Immuno 2010 No. 4
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

"Epitope Mapping: B-Cell Epitopes". In: Encyclopedia of Life Sciences
Epitope Mapping: B-cell Advanced article Epitopes Article Contents . Introduction GE Morris, Wolfson Centre for Inherited Neuromuscular Disease RJAH Orthopaedic Hospital, . What Is a B-cell Epitope? . Epitope Mapping Methods Oswestry, UK and Keele University, Keele, Staffordshire, UK . Applications Immunoglobulin molecules are folded to present a surface structure complementary to doi: 10.1002/9780470015902.a0002624.pub2 a surface feature on the antigen – the epitope is this feature of the antigen. Epitope mapping is the process of locating the antibody-binding site on the antigen, although the term is also applied more broadly to receptor–ligand interactions unrelated to the immune system. Introduction formed of highly convoluted peptide chains, so that resi- dues that lie close together on the protein surface are often Immunoglobulin molecules are folded in a way that as- far apart in the amino acid sequence (Barlow et al., 1986). sembles sequences from the variable regions of both the Consequently, most epitopes on native, globular proteins heavy and light chains into a surface feature (comprised of are conformation-dependent and they disappear if the up to six complementarity-determining regions (CDRs)) protein is denatured or fragmented. Sometimes, by acci- that is complementary in shape to a surface structure on the dent or design, antibodies are produced against linear antigen. These two surface features, the ‘paratope’ on the (sequential) epitopes that survive denaturation, though antibody and the ‘epitope’ on the antigen, may have a cer- such antibodies usually fail to recognize the native protein. tain amount of flexibility to allow an ‘induced fit’ between The simplest way to find out whether an epitope is confor- them. -

Transfusion Problems in Hemolytic Anemias*
Transfusion Problems in Hemolytic Anemias* ALI A. HOSSAIN! Department of Pathdlogy, Medical College of Virginia, Richmond 23219 All hemolytic anemias feature shortened red cell Extrinsic Mechanisms survival due to premature hemolysis of the cell. For the Those hemolytic anemias which are due to extrinsic purposes of this presentation, we may classify the factors may be classified, further, as non-immune or hemolytic anemias, most broadly, according to the immune. Non-immune mechanisms include a) drugs mechanisms leading to hemolysis. and chemicals (phenylhydrazine, naphthalene, lead, snake venoms); b) physical agents (heat); c) bacteria Intrinsic Mechanisms and parasites (hemolytic streptococci, Clostridium Hemolytic anemias due to intrinsically defective welchii, Bartonella, plasmodia); and d) acquired sen erythrocytes are essentially of three types. First are sitivity to penicillin, methylodopa, Keftin®, or fava those anemias in which the red cells are defective due plant as examples. Some of the agents in this. last to lack of an essential factor, eg, pernicious anemia group serve to lyse the cells, either through duect in relapse. The second type includes those in which action or by formation of antibodies. the red cells have an abnormal shape because of an These hemolytic anemias due to extrinsic factors inherited error in the chemical makeup of the hemo of the non-immune variety present no transfusion globin molecules; eg, sickle cells, elliptocytes, sphero problem for the Blood Bank. However, it ~~st b.e cytes, and the target -

