Epitope Profiling Reveals Binding Signatures of SARS-Cov-2 Immune Response and Cross- Reactivity with Endemic Hcovs
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

"Epitope Mapping: B-Cell Epitopes". In: Encyclopedia of Life Sciences
Epitope Mapping: B-cell Advanced article Epitopes Article Contents . Introduction GE Morris, Wolfson Centre for Inherited Neuromuscular Disease RJAH Orthopaedic Hospital, . What Is a B-cell Epitope? . Epitope Mapping Methods Oswestry, UK and Keele University, Keele, Staffordshire, UK . Applications Immunoglobulin molecules are folded to present a surface structure complementary to doi: 10.1002/9780470015902.a0002624.pub2 a surface feature on the antigen – the epitope is this feature of the antigen. Epitope mapping is the process of locating the antibody-binding site on the antigen, although the term is also applied more broadly to receptor–ligand interactions unrelated to the immune system. Introduction formed of highly convoluted peptide chains, so that resi- dues that lie close together on the protein surface are often Immunoglobulin molecules are folded in a way that as- far apart in the amino acid sequence (Barlow et al., 1986). sembles sequences from the variable regions of both the Consequently, most epitopes on native, globular proteins heavy and light chains into a surface feature (comprised of are conformation-dependent and they disappear if the up to six complementarity-determining regions (CDRs)) protein is denatured or fragmented. Sometimes, by acci- that is complementary in shape to a surface structure on the dent or design, antibodies are produced against linear antigen. These two surface features, the ‘paratope’ on the (sequential) epitopes that survive denaturation, though antibody and the ‘epitope’ on the antigen, may have a cer- such antibodies usually fail to recognize the native protein. tain amount of flexibility to allow an ‘induced fit’ between The simplest way to find out whether an epitope is confor- them. -

Ige – the Main Player of Food Allergy
DDMOD-431; No of Pages 8 Vol. xxx, No. xx 2016 Drug Discovery Today: Disease Models Editors-in-Chief Jan Tornell – AstraZeneca, Sweden DRUG DISCOVERY Andrew McCulloch – University of California, SanDiego, USA TODAY DISEASE MODELS IgE – the main player of food allergy 1 2,3 2 Henrike C.H. Broekman , Thomas Eiwegger , Julia Upton , 4, Katrine L. Bøgh * 1 Department of Dermatology/Allergology, University Medical Centre Utrecht (UMCU), Utrecht, The Netherlands 2 Division of Immunology and Allergy, Food Allergy and Anaphylaxis Program, The Department of Paediatrics, Hospital for Sick Children, Toronto, Canada 3 Research Institute, Physiology and Experimental Medicine, The University of Toronto, Toronto, Canada 4 National Food Institute, Technical University of Denmark, Søborg, Denmark Food allergy is a growing problem worldwide, presently Section editor: affecting 2–4% of adults and 5–8% of young children. IgE Michelle Epstein – Medical University of Vienna, is a key player in food allergy. Consequently huge Department of Dermatology, DIAID, Experimental Allergy, Waehringer Guertel 18-20, Room 4P9.02, A1090, efforts have been made to develop tests to detect Vienna, Austria. either the presence of IgE molecules, their allergen binding sites or their functionality, in order to provide allergen ingestion [1], and involve one or more of the follow- information regarding the patient’s food allergy. The ing systems; the skin (pruritus, urticaria, or angioedema), the ultimate goal is to develop tools that are capable of gastro-intestinal tract (diarrhea, vomiting, contractions, in- creased bowel movement), the respiratory tract (asthma at- discriminating between asymptomatic sensitization tack, hoarseness, stridor/laryngeal angioedema) or the and a clinically relevant food allergy, and between cardiovascular system (dizziness, drop in blood pressure, loss different allergic phenotypes in an accurate and trust- of consciousness) [2,3]. -
Using Peptide-Phage Display to Capture Conditional Motif-Based Interactions
