degree and graduation date. If you are an LPN applicant, you must submit a copy of your certificate or official transcript issued directly from the registrar to the student or to the Board, which must indicate a nursing degree or graduation date. Please note that computer-generated transcripts are not acceptable. * All graduates of international nursing programs: * You must submit a copy of your transcript, which must indicate a nursing degree and graduation date. You must include a copy of the related learning experience (RLE) report, if applicable. (The Board will notify you if you will also be required to complete the CGFNS/CES8 Professional Report OR IERF** Nursing Licensure Evaluation Report for the state of Nevada). -
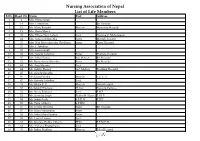
Nursing Association of Nepal List of Life Members S.No
Nursing Association of Nepal List of Life Members S.No. Regd. No. Name Post Address 1 2 Mrs. Prema Singh 2 14 Mrs. I. Mathema Bir Hospital 3 15 Ms. Manu Bangdel Matron Maternity Hospital 4 19 Mrs. Geeta Murch 5 20 Mrs. Dhana Nani Lohani Lect. Nursing C. Maharajgunj 6 24 Mrs. Saraswati Shrestha Sister Mental Hospital 7 25 Mrs. Nati Maya Shrestha (Pradhan) Sister Kanti Hospital 8 26 Mrs. I. Tuladhar 9 32 Mrs. Laxmi Singh 10 33 Mrs. Sarada Tuladhar Sister Pokhara Hospital 11 37 Mrs. Mita Thakur Ad. Matron Bir Hospital 12 42 Ms. Rameshwori Shrestha Sister Bir Hospital 13 43 Ms. Anju Sharma Lect. 14 44 Ms. Sabitry Basnet Ast. Matron Teaching Hospital 15 45 Ms. Sarada Shrestha 16 46 Ms. Geeta Pandey Matron T.U.T. H 17 47 Ms. Kamala Tuladhar Lect. 18 49 Ms. Bijaya K. C. Matron Teku Hospital 19 50 Ms.Sabitry Bhattarai D. Inst Nursing Campus 20 52 Ms. Neeta Pokharel Lect. F.H.P. 21 53 Ms. Sarmista Singh Publin H. Nurse F. H. P. 22 54 Ms. Sabitri Joshi S.P.H.N F.H.P. 23 55 Ms. Tuka Chhetry S.P.HN 24 56 Ms. Urmila Shrestha Sister Bir Hospital 25 57 Ms. Maya Manandhar Sister 26 58 Ms. Indra Maya Pandey Sister 27 62 Ms. Laxmi Thakur Lect. 28 63 Ms. Krishna Prabha Chhetri PHN F.P.M.C.H. 29 64 Ms. Archana Bhattacharya Lect. 30 65 Ms. Indira Pradhan Matron Teku Hospital S.No. Regd. No. Name Post Address 31 67 Ms. -

The Enhanced Nurse Licensure Compact and APRN Compact
The enhanced Nurse Licensure Compact and APRN Compact Presented by: Rebecca Fotsch Nicole Livanos What is the Nurse Licensure Compact? . The NLC is an interstate compact. It allows a nurse to have one multistate license (in primary state of residency) . This permits the nurse to practice in other member states (both physically and electronically) subject to each state’s practice laws 2 Mutual Recognition Model of Licensure The NLC is modeled after the driver’s license compact which follows the mutual recognition model of licensure. 3 Primary Concepts . Nurse is issued a multistate license in the declared primary state of residence (PSOR) known as the home state . Nurse holds only one multistate license issued by the home state . Nurse has a multistate licensure privilege in other Compact states (remote states) 4 . Nurses can practice in NLC Benefits for multiple states with one Telehealth license . Increases patient access to care . Enables care continuity for patients regardless of their location . Provides member states with authority to facilitate a discipline case across state lines 5 NLC Benefits for Nurses . Ability to practice in multiple states with one license . Reduces regulatory requirements by removing necessity for obtaining a license in each state . Clarifies a nurse’s authority to practice in multiple states via telehealth 6 NLC Benefits for Nursing Boards . Ability to share complaint and investigative information throughout the investigative course . Shared responsibility for patient safety not governed by geographical boundaries . Shared commitment to improving our collective ability to protect patients 7 NLC Participating States 8 Recent Drivers of Change . NLC adoption slowed . Affordable Care Act (ACA) has increased access to care for nation’s growing and aging population . -
Customer Service Skills: an Essential Tool for Every Nurse
