Highly Accurate and Reproducible Diagnosis of Peanut Allergy Using Epitope Mapping
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

"Epitope Mapping: B-Cell Epitopes". In: Encyclopedia of Life Sciences
Epitope Mapping: B-cell Advanced article Epitopes Article Contents . Introduction GE Morris, Wolfson Centre for Inherited Neuromuscular Disease RJAH Orthopaedic Hospital, . What Is a B-cell Epitope? . Epitope Mapping Methods Oswestry, UK and Keele University, Keele, Staffordshire, UK . Applications Immunoglobulin molecules are folded to present a surface structure complementary to doi: 10.1002/9780470015902.a0002624.pub2 a surface feature on the antigen – the epitope is this feature of the antigen. Epitope mapping is the process of locating the antibody-binding site on the antigen, although the term is also applied more broadly to receptor–ligand interactions unrelated to the immune system. Introduction formed of highly convoluted peptide chains, so that resi- dues that lie close together on the protein surface are often Immunoglobulin molecules are folded in a way that as- far apart in the amino acid sequence (Barlow et al., 1986). sembles sequences from the variable regions of both the Consequently, most epitopes on native, globular proteins heavy and light chains into a surface feature (comprised of are conformation-dependent and they disappear if the up to six complementarity-determining regions (CDRs)) protein is denatured or fragmented. Sometimes, by acci- that is complementary in shape to a surface structure on the dent or design, antibodies are produced against linear antigen. These two surface features, the ‘paratope’ on the (sequential) epitopes that survive denaturation, though antibody and the ‘epitope’ on the antigen, may have a cer- such antibodies usually fail to recognize the native protein. tain amount of flexibility to allow an ‘induced fit’ between The simplest way to find out whether an epitope is confor- them. -

Ige – the Main Player of Food Allergy
DDMOD-431; No of Pages 8 Vol. xxx, No. xx 2016 Drug Discovery Today: Disease Models Editors-in-Chief Jan Tornell – AstraZeneca, Sweden DRUG DISCOVERY Andrew McCulloch – University of California, SanDiego, USA TODAY DISEASE MODELS IgE – the main player of food allergy 1 2,3 2 Henrike C.H. Broekman , Thomas Eiwegger , Julia Upton , 4, Katrine L. Bøgh * 1 Department of Dermatology/Allergology, University Medical Centre Utrecht (UMCU), Utrecht, The Netherlands 2 Division of Immunology and Allergy, Food Allergy and Anaphylaxis Program, The Department of Paediatrics, Hospital for Sick Children, Toronto, Canada 3 Research Institute, Physiology and Experimental Medicine, The University of Toronto, Toronto, Canada 4 National Food Institute, Technical University of Denmark, Søborg, Denmark Food allergy is a growing problem worldwide, presently Section editor: affecting 2–4% of adults and 5–8% of young children. IgE Michelle Epstein – Medical University of Vienna, is a key player in food allergy. Consequently huge Department of Dermatology, DIAID, Experimental Allergy, Waehringer Guertel 18-20, Room 4P9.02, A1090, efforts have been made to develop tests to detect Vienna, Austria. either the presence of IgE molecules, their allergen binding sites or their functionality, in order to provide allergen ingestion [1], and involve one or more of the follow- information regarding the patient’s food allergy. The ing systems; the skin (pruritus, urticaria, or angioedema), the ultimate goal is to develop tools that are capable of gastro-intestinal tract (diarrhea, vomiting, contractions, in- creased bowel movement), the respiratory tract (asthma at- discriminating between asymptomatic sensitization tack, hoarseness, stridor/laryngeal angioedema) or the and a clinically relevant food allergy, and between cardiovascular system (dizziness, drop in blood pressure, loss different allergic phenotypes in an accurate and trust- of consciousness) [2,3]. -