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Science and Technology 1716 Using peptide-phage display to capture conditional motif-based interactions GUSTAV SUNDELL ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6214 ISBN 978-91-513-0433-5 UPPSALA urn:nbn:se:uu:diva-359434 2018 Dissertation presented at Uppsala University to be publicly examined in B42, BMC, Husargatan 3, Uppsala, Friday, 19 October 2018 at 09:15 for the degree of Doctor of Philosophy. The examination will be conducted in English. Faculty examiner: Doctor Attila Reményi (nstitute of Enzymology, Research Center for Natural Sciences, Hungarian Academy of Sciences, Budapest, Hungary). Abstract Sundell, G. 2018. Using peptide-phage display to capture conditional motif-based interactions. Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Science and Technology 1716. 87 pp. Uppsala: Acta Universitatis Upsaliensis. ISBN 978-91-513-0433-5. This thesis explores the world of conditional protein-protein interactions using combinatorial peptide-phage display and proteomic peptide-phage display (ProP-PD). Large parts of proteins in the human proteome do not fold in to well-defined structures instead they are intrinsically disordered. The disordered parts are enriched in linear binding-motifs that participate in protein-protein interaction. These motifs are 3-12 residue long stretches of proteins where post-translational modifications, like protein phosphorylation, can occur changing the binding preference of the motif. Allosteric changes in a protein or domain due to phosphorylation or binding to second messenger molecules like Ca2+ can also lead conditional interactions. Finding phosphorylation regulated motif-based interactions on a proteome-wide scale has been a challenge for the scientific community. -

Protein Epitope Mapping by Mass Spectrometry
Anal. Chem. 1994,66, 3723-3726 Protein Epitope Mapping By Mass Spectrometry Ylngmlng Zhao and Brian T. Chalt’ The Rockefeller University, 1230 York Avenue, New York, New York 10021 A mass spectrometricmethod is described for the rapid mapping antigen bound to an antibody. Alternatively, these workers of linear epitopes in proteins that are bound by monoclonal subjected the peptide to proteolytic digestion and identified antibodies. The method consists of three steps. In the first products that bound to the immobilized antibody. In both step, an antigen protein is digested by a proteolytic enzyme to cases, the peptides of interest were identified by 2Wfplasma produce an appropriate set of peptide fragments. In the second desorption mass spectrometry. step, peptide fragments containing the linear epitope are selected Matrix-assisted laser desorption mass spectrometry (MAL- and separated from the pool of peptide fragments by immu- DI-MS) is a recently developed method for measuring the noprecipitation with the monoclonal antibody. In the final molecular weights of peptides and proteins.12-14 The technique step, the immunoprecipitated peptides are identified by matrix- allows the accurate (better than O.l%), rapid (<1 min), and assisted laser desorption mass spectrometry. The method sensitive (<1 pmol) determination of the molecular weights allows the rapid determination of antigenic sites without tedious of components of complex mixtures of peptides. MALDI- peptide synthesis or protein mutagenesis. The approach is MS is finding wide use for the rapid identification of proteins demonstrated through the mapping of epitopes in two peptides and the elucidation of their primary structures (in particular, (melittin and glucagon-like peptide-1 7-37) against which the definition of posttranslational modifications.) monoclonal antibodies were raised. -
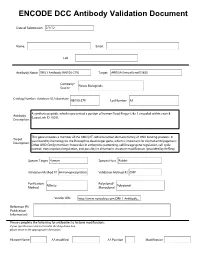
ENCODE DCC Antibody Validation Document
ENCODE DCC Antibody Validation Document Date of Submission Name: Email: Lab Antibody Name: Target: Company/ Source: Catalog Number, database ID, laboratory Lot Number Antibody Description: Target Description: Species Target Species Host Validation Method #1 Validation Method #2 Purification Polyclonal/ Method Monoclonal Vendor URL: Reference (PI/ Publication Information) Please complete the following for antibodies to histone modifications: if your specifications are not listed in the drop-down box, please write-in the appropriate information Histone Name AA modified AA Position Modification Validation #1 Analysis Insert Validation Image (click here) ARID3A (NB100-279) & (sc-8821) Immunoblot / Immunoprecipitation A. MW (kD) B. MW (kD) C. MW (kD) D. MW (kD) 150 150 150 150 100 100 100 100 75 