Hemolytic Disease of the Newborn
Intensive Care Nursery House Staff Manual Hemolytic Disease of the Newborn INTRODUCTION and DEFINITION: Hemolytic Disease of the Newborn (HDN), also known as erythroblastosis fetalis, isoimmunization, or blood group incompatibility, occurs when fetal red blood cells (RBCs), which possess an antigen that the mother lacks, cross the placenta into the maternal circulation, where they stimulate antibody production. The antibodies return to the fetal circulation and result in RBC destruction. DIFFERENTIAL DIAGNOSIS of hemolytic anemia in a newborn infant: -Isoimmunization -RBC enzyme disorders (e.g., G6PD, pyruvate kinase deficiency) -Hemoglobin synthesis disorders (e.g., alpha-thalassemias) -RBC membrane abnormalities (e.g., hereditary spherocytosis, elliptocytosis) -Hemangiomas (Kasabach Merritt syndrome) -Acquired conditions, such as sepsis, infections with TORCH or Parvovirus B19 (anemia due to RBC aplasia) and hemolysis secondary to drugs. ISOIMMUNIZATION A. Rh disease (Rh = Rhesus factor) (1) Genetics: Rh positive (+) denotes presence of D antigen. The number of antigenic sites on RBCs varies with genotype. Prevalence of genotype varies with the population. Rh negative (d/d) individuals comprise 15% of Caucasians, 5.5% of African Americans, and <1% of Asians. A sensitized Rh negative mother produces anti-Rh IgG antibodies that cross the placenta. Risk factors for antibody production include 2nd (or later) pregnancies*, maternal toxemia, paternal zygosity (D/D rather than D/d), feto-maternal compatibility in ABO system and antigen load. (2) Clinical presentation of HDN varies from mild jaundice and anemia to hydrops fetalis (with ascites, pleural and pericardial effusions). Because the placenta clears bilirubin, the chief risk to the fetus is anemia. Extramedullary hematopoiesis (due to anemia) results in hepatosplenomegaly. -

A Newly Recognized Blood Group in Domestic Shorthair Cats: the Mik Red Cell Antigen
J Vet Intern Med 2007;21:287–292 A Newly Recognized Blood Group in Domestic Shorthair Cats: The Mik Red Cell Antigen Nicole M. Weinstein, Marie-Claude Blais, Kimberly Harris, Donna A. Oakley, Lillian R. Aronson, and Urs Giger Background: Naturally occurring alloantibodies produced against A and B red cell antigens in cats can cause acute hemolytic transfusion reactions. Blood incompatibilities, unrelated to the AB blood group system, have also been suspected after blood transfusions through routine crossmatch testing or as a result of hemolytic transfusion reactions. Hypothesis: Incompatible crossmatch results among AB compatible cats signify the presence of a naturally occurring alloantibody against a newly identified blood antigen in a group of previously never transfused blood donor cats. The associated alloantibody is clinically important based upon a hemolytic transfusion reaction after inadvertent transfusion of red cells expressing this red cell antigen in a feline renal transplant recipient that lacks this red cell antigen. Methods: Blood donor and nonblood donor cats were evaluated for the presence of auto- and alloantibodies using direct antiglobulin and crossmatch tests, respectively, and were blood typed for AB blood group status. Both standard tube and novel gel column techniques were used. Results: Plasma from 3 of 65 cats and 1 feline renal transplant recipient caused incompatible crossmatch test results with AB compatible erythrocytes indicating these cats formed an alloantibody against a red cell antigen they lack, termed Mik. The 3 donors and the renal transplant recipient were crossmatch-compatible with one another. Tube and gel column crossmatch test results were similar. Conclusions and Clinical Importance: The absence of this novel Mik red cell antigen can be associated with naturally occurring anti-Mik alloantibodies and can elicit an acute hemolytic transfusion reaction after an AB-matched blood transfusion. -

Ige – the Main Player of Food Allergy
DDMOD-431; No of Pages 8 Vol. xxx, No. xx 2016 Drug Discovery Today: Disease Models Editors-in-Chief Jan Tornell – AstraZeneca, Sweden DRUG DISCOVERY Andrew McCulloch – University of California, SanDiego, USA TODAY DISEASE MODELS IgE – the main player of food allergy 1 2,3 2 Henrike C.H. Broekman , Thomas Eiwegger , Julia Upton , 4, Katrine L. Bøgh * 1 Department of Dermatology/Allergology, University Medical Centre Utrecht (UMCU), Utrecht, The Netherlands 2 Division of Immunology and Allergy, Food Allergy and Anaphylaxis Program, The Department of Paediatrics, Hospital for Sick Children, Toronto, Canada 3 Research Institute, Physiology and Experimental Medicine, The University of Toronto, Toronto, Canada 4 National Food Institute, Technical University of Denmark, Søborg, Denmark Food allergy is a growing problem worldwide, presently Section editor: affecting 2–4% of adults and 5–8% of young children. IgE Michelle Epstein – Medical University of Vienna, is a key player in food allergy. Consequently huge Department of Dermatology, DIAID, Experimental Allergy, Waehringer Guertel 18-20, Room 4P9.02, A1090, efforts have been made to develop tests to detect Vienna, Austria. either the presence of IgE molecules, their allergen binding sites or their functionality, in order to provide allergen ingestion [1], and involve one or more of the follow- information regarding the patient’s food allergy. The ing systems; the skin (pruritus, urticaria, or angioedema), the ultimate goal is to develop tools that are capable of gastro-intestinal tract (diarrhea, vomiting, contractions, in- creased bowel movement), the respiratory tract (asthma at- discriminating between asymptomatic sensitization tack, hoarseness, stridor/laryngeal angioedema) or the and a clinically relevant food allergy, and between cardiovascular system (dizziness, drop in blood pressure, loss different allergic phenotypes in an accurate and trust- of consciousness) [2,3]. -