Protein Epitope Mapping by Mass Spectrometry
Anal. Chem. 1994,66, 3723-3726 Protein Epitope Mapping By Mass Spectrometry Ylngmlng Zhao and Brian T. Chalt’ The Rockefeller University, 1230 York Avenue, New York, New York 10021 A mass spectrometricmethod is described for the rapid mapping antigen bound to an antibody. Alternatively, these workers of linear epitopes in proteins that are bound by monoclonal subjected the peptide to proteolytic digestion and identified antibodies. The method consists of three steps. In the first products that bound to the immobilized antibody. In both step, an antigen protein is digested by a proteolytic enzyme to cases, the peptides of interest were identified by 2Wfplasma produce an appropriate set of peptide fragments. In the second desorption mass spectrometry. step, peptide fragments containing the linear epitope are selected Matrix-assisted laser desorption mass spectrometry (MAL- and separated from the pool of peptide fragments by immu- DI-MS) is a recently developed method for measuring the noprecipitation with the monoclonal antibody. In the final molecular weights of peptides and proteins.12-14 The technique step, the immunoprecipitated peptides are identified by matrix- allows the accurate (better than O.l%), rapid (<1 min), and assisted laser desorption mass spectrometry. The method sensitive (<1 pmol) determination of the molecular weights allows the rapid determination of antigenic sites without tedious of components of complex mixtures of peptides. MALDI- peptide synthesis or protein mutagenesis. The approach is MS is finding wide use for the rapid identification of proteins demonstrated through the mapping of epitopes in two peptides and the elucidation of their primary structures (in particular, (melittin and glucagon-like peptide-1 7-37) against which the definition of posttranslational modifications.) monoclonal antibodies were raised. -
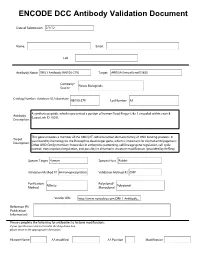
ENCODE DCC Antibody Validation Document
ENCODE DCC Antibody Validation Document Date of Submission Name: Email: Lab Antibody Name: Target: Company/ Source: Catalog Number, database ID, laboratory Lot Number Antibody Description: Target Description: Species Target Species Host Validation Method #1 Validation Method #2 Purification Polyclonal/ Method Monoclonal Vendor URL: Reference (PI/ Publication Information) Please complete the following for antibodies to histone modifications: if your specifications are not listed in the drop-down box, please write-in the appropriate information Histone Name AA modified AA Position Modification Validation #1 Analysis Insert Validation Image (click here) ARID3A (NB100-279) & (sc-8821) Immunoblot / Immunoprecipitation A. MW (kD) B. MW (kD) C. MW (kD) D. MW (kD) 150 150 150 150 100 100 100 100 75 75 75 75 50 50 50 50 38 38 38 38 25 25 25 20 20 20 25 15 15 15 15 Lane : 1 2 3 4 Lane : 1 2 3 Lane : 1 2 Lane : 1 2 3 A. Western Blot using NB100-279 on nuclear lysates from cell lines GM12878 (Lane1), K562 (Lane2), HeLaS3 (Lane3), and HepG2 (Lane4). B. Immunoprecipitation was performed on nuclear lysates from K562 cells using antibody NB100-279. Lane1: Nuclear lysate. Lane 3: Bound material from control immunoprecipitation with rabbit IgG. Lane 2: Bound material from immunoprecipitation with NB100-279. C. Western Blot using sc-8821 on nuclear lysates from cell lines GM12878 (Lane1), K562 (Lane2). D. Immunoprecipitation was performed on nuclear lysates from K562 cells using antibody sc-8821 and immunoblot with NB100-279. Lane1: Nuclear lysate. Lane 2: Bound material from immunoprecipitation with sc-8821. Lane 3: Bound material from control immunoprecipitation with Goat IgG. -