75 75 75 50 50 50 50 38 38 38 38 25 25 25 20 20 20 25 15 15 15 15 Lane : 1 2 3 4 Lane : 1 2 3 Lane : 1 2 Lane : 1 2 3 A. Western Blot using NB100-279 on nuclear lysates from cell lines GM12878 (Lane1), K562 (Lane2), HeLaS3 (Lane3), and HepG2 (Lane4). B. Immunoprecipitation was performed on nuclear lysates from K562 cells using antibody NB100-279. Lane1: Nuclear lysate. Lane 3: Bound material from control immunoprecipitation with rabbit IgG. Lane 2: Bound material from immunoprecipitation with NB100-279. C. Western Blot using sc-8821 on nuclear lysates from cell lines GM12878 (Lane1), K562 (Lane2). D. Immunoprecipitation was performed on nuclear lysates from K562 cells using antibody sc-8821 and immunoblot with NB100-279. Lane1: Nuclear lysate. Lane 2: Bound material from immunoprecipitation with sc-8821. Lane 3: Bound material from control immunoprecipitation with Goat IgG. -
Development of a Phage Display Library for Discovery of Antigenic Brucella Peptides Jeffrey Williams Iowa State University
Iowa State University Capstones, Theses and Graduate Theses and Dissertations Dissertations 2018 Development of a phage display library for discovery of antigenic Brucella peptides Jeffrey Williams Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/etd Part of the Microbiology Commons Recommended Citation Williams, Jeffrey, "Development of a phage display library for discovery of antigenic Brucella peptides" (2018). Graduate Theses and Dissertations. 16896. https://lib.dr.iastate.edu/etd/16896 This Thesis is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Graduate Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. Development of a phage display library for discovery of antigenic Brucella peptides by Jeffrey Williams A thesis submitted to the graduate faculty in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE Major: Microbiology Program of Study Committee: Bryan H. Bellaire, Major Professor Steven Olsen Steven Carlson The student author, whose presentation of the scholarship herein was approved by the program of study committee, is solely responsible for the content of this thesis. The Graduate College will ensure this thesis is globally accessible and will not permit alterations after a degree is conferred. Iowa State University -
![Epitope Mapping of an Uncertain Endogenous Antigen Implies Secretogranin II Peptide Splicing [Version 2; Peer Review: 1 Approved, 2 Approved with Reservations]](https://docslib.b-cdn.net/cover/9315/epitope-mapping-of-an-uncertain-endogenous-antigen-implies-secretogranin-ii-peptide-splicing-version-2-peer-review-1-approved-2-approved-with-reservations-409315.webp)
Epitope Mapping of an Uncertain Endogenous Antigen Implies Secretogranin II Peptide Splicing [Version 2; Peer Review: 1 Approved, 2 Approved with Reservations]
F1000Research 2019, 8:1732 Last updated: 26 JUL 2021 RESEARCH ARTICLE Epitope mapping of an uncertain endogenous antigen implies secretogranin II peptide splicing [version 2; peer review: 1 approved, 2 approved with reservations] David R. Howlett 1, Iain J. Clarke2, Russell P. Newton3, John E. Hart4 1Wolfson Centre for Age Related Disease, Kings College London, London, SE1 1UL, UK 2School of Agriculture and Veterinary Science, Melbourne University, Parkville, Victoria, VIC 3010, Australia 3Biochemistry Group, Institute of Life Sciences, Medical School, Swansea University, Swansea, Wales, SA2 8PP, UK 4Endocrine Pharmaceuticals Ltd, Tadley, Hampshire, RG26 3TA, UK v2 First published: 09 Oct 2019, 8:1732 Open Peer Review https://doi.org/10.12688/f1000research.20633.1 Latest published: 05 Dec 2019, 8:1732 https://doi.org/10.12688/f1000research.20633.2 Reviewer Status Invited Reviewers Abstract Background: The search for a tissue-mass reducing reproductive 1 2 3 hormone involved a bioassay-guided physicochemical fractionation of sheep blood plasma. This brought forth a candidate protein whose version 2 apparent mass on gels and in mass spectrometry (MS) was 7-8 kDa, (revision) report report implying a polypeptide of ~70 residues. Four purification runs gave 05 Dec 2019 Edman N-terminal sequences relating to 1MKPLTGKVKEFNNI14. This is bioinformatically obscure and has been resistant to molecular version 1 biological investigation. The sequence was synthesized as the peptide 09 Oct 2019 report report EPL001, against which was raised a goat polyclonal antiserum, G530. Used in an antigen capture campaign, G530 pointed to the existence of a novel derivative of secretogranin II (SgII), the neuroendocrine 1. -