Protein Epitope Mapping by Mass Spectrometry
Anal. Chem. 1994,66, 3723-3726 Protein Epitope Mapping By Mass Spectrometry Ylngmlng Zhao and Brian T. Chalt’ The Rockefeller University, 1230 York Avenue, New York, New York 10021 A mass spectrometricmethod is described for the rapid mapping antigen bound to an antibody. Alternatively, these workers of linear epitopes in proteins that are bound by monoclonal subjected the peptide to proteolytic digestion and identified antibodies. The method consists of three steps. In the first products that bound to the immobilized antibody. In both step, an antigen protein is digested by a proteolytic enzyme to cases, the peptides of interest were identified by 2Wfplasma produce an appropriate set of peptide fragments. In the second desorption mass spectrometry. step, peptide fragments containing the linear epitope are selected Matrix-assisted laser desorption mass spectrometry (MAL- and separated from the pool of peptide fragments by immu- DI-MS) is a recently developed method for measuring the noprecipitation with the monoclonal antibody. In the final molecular weights of peptides and proteins.12-14 The technique step, the immunoprecipitated peptides are identified by matrix- allows the accurate (better than O.l%), rapid (<1 min), and assisted laser desorption mass spectrometry. The method sensitive (<1 pmol) determination of the molecular weights allows the rapid determination of antigenic sites without tedious of components of complex mixtures of peptides. MALDI- peptide synthesis or protein mutagenesis. The approach is MS is finding wide use for the rapid identification of proteins demonstrated through the mapping of epitopes in two peptides and the elucidation of their primary structures (in particular, (melittin and glucagon-like peptide-1 7-37) against which the definition of posttranslational modifications.) monoclonal antibodies were raised. -
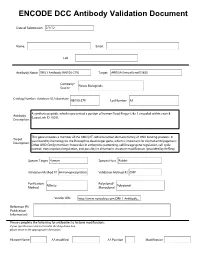
ENCODE DCC Antibody Validation Document
ENCODE DCC Antibody Validation Document Date of Submission Name: Email: Lab Antibody Name: Target: Company/ Source: Catalog Number, database ID, laboratory Lot Number Antibody Description: Target Description: Species Target Species Host Validation Method #1 Validation Method #2 Purification Polyclonal/ Method Monoclonal Vendor URL: Reference (PI/ Publication Information) Please complete the following for antibodies to histone modifications: if your specifications are not listed in the drop-down box, please write-in the appropriate information Histone Name AA modified AA Position Modification Validation #1 Analysis Insert Validation Image (click here) ARID3A (NB100-279) & (sc-8821) Immunoblot / Immunoprecipitation A. MW (kD) B. MW (kD) C. MW (kD) D. MW (kD) 150 150 150 150 100 100 100 100 75 75 75 75 50 50 50 50 38 38 38 38 25 25 25 20 20 20 25 15 15 15 15 Lane : 1 2 3 4 Lane : 1 2 3 Lane : 1 2 Lane : 1 2 3 A. Western Blot using NB100-279 on nuclear lysates from cell lines GM12878 (Lane1), K562 (Lane2), HeLaS3 (Lane3), and HepG2 (Lane4). B. Immunoprecipitation was performed on nuclear lysates from K562 cells using antibody NB100-279. Lane1: Nuclear lysate. Lane 3: Bound material from control immunoprecipitation with rabbit IgG. Lane 2: Bound material from immunoprecipitation with NB100-279. C. Western Blot using sc-8821 on nuclear lysates from cell lines GM12878 (Lane1), K562 (Lane2). D. Immunoprecipitation was performed on nuclear lysates from K562 cells using antibody sc-8821 and immunoblot with NB100-279. Lane1: Nuclear lysate. Lane 2: Bound material from immunoprecipitation with sc-8821. Lane 3: Bound material from control immunoprecipitation with Goat IgG. -