![Epitope Mapping of an Uncertain Endogenous Antigen Implies Secretogranin II Peptide Splicing [Version 2; Peer Review: 1 Approved, 2 Approved with Reservations]](https://docslib.b-cdn.net/cover/9315/epitope-mapping-of-an-uncertain-endogenous-antigen-implies-secretogranin-ii-peptide-splicing-version-2-peer-review-1-approved-2-approved-with-reservations-409315.webp)
Epitope Mapping of an Uncertain Endogenous Antigen Implies Secretogranin II Peptide Splicing [Version 2; Peer Review: 1 Approved, 2 Approved with Reservations]
F1000Research 2019, 8:1732 Last updated: 26 JUL 2021 RESEARCH ARTICLE Epitope mapping of an uncertain endogenous antigen implies secretogranin II peptide splicing [version 2; peer review: 1 approved, 2 approved with reservations] David R. Howlett 1, Iain J. Clarke2, Russell P. Newton3, John E. Hart4 1Wolfson Centre for Age Related Disease, Kings College London, London, SE1 1UL, UK 2School of Agriculture and Veterinary Science, Melbourne University, Parkville, Victoria, VIC 3010, Australia 3Biochemistry Group, Institute of Life Sciences, Medical School, Swansea University, Swansea, Wales, SA2 8PP, UK 4Endocrine Pharmaceuticals Ltd, Tadley, Hampshire, RG26 3TA, UK v2 First published: 09 Oct 2019, 8:1732 Open Peer Review https://doi.org/10.12688/f1000research.20633.1 Latest published: 05 Dec 2019, 8:1732 https://doi.org/10.12688/f1000research.20633.2 Reviewer Status Invited Reviewers Abstract Background: The search for a tissue-mass reducing reproductive 1 2 3 hormone involved a bioassay-guided physicochemical fractionation of sheep blood plasma. This brought forth a candidate protein whose version 2 apparent mass on gels and in mass spectrometry (MS) was 7-8 kDa, (revision) report report implying a polypeptide of ~70 residues. Four purification runs gave 05 Dec 2019 Edman N-terminal sequences relating to 1MKPLTGKVKEFNNI14. This is bioinformatically obscure and has been resistant to molecular version 1 biological investigation. The sequence was synthesized as the peptide 09 Oct 2019 report report EPL001, against which was raised a goat polyclonal antiserum, G530. Used in an antigen capture campaign, G530 pointed to the existence of a novel derivative of secretogranin II (SgII), the neuroendocrine 1. -

Molecular Immunology a Machine-Learning Approach for Predicting B-Cell Epitopes
Molecular Immunology 46 (2009) 840–847 Contents lists available at ScienceDirect Molecular Immunology journal homepage: www.elsevier.com/locate/molimm A machine-learning approach for predicting B-cell epitopes Nimrod D. Rubinstein, Itay Mayrose, Tal Pupko ∗ Department of Cell Research and Immunology, Tel Aviv University, Tel Aviv 69978, Israel article info abstract Article history: The immune activity of an antibody is directed against a specific region on its target antigen known as Received 25 May 2008 the epitope. Numerous immunodetection and immunotheraputics applications are based on the ability of Received in revised form 23 July 2008 antibodies to recognize epitopes. The detection of immunogenic regions is often an essential step in these Accepted 7 September 2008 applications. The experimental approaches used for detecting immunogenic regions are often laborious Available online 22 October 2008 and resource-intensive. Thus, computational methods for the prediction of immunogenic regions allevi- ate this drawback by guiding the experimental procedures. In this work we developed a computational Keywords: method for the prediction of immunogenic regions from either the protein three-dimensional structure Antigen Antibody or sequence when the structure is unavailable. The method implements a machine-learning algorithm Epitope that was trained to recognize immunogenic patterns based on a large benchmark dataset of validated Immunogenic regions epitopes derived from antigen structures and sequences. We compare our method to other available tools Prediction that perform the same task and show that it outperforms them. Properties © 2008 Elsevier Ltd. All rights reserved. Surface 1. Introduction Woods, 1981; Karplus and Schulz, 1985; Kolaskar and Tongaonkar, 1990; Kulkarni-Kale et al., 2005; Parker et al., 1986; Pellequer et The ability of an antibody to specifically bind an antigen is al., 1991). -