Highly Accurate and Reproducible Diagnosis of Peanut Allergy Using Epitope Mapping
medRxiv preprint doi: https://doi.org/10.1101/2020.06.19.20136002; this version posted June 20, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Highly Accurate and Reproducible Diagnosis of Peanut Allergy Using Epitope Mapping Paul Kearney1, Robert Getts1, Clive Hayward1, David Luta1, Alex Porter1, Marc Witmer1, George du Toit2, Gideon Lack2, R. Sharon Chinthrajah3, Stephen J Galli3,4, Kari Nadeau3, Galina Grishina5, Mayte Suárez-Fariñas5, Maria Suprun5, Hugh A Sampson5 1. AllerGenis LLC, Hatfield, PA, USA 2. King’s College London, London, UK 3. Sean N. Parker Center for Allergy and Asthma Research at Stanford University, Stanford, USA 4. Departments of Pathology and Microbiology & Immunology, Stanford University. 5. Department of Pediatrics, Allergy and Immunology, Icahn School of Medicine at Mount Sinai, New York, NY, USA Abstract Background: Misdiagnosis of peanut allergy is a significant clinical challenge. Here, a novel diagnostic blood-based test using a Bead-Based Epitope Assay (“peanut BBEA”) has been developed on the LEAP cohort and then independently validated on the CoFAR2 and POISED cohorts. Methods: Development of the peanut BBEA followed the National Academy of Medicine’s established guidelines with discovery performed on 133 subjects from the non- interventional arm of the LEAP trial and an independent validation performed on 81 subjects from the CoFAR2 study and 84 subjects from the POISED study. All subject samples were analyzed using the BBEA methodology. -

Phage Display Libraries for Antibody Therapeutic Discovery and Development
antibodies Review Phage Display Libraries for Antibody Therapeutic Discovery and Development Juan C. Almagro 1,2,* , Martha Pedraza-Escalona 3, Hugo Iván Arrieta 3 and Sonia Mayra Pérez-Tapia 3 1 GlobalBio, Inc., 320, Cambridge, MA 02138, USA 2 UDIBI, ENCB, Instituto Politécnico Nacional, Prolongación de Carpio y Plan de Ayala S/N, Colonia Casco de Santo Tomas, Delegación Miguel Hidalgo, Ciudad de Mexico 11340, Mexico 3 CONACyT-UDIBI, ENCB, Instituto Politécnico Nacional, Prolongación de Carpio y Plan de Ayala S/N, Colonia Casco de Santo Tomas, Delegación Miguel Hidalgo, Ciudad de Mexico 11340, Mexico * Correspondence: [email protected] Received: 24 June 2019; Accepted: 15 August 2019; Published: 23 August 2019 Abstract: Phage display technology has played a key role in the remarkable progress of discovering and optimizing antibodies for diverse applications, particularly antibody-based drugs. This technology was initially developed by George Smith in the mid-1980s and applied by John McCafferty and Gregory Winter to antibody engineering at the beginning of 1990s. Here, we compare nine phage display antibody libraries published in the last decade, which represent the state of the art in the discovery and development of therapeutic antibodies using phage display. We first discuss the quality of the libraries and the diverse types of antibody repertoires used as substrates to build the libraries, i.e., naïve, synthetic, and semisynthetic. Second, we review the performance of the libraries in terms of the number of positive clones per panning, hit rate, affinity, and developability of the selected antibodies. Finally, we highlight current opportunities and challenges pertaining to phage display platforms and related display technologies. -

Revealing Protein Structures: a New Method for Mapping Antibody Epitopes
