Ige – the Main Player of Food Allergy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evaluation of T-Cell and B-Cell Epitopes and Design of Multivalent Vaccines Against Htlv-1 Diseases
EVALUATION OF T-CELL AND B-CELL EPITOPES AND DESIGN OF MULTIVALENT VACCINES AGAINST HTLV-1 DISEASES DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Roshni Sundaram, M.S. * * * * * The Ohio State University 2003 Dissertation Committee: Approved by Professor Pravin T.P. Kaumaya, Adviser Professor Christopher M. Walker Adviser Professor Neil R. Baker Department of Microbiology Professor Marshall V. Williams ABSTRACT Human T-cell lymphotropic virus type I (HTLV-1) is a C type retrovirus that is the causative agent of an aggressive T-cell malignancy, adult T-cell leukemia/lymphoma (ATLL). The virus is also implicated in a number of inflammatory disorders, the most prominent among them being HTLV-1 associated myelopathy or tropical spastic paraparesis (HAM/TSP). HTLV-1, like many viruses that cause chronic infection, has adapted to persist in the face of an active immune response in infected individuals. The viral transactivator Tax is the primary target of the cellular immune response and humoral responses are mainly directed against the envelope protein. Vaccination against HTLV-1 is a feasible option as there is very little genetic and antigenic variability. Vaccination regimes against chronic viruses must be aimed at augmenting the immune response to a level that is sufficient to clear the virus. This requires that the vaccine delivers a potent stimulus to the immune system that closely resembles natural infection to activate both the humoral arm and the cellular arm. It is also clear that multicomponent vaccines may be more beneficial in terms of increasing the breadth of the immune response as well as being applicable in an outbred population. -

"Epitope Mapping: B-Cell Epitopes". In: Encyclopedia of Life Sciences
Epitope Mapping: B-cell Advanced article Epitopes Article Contents . Introduction GE Morris, Wolfson Centre for Inherited Neuromuscular Disease RJAH Orthopaedic Hospital, . What Is a B-cell Epitope? . Epitope Mapping Methods Oswestry, UK and Keele University, Keele, Staffordshire, UK . Applications Immunoglobulin molecules are folded to present a surface structure complementary to doi: 10.1002/9780470015902.a0002624.pub2 a surface feature on the antigen – the epitope is this feature of the antigen. Epitope mapping is the process of locating the antibody-binding site on the antigen, although the term is also applied more broadly to receptor–ligand interactions unrelated to the immune system. Introduction formed of highly convoluted peptide chains, so that resi- dues that lie close together on the protein surface are often Immunoglobulin molecules are folded in a way that as- far apart in the amino acid sequence (Barlow et al., 1986). sembles sequences from the variable regions of both the Consequently, most epitopes on native, globular proteins heavy and light chains into a surface feature (comprised of are conformation-dependent and they disappear if the up to six complementarity-determining regions (CDRs)) protein is denatured or fragmented. Sometimes, by acci- that is complementary in shape to a surface structure on the dent or design, antibodies are produced against linear antigen. These two surface features, the ‘paratope’ on the (sequential) epitopes that survive denaturation, though antibody and the ‘epitope’ on the antigen, may have a cer- such antibodies usually fail to recognize the native protein. tain amount of flexibility to allow an ‘induced fit’ between The simplest way to find out whether an epitope is confor- them. -

Mapping B-Cell Epitopes for Nonspecific Lipid Transfer Proteins of Legumes Consumed in India and Identification of Critical Resi
foods Article Mapping B-Cell Epitopes for Nonspecific Lipid Transfer Proteins of Legumes Consumed in India and Identification of Critical Residues Responsible for IgE Binding Ankita Mishra 1,* and Ashok Kumar 1,2,3,4 1 Department of Biological Sciences and Bioengineering, Indian Institute of Technology Kanpur, Kanpur 208016, UP, India; [email protected] 2 Centre for Environmental Science and Engineering, Indian Institute of Technology Kanpur, Kanpur 208016, UP, India 3 Centre for Nanosciences, Indian Institute of Technology Kanpur, Kanpur 208016, UP, India 4 The Mehta Family Centre for Engineering in Medicine, Indian Institute of Technology Kanpur, Kanpur 208016, UP, India * Correspondence: [email protected] Abstract: Nonspecific lipid transfer proteins (nsLTPs) have been categorized as panallergens and display widespread occurrence across plant-kingdom. Present study, investigated B-cell epitopes for LTPs from chickpea, mung-bean, cowpea, pigeon-pea, and soybean via in silico methods. In-silico predicted regions were evaluated for epitope-conservancy and property-based peptide similarity search by different allergen databases. Additionally, the in-silico predicted regions were compared Citation: Mishra, A.; Kumar, A. with the experimentally validated epitopes of peach-LTP. Sequence-homology studies showed that Mapping B-Cell Epitopes for chickpea and mung-bean LTPs shared significant homology, i.e., >70% and >60%, respectively, with Nonspecific Lipid Transfer Proteins of other LTP allergens from lentil, garden-pea, peanut, etc. Phylogenetic-analysis also showed chickpea Legumes Consumed in India and and mung-bean LTPs to be closely related to allergenic LTPs from lentil and peanut, respectively. Identification of Critical Residues Responsible for IgE Binding. Foods Epitope-conservation analysis showed that two of the predicted B-cell epitopic regions in chickpea 2021, 10, 1269. -

Opportunities for Conformation-Selective Antibodies in Amyloid-Related Diseases
Antibodies 2015, 4, 170-196; doi:10.3390/antib4030170 OPEN ACCESS antibodies ISSN 2073-4468 www.mdpi.com/journal/antibodies Review Opportunities for Conformation-Selective Antibodies in Amyloid-Related Diseases Marta Westwood * and Alastair D. G. Lawson Structural Biology, UCB, 216 Bath Road, Slough, SL1 3WE UK; E-Mail: [email protected]. * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +44-1-753-534-655 (ext.7749); Fax: +44-1-753-536-632. Academic Editor: Dimiter S. Dimitrov Received: 13 May 2015 / Accepted: 9 July 2015 / Published: 15 July 2015 Abstract: Assembly of misfolded proteins into fibrillar deposits is a common feature of many neurodegenerative diseases. Developing effective therapies to these complex, and not yet fully understood diseases is currently one of the greatest medical challenges facing society. Slow and initially asymptomatic onset of neurodegenerative disorders requires profound understanding of the processes occurring at early stages of the disease including identification and structural characterisation of initial toxic species underlying neurodegeneration. In this review, we chart the latest progress made towards understanding the multifactorial process leading to amyloid formation and highlight efforts made in the development of therapeutic antibodies for the treatment of amyloid-based disorders. The specificity and selectivity of conformational antibodies make them attractive research probes to differentiate between transient states preceding formation of mature fibrils and enable strategies for potential therapeutic intervention to be considered. Keywords: antibody; amyloids; conformation; prion; Alzheimer’s; Parkinson’s; fibrils, tau; Huntingtin; protein misfolding 1. Introduction Correct protein folding is crucial for maintaining healthy biological functions. -

Inhibition of Allergic Reactivity Through Targeting Fcεri-Bound Ige with Humanized Low-Affinity Antibodies
Inhibition of Allergic Reactivity through Targeting Fc εRI-Bound IgE with Humanized Low-Affinity Antibodies This