Polyclonal Epitope Cartography Reveals the Temporal Dynamics and Diversity of Human Antibody Responses to H5N1 Vaccination
bioRxiv preprint doi: https://doi.org/10.1101/2020.06.16.155754; this version posted June 17, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Polyclonal epitope cartography reveals the temporal dynamics and diversity of human antibody responses to H5N1 vaccination Julianna Han1, Aaron J. Schmitz2, Sara T. Richey1, Ya-Nan Dai2, Hannah L. Turner1, Bassem M. Mohammed2, Daved H. Fremont2,3,4, Ali H. Ellebedy2,4, Andrew B. Ward1,5* 1Department of Integrative Structural and Computational Biology, The Scripps Research Institute, La Jolla, CA, 92037, USA. 2Department of Pathology and Immunology, Washington University School of Medicine, St Louis, MO, 63110, USA. 3Department of Biochemistry & Molecular Biophysics, Washington University School of Medicine, St. Louis, MO, 63110, USA. 4Department of Molecular Microbiology, Washington University School of Medicine, St. Louis, MO, 63110, USA. 5Lead contact *Correspondence: [email protected] (A.B.W.) SUMMARY Novel influenza A virus (IAV) strains elicit recall immune responses to conserved epitopes, making them favorable antigenic choices for universal influenza virus vaccines. Evaluating these immunogens requires a thorough understanding of the antigenic sites targeted by the polyclonal antibody (pAb) response, which single particle electron microscopy (EM) can sensitively detect. Here, we employed EM polyclonal epitope mapping (EMPEM) to extensively characterize the pAb response to hemagglutinin (HA) after H5N1 immunization in humans. Cross-reactive pAbs originating from memory B cells immediately bound the stem of HA and persisted for over a year post vaccination. -

Proteome-Wide Epitope Mapping Identifies a Resource of Antibodies
Signal Transduction and Targeted Therapy www.nature.com/sigtrans LETTER OPEN Proteome-wide epitope mapping identifies a resource of antibodies for SARS-CoV-2 detection and neutralization Signal Transduction and Targeted Therapy (2021) 6:166; https://doi.org/10.1038/s41392-021-00573-9 Dear Editor, The epitopes of 15 antibodies to the SARS-CoV-2 ORF1ab, M, E, Since December 2019, the coronavirus disease 2019 (COVID- ORF6, ORF7a, and ORF8 proteins were also analyzed (Supple- 19) caused by the severe acute respiratory syndrome mentary Table S2 and Fig. S2). Our analyses indicate that the coronavirus-2 (SARS-CoV-2) has become a worldwide pandemic.1 epitopes of ORF1ab antibodies are located on nsp1, nsp2, nsp3, Significant efforts have been made to generate antibodies to nsp12, and nsp13 proteins (Supplementary Fig. S2a). The epitopes help study COVID-19 pathogenesis, perform diagnostic testing, of two ORF3a antibodies (#45 and #46) are 266-EPTTTTSVPL-275, and develop treatment to neutralize SARS-CoV-2 activity. 176-TSPIS-180, respectively. Another ORF3a antibody (#47) has However, the specific sequence of amino acids recognized and two epitopes, including 246-IHTID-250 and 266-EPTTTTSVPL-275 bound by an antibody, the “epitope” is unknown for most (Supplementary Fig. S2b). Two rabbit polyclonal anti-M antibodies antibodies. In this study, we developed a high-throughput (#42, #43) bind to 186-RVAGDSGFAAYSRYR-200 and 206-LNTDH- epitope mapping platform using a peptide-based SARS-CoV-2 210, respectively (Supplementary Fig. S2c). The E protein antibody proteome microarray.2 to detect the binding epitopes of 57 (#44) has two epitopes, including 16-SVLLF-20 and 56- commercial antibodies to ORF1ab, nucleocapsid (N), spike (S), FYVYSRVKNLNSSRVPDLLV-75 (Supplementary Fig. -