Revealing protein structures: A new method for mapping antibody epitopes Brendan M. Mumey Brian W. Bailey Edward A. Dratz Department of Computer NIH/NlAAA/DlCBWLMBB Department of Chemistry and Science Fluorescence Studies Biochemistry Montana State University Park 5 Building Montana State University Bozeman, MT 59717-3880 12420 Parklawn Dr. MSC Bozeman, MT 59717-3400 [email protected] 8115 [email protected] Bethesda, MD 20892-8115 [email protected] ABSTRACT cells [9] and each protein has a unique folded structure. Whenever A recent idea for determining the three-dimensional structure of a the 3-D folding structure of linear protein sequences can be de- protein uses antibody recognition of surface structure and random termined this information has provided fundamental insights into peptide libraries to map antibody epitope combining sites. Anti- mechanisms of action that are often extremely useful in drug de- bodies that bind to the surface of the protein of interest can be sign. Traditional methods of protein structure determination re- used as “witnesses” to report the structure of the protein as follows: quire preparation of large amounts of protein in functional form, Proteins are composed of linear polypeptide chains that come to- which often may not be feasible. Attempts are then made to grow gether in complex spatial folding patterns to create the native pro- 3-D crystals of the proteins of interest for structure determination tein structures and these folded structures form the binding sites by x-ray diffraction, however, obtaining crystals of sufficient qual- for the antibodies. Short amino acid probe sequences, which bind ity is still an art and may not be possible [24, 251. -

Monitoramento Em Biotecnologia Desenvolvimento Científico E Tecnológico
Centro de Gestão e Estudos Estratégicos Ciência, Tecnologia e Inovação Monitoramento em Biotecnologia Desenvolvimento científico e tecnológico 3° Relatório Volume II - Patentes e Países Depositantes Coordenação Adelaide Antunes Rio de Janeiro Março, 2005 MONITORAMENTO EM BIOTECNOLOGIA Desenvolvimento científico e tecnológico 3° Relatório Volume II Patentes e Países Depositantes Executor: Sistema de Informação sobre a Indústria Química (SIQUIM) Escola de Química (EQ) Universidade Federal do Rio de Janeiro (UFRJ) Março / 2005 2 A Biotecnologia tem sido destacada como tecnologia portadora do futuro e consequentemente, com alto componente de desenvolvimento econômico e social, em vários países, principalmente nos últimos anos. O estudo "Monitoramento em Biotecnologia" encomendado pelo CGEE ao SIQUIM/EQ/UFRJ, permite visualizar a dinâmica de P,D&I desta área, a diversidade de atores envolvidos e o forte escopo de atuação em desenvolvimentos que impactam fortemente "Saúde e Qualidade de vida", bem como a "Agricultura e Meio ambiente", por meio de desenvolvimento acelerado de publicações científicas e de patentes nos Temas e/ou Termos tratados neste estudo. Reforça-se, então, que este estudo representa um instrumento importante de apoio à decisão aos stakeholders atuantes na área, pois permite priorizar ações concernentes ao desenvolvimento e estímulo ao uso sustentável da biodiversidade, à segurança biológica e à produção de bioprodutos, biodrogas, transgênicos. Monitoramento em Biotecnologia SIQUIM/EQ/UFRJ e CGEE 3 EQUIPE: Coordenação Geral: -

Phage Display
Chem. Rev. 1997, 97, 391−410 391 Phage Display George P. Smith* and Valery A. Petrenko Division of Biological Sciences, University of Missouri, Columbia, Missouri 65211 Received January 2, 1997 (Revised Manuscript Received January 23, 1997) Contents more, and that in a degree which exceeds all computation.”1 I. In Vitro Evolution of Chemicals 391 II. Phage-Display Libraries as Populations of 392 Replicable, Mutable Chemicals But ever since Darwin we have come to understand that the exquisite “watches” of the living world are A. Phage-Display Vectors 392 fashioned by an altogether different process. As B. How Foreign Peptides Are Displayed on 393 Richard Dawkins writes in his compelling book on Filamentous Phages evolution, natural selection “does not plan for the C. Types of Phage-Display Systems 394 future. It has no vision, no foresight, no sight at all. III. Types of Displayed Peptides and Proteins 394 If it can be said to play the role of watchmaker in IV. Selection 397 nature, it is the blind watchmaker.”2 A. General Principles 397 Imagine, then, the applied chemist, not as designer B. Affinity Selection 397 of molecules with a particular purpose, but rather C. Selection for Traits Other than Affinity 399 as custodian of a highly diverse population of chemi- D. Enrichment of Specific Sequence Motifs 399 cals evolving in vitro as if they were organisms V. Exploring the Fitness Landscape 400 subject to natural selection. A chemical’s “fitness” A. Sequence Space, Fitness Landscapes, and 400 in this artificial biosphere would be imposed by the Sparse Libraries custodian for his or her own ends.