July 2019 • Volume 23 • Number 3 • www.arsbn.org Have You Considered Serving on the State Board of Nursing? Customer Service Skills: An Essential Tool for Every Nurse Publication of the Arkansas State Board of Nursing 2 501.686.2700 The ASBN Contents Update circulation PUBLISHED BY includes Arkansas State Board of Nursing Director’s Message • University Tower Building 4 over 57,000 1123 S. University, Suite 800 licensed nurses Little Rock, Arkansas 72204 Telephone: 501.686.2700 and student Fax: 501.686.2714 nurses in www.arsbn.org President’s Message — Never Forget • 6 Arkansas. BOARD MEMBERS PRESIDENT Ramonda Housh, APRN VICE PRESIDENT Lance Lindow, RN SECRETARY Kaci Bohn, Consumer Rep. Board Business • 9 TREASURER Janice Ivers, RN Mike Burdine, RN Neldia Dycus, RN Jasper Fultz, LPN Melanie Garner, LPN Customer Service Skills: Yolanda Green, LPN An Essential Tool for Every Nurse • Stacie Hipp, APRN 10 Pamela Leal, Rep. of the Older Population Renee Mihalko-Corbitt, APRN Rachel Sims, RN APRN Corner: National Certification, Renewals and Pharmacotherapeutics The mission of the Arkansas State Board of Nursing is to protect the public and act Continuing Education •12 as their advocate by effectively regulating the practice of nursing. DIRECTOR Sue A. Tedford, MNSc, APRN I Think My Coworker EDITOR LouAnn Walker Is Impaired –What Do I Do? •14 Information published in the ASBN Update is not copyrighted and may be reproduced. The Board would appreciate credit for the material used. Have You Considered Direct ASBN Update questions or comments to: Editor, Arkansas State Board of Nursing, Serving on the State 1123 S. -

Lawrlwytho'r Atodiad Gwreiddiol
Operational services structure April 2021 14/04/2021 Operational Leadership Structures Director of Operations Director of Nursing & Quality Medical Director Lee McMenamy Joanne Hiley Dr Tessa Myatt Medical Operations Operations Clinical Director of Operations Deputy Director of Nursing & Deputy Medical Director Hazel Hendriksen Governance Dr Jose Mathew Assistant Clinical Director Assistant Director of Assistant Clinical DWiraerctringor ton & Halton Operations Corporate Corporate Lorna Pink Assistant Assistant Director Julie Chadwick Vacant Clinical Director of Nursing, AHP & Associate Clinical Director Governance & Professional Warrington & Halton Compliance Standards Assistant Director of Operations Assistant Clinical Director Dr Aravind Komuravelli Halton & Warrington Knowsley Lee Bloomfield Claire Hammill Clare Dooley Berni Fay-Dunkley Assistant Director of Operations Knowsley Associate Medical Director Nicky Over Assistant Clinical Director Allied Health Knowsley Assistant Director of Sefton Professional Dr Ashish Kumar AssiOstapenrta Dtiironesc tKnor oofw Oslpeeyr ations Sara Harrison Lead Nicola Over Sefton James Hester Anne Tattersall Assistant Clinical Director Associate Clinical Director Assistant Director of St Helens & Knowsley Inpatients St Helens Operations Sefton Debbie Tubey Dr Raj Madgula AssistanAt nDniree Tcatttore ofrs aOllp erations Head of St Helens & Knowsley Inpatients Safeguarding Tim McPhee Assistant Clinical Director Sarah Shaw Assistant Director of Associate Medical Director Operations St Helens Mental Health -
Key Performance Indicators a Guide to Choosing, Developing and Using Kpis for Clinical Nurse/Midwife Specialists and Advanced Nurse/Midwife Practitioners
DISCUSSION PAPER 3 Key Performance Indicators A Guide to Choosing, Developing and Using KPIs for Clinical Nurse/Midwife Specialists and Advanced Nurse/Midwife Practitioners DECEMBER 2010 KEY PERFORMANCE INDICATORS Introduction Development of healthcare in Ireland, including its structures and delivery of care, is driven by the safety and quality agenda that has become increasingly explicit in the last ten years (Department of Health and Children 2008). Nurses and midwives have contributed and continue to contribute to the enhancement of patient care and this contribution can be captured and articulated by focusing on their clinical outcomes. The National Council for the Professional Development of Nursing and Midwifery has provided focused guidance on measuring clinical outcomes in its discussion paper Clinical Outcomes (National Council 2010a). Building on that guidance, the present discussion paper has been developed as a resource for clinical nurse/midwife specialists (CNSs/CMSs) and advanced nurse/midwife practitioners (ANPs/AMPs) wishing to articulate and clarify their contribution to patient care. The need for this specialised guidance emerged from a recent evaluation of CNSs’/CMSs’ and ANPs’/AMPs’ clinical outcomes, and the final report on the evaluation contains a recommendation concerning the development of key performance indicators relevant to the roles of these nurses and midwives. The Evaluation of Clinical Nurse/Midwife Specialists and Advanced Nurse/Midwife Practitioners in Ireland Known as the SCAPE Project, the examination of CNSs’/CMSs’ and ANPs’/AMPs’ clinical outcomes involved the use of an extensive variety of research methods and date collection tools (Begley et al 2010). The study demonstrated that patient care provided by CNSs/CMSs and ANPs/AMPs improved patient outcomes, as well as being safe and cost-neutral.