SARS-Cov-2 Epitope Mapping on Microarrays Highlights Strong Immune-Response to N Protein Region
bioRxiv preprint doi: https://doi.org/10.1101/2020.11.09.374082; this version posted November 9, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. SARS-CoV-2 epitope mapping on microarrays highlights strong immune-response to N protein region Angelo Musicò§1, Roberto Frigerio§1, Alessandro Mussida1, Luisa Barzon2, Alessandro Sinigaglia2, Silvia Riccetti2, Federico Gobbi3, Chiara Piubelli3, Greta Bergamaschi1, Marcella Chiari1, Alessandro Gori#*, Marina Cretich#* 1: Consiglio Nazionale delle Ricerche, Istituto di Scienze e Tecnologie Chimiche “Giulio Natta”” (SCITEC), Via Mario Bianco 9, 20131, Milano, Italy 2: Department of Molecular Medicine, University of Padova, Via A. Gabelli 63, 35121 Padova, Italy 3: Department of Infectious-Tropical Diseases and Microbiology, IRCCS Sacro Cuore Don Calabria Hospital, Via Don A. Sempreboni, 5 – 37024 Negrar di Valpolicella (Verona), Italy §: these authors equally contributed #: these authors equally contributed *: corresponding authors [email protected] ; [email protected] Abstract A workflow for SARS-CoV-2 epitope discovery on peptide microarrays is herein reported. The process started with a proteome-wide screening of immunoreactivity based on the use of a high-density microarray followed by a refinement and validation phase on a restricted panel of probes using microarrays with tailored peptide immobilization through a click-based strategy. Progressively larger, independent cohorts of Covid-19 positive sera were tested in the refinement processes, leading to the identification of immunodominant regions on SARS-CoV-2 Spike (S), Nucleocapsid (N) protein and Orf1ab polyprotein. A summary study testing 50 serum samples highlighted an epitope of the N protein (region 155-171) providing 92% sensitivity and 100% specificity of IgG detection in Covid-19 samples thus being a promising candidate for rapid implementation in serological tests. -

Structure of a Protective Epitope of Group B Streptococcus Type III Capsular Polysaccharide
Structure of a protective epitope of group B Streptococcus type III capsular polysaccharide Filippo Carbonia, Roberto Adamoa,1, Monica Fabbrinia, Riccardo De Riccoa, Vittorio Cattaneoa, Barbara Brogionia, Daniele Veggia, Vittoria Pintoa, Irene Passalacquaa, Davide Oldrinia, Rino Rappuolia,2, Enrico Malitoa, Immaculada y Ros Margarita,1, and Francesco Bertia,1,2 aGSK Vaccines, 53100 Siena, Italy Contributed by Rino Rappuoli, March 27, 2017 (sent for review February 3, 2017; reviewed by Dennis L. Kasper and Robert J. Woods) Despite substantial progress in the prevention of group B Strepto- GBS is an encapsulated Gram-positive β-hemolytic pathogen coccus (GBS) disease with the introduction of intrapartum antibiotic causing neonatal sepsis and meningitis, particularly in infants born prophylaxis, this pathogen remains a leading cause of neonatal to mothers carrying the bacteria (12). The GBS capsular PS is infection. Capsular polysaccharide conjugate vaccines have been constituted by multiple RUs (from ∼50 up to 300 per polymer) of tested in phase I/II clinical studies, showing promise for further de- four to seven monosaccharides shaped to form a backbone and one velopment. Mapping of epitopes recognized by protective anti- or two side chains. Ten serotypes presenting a unique pattern of bodies is crucial for understanding the mechanism of action of glycosidic linkages have been identified and their primary struc- vaccines and for enabling antigen design. In this study, we report β the structure of the epitope recognized by a monoclonal antibody tures elucidated (13). Three monosaccharides ( -D-glucopyranose, β β β β with opsonophagocytic activity and representative of the protective -D-Glc; -D-galactopyranose, -D-Gal; and -D-N-acetylglucosamine, response against type III GBS polysaccharide. -