Flow Reagents Single Color Antibodies CD Chart
CD CHART CD N° Alternative Name CD N° Alternative Name CD N° Alternative Name Beckman Coulter Clone Beckman Coulter Clone Beckman Coulter Clone T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells CD1a T6, R4, HTA1 Act p n n p n n S l CD99 MIC2 gene product, E2 p p p CD223 LAG-3 (Lymphocyte activation gene 3) Act n Act p n CD1b R1 Act p n n p n n S CD99R restricted CD99 p p CD224 GGT (γ-glutamyl transferase) p p p p p p CD1c R7, M241 Act S n n p n n S l CD100 SEMA4D (semaphorin 4D) p Low p p p n n CD225 Leu13, interferon induced transmembrane protein 1 (IFITM1). p p p p p CD1d R3 Act S n n Low n n S Intest CD101 V7, P126 Act n p n p n n p CD226 DNAM-1, PTA-1 Act n Act Act Act n p n CD1e R2 n n n n S CD102 ICAM-2 (intercellular adhesion molecule-2) p p n p Folli p CD227 MUC1, mucin 1, episialin, PUM, PEM, EMA, DF3, H23 Act p CD2 T11; Tp50; sheep red blood cell (SRBC) receptor; LFA-2 p S n p n n l CD103 HML-1 (human mucosal lymphocytes antigen 1), integrin aE chain S n n n n n n n l CD228 Melanotransferrin (MT), p97 p p CD3 T3, CD3 complex p n n n n n n n n n l CD104 integrin b4 chain; TSP-1180 n n n n n n n p p CD229 Ly9, T-lymphocyte surface antigen p p n p n -

Blood Bank I D
The Osler Institute Blood Bank I D. Joe Chaffin, MD Bonfils Blood Center, Denver, CO The Fun Just Never Ends… A. Blood Bank I • Blood Groups B. Blood Bank II • Blood Donation and Autologous Blood • Pretransfusion Testing C. Blood Bank III • Component Therapy D. Blood Bank IV • Transfusion Complications * Noninfectious (Transfusion Reactions) * Infectious (Transfusion-transmitted Diseases) E. Blood Bank V (not discussed today but available at www.bbguy.org) • Hematopoietic Progenitor Cell Transplantation F. Blood Bank Practical • Management of specific clinical situations • Calculations, Antibody ID and no-pressure sample questions Blood Bank I Blood Groups I. Basic Antigen-Antibody Testing A. Basic Red Cell-Antibody Interactions 1. Agglutination a. Clumping of red cells due to antibody coating b. Main reaction we look for in Blood Banking c. Two stages: 1) Coating of cells (“sensitization”) a) Affected by antibody specificity, electrostatic RBC charge, temperature, amounts of antigen and antibody b) Low Ionic Strength Saline (LISS) decreases repulsive charges between RBCs; tends to enhance cold antibodies and autoantibodies c) Polyethylene glycol (PEG) excludes H2O, tends to enhance warm antibodies and autoantibodies. 2) Formation of bridges a) Lattice structure formed by antibodies and RBCs b) IgG isn’t good at this; one antibody arm must attach to one cell and other arm to the other cell. c) IgM is better because of its pentameric structure. P}Chaffin (12/28/11) Blood Bank I page 1 Pathology Review Course 2. Hemolysis a. Direct lysis of a red cell due to antibody coating b. Uncommon, but equal to agglutination. 1) Requires complement fixation 2) IgM antibodies do this better than IgG. -