Mapping the Protein Surface of Human Immunodeficiency Virus Type 1 Gp120 Using Human Monoclonal Antibodies from Phage Display Libraries
J. Mol. Biol. (1997) 267, 684±695 Mapping the Protein Surface of Human Immunodeficiency Virus Type 1 gp120 using Human Monoclonal Antibodies from Phage Display Libraries HenrikJ.Ditzel1,3,PaulW.H.I.Parren1,JamesM.Binley1,4 JosephSodroski5,JohnP.Moore4,CarlosF.BarbasIII2 andDennisR.Burton1,2* 1Departments of Immunology Panels of hybridoma-derived monoclonal antibodies against diverse epi- and 2Molecular Biology topes are widely used in de®ning protein surface topography, particu- The Scripps Research Institute larly in the absence of crystal or NMR structural information. Here we La Jolla, CA, 92037, USA show that recombinant monoclonal antibodies from phage display libraries provide a rapid alternative for surface epitope mapping. Diverse 3Department of Medical epitopes are accessed by presenting antigen to the library in different Microbiology, Odense forms, such as sequential masking of epitopes with existing antibodies or University Medical School ligands prior to selection and selection on peptides. The approach is illus- Odense, and Department of trated for a recombinant form of the human immunode®ciency virus Clinical Immunology type 1 (HIV-1) surface glycoprotein gp120 which has been extensively Copenhagen University mapped by rodent and human monoclonal antibodies derived by cellular Hospital, Rigshospitalet methods. Human recombinant Fab fragments to most of the principal Copenhagen, Denmark epitopes on gp120 are selected including Fabs to the C1 region, a C1/C5 4Aaron Diamond AIDS epitope, a C1/C2 epitope, the V2 loop, the V3 loop and the CD4 binding Research Center, New York domain. In addition an epitope linked to residues in the V2 loop and University School of Medicine CD4 binding domain is identi®ed. -

Investigation Strategy for Rh D Typing Discrepancies Using a Combination
Investigation strategy for RhD typing discrepancies using a combination of PCR-SSP and serological techniques ABSTRACT BACKGROUND: Reactivity of different anti-D reagents and different methods for detecting RhD antigen has led to discrepancies between historical and current RhD typing. Typing problems can be resolved by a combination of serological testing and molecular techniques. STUDY DESIGN: Fifty samples with discrepant routine RhD typing were selected. Samples were tested with seven FDA-licensed Anti-D reagents and a commercial panel of monoclonal anti-D. An Rh phenotype (C, c, E, e) was performed to provide presumptive clues to the questionable D type. Samples were further investigated using the BAGene PCR-SSP kits. Results obtained were compared to the serological results. RESULTS: Twenty-six samples had positive immediate spin (IS) results with at least one of the seven routine anti-D reagents. Four samples failed to react at IAT (indirect antiglobulin test) with at least three reagents, 2 failed to react with two of the reagents. The monoclonal anti-D panel categorized 36 samples. Of these, 27 had serologic results correlated with molecular typing. Eleven samples were identified and categorized by PCR-SSP only. Serological and molecular typing failed to characterize 3 samples. CONCLUSION: Based on these findings, a testing algorithm is proposed that can be used to resolve many discrepant or doubtful RhD serologic typings. 1 INTRODUCTION The Rh blood group system is one of the most complex blood group systems. The D antigen resides on a 416 amino acid moiety consisting of over 30 different epitopes. The D antigen is present on red cells of 85% of white people and is more frequent in African and Asian populations.1 Exposure to RhD in a D-negative individual often results in the production of anti-D.