Análise Integrativa De Perfis Transcricionais De Pacientes Com
UNIVERSIDADE DE SÃO PAULO FACULDADE DE MEDICINA DE RIBEIRÃO PRETO PROGRAMA DE PÓS-GRADUAÇÃO EM GENÉTICA ADRIANE FEIJÓ EVANGELISTA Análise integrativa de perfis transcricionais de pacientes com diabetes mellitus tipo 1, tipo 2 e gestacional, comparando-os com manifestações demográficas, clínicas, laboratoriais, fisiopatológicas e terapêuticas Ribeirão Preto – 2012 ADRIANE FEIJÓ EVANGELISTA Análise integrativa de perfis transcricionais de pacientes com diabetes mellitus tipo 1, tipo 2 e gestacional, comparando-os com manifestações demográficas, clínicas, laboratoriais, fisiopatológicas e terapêuticas Tese apresentada à Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo para obtenção do título de Doutor em Ciências. Área de Concentração: Genética Orientador: Prof. Dr. Eduardo Antonio Donadi Co-orientador: Prof. Dr. Geraldo A. S. Passos Ribeirão Preto – 2012 AUTORIZO A REPRODUÇÃO E DIVULGAÇÃO TOTAL OU PARCIAL DESTE TRABALHO, POR QUALQUER MEIO CONVENCIONAL OU ELETRÔNICO, PARA FINS DE ESTUDO E PESQUISA, DESDE QUE CITADA A FONTE. FICHA CATALOGRÁFICA Evangelista, Adriane Feijó Análise integrativa de perfis transcricionais de pacientes com diabetes mellitus tipo 1, tipo 2 e gestacional, comparando-os com manifestações demográficas, clínicas, laboratoriais, fisiopatológicas e terapêuticas. Ribeirão Preto, 2012 192p. Tese de Doutorado apresentada à Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo. Área de Concentração: Genética. Orientador: Donadi, Eduardo Antonio Co-orientador: Passos, Geraldo A. 1. Expressão gênica – microarrays 2. Análise bioinformática por module maps 3. Diabetes mellitus tipo 1 4. Diabetes mellitus tipo 2 5. Diabetes mellitus gestacional FOLHA DE APROVAÇÃO ADRIANE FEIJÓ EVANGELISTA Análise integrativa de perfis transcricionais de pacientes com diabetes mellitus tipo 1, tipo 2 e gestacional, comparando-os com manifestações demográficas, clínicas, laboratoriais, fisiopatológicas e terapêuticas. -

Investigation of Four Genes Responsible for Autosomal Recessive Congenital Cataract and Highly Expressed in the Brain in Four Unrelated Tunisian Families
Open Journal of Ophthalmology, 2012, 2, 64-70 http://dx.doi.org/10.4236/ojoph.2012.23014 Published Online August 2012 (http://www.SciRP.org/journal/ojoph) Investigation of Four Genes Responsible for Autosomal Recessive Congenital Cataract and Highly Expressed in the Brain in Four Unrelated Tunisian Families Manèl Chograni1, Myriam Chaabouni1,2, Faouzi Maazoul2, Habiba Chaabouni Bouhamed1,2* 1Laboratoire de Génétique Humaine, Faculté de Médecine de Tunis, University Tunis Elmanar, Tunis, Tunisia; 2Congenital and Hereditary Disorders Department, Charles Nicolle Hospital, Tunis, Tunisia. Email: *[email protected] Received March 14th, 2012; revised April 28th, 2012; accepted May 11th, 2012 ABSTRACT Purpose: To identify the causative gene for phenotypes associating autosomal recessive congenital cataract, mental re- tardation and congenital cataract, mental retardation and microcephaly in four unrelated Tunisian families. Methods: Four genes (EPHA2, GALK1, GCNT2, and CRYBB1) were selected based on their expression in human brain and their known or putative function. Linkage analysis were performed for the four genes in multiple affected and unaffected families’ members and results were explored by the GeneMapper ID v3.2 software. Results: No linkage was identified for the four studied genes in the four families. Affected members of each family did not share common haplotypes in corresponding candidate regions containing selected gene. Conclusion: Although the four studied genes were reported responsible for autosomal recessive congenital cataract and highly expressed in the human brain, we report no linkage for EPHA2, GALK1, GCNT2, and CRYBB1 genes in four families with congenital cataract, mental retardation and con- genital cataract, mental retardation and microcephaly. Keywords: Congenital Cataract; Mental Retardation; Microcephaly; Autosomal Recessive; Association; Linkage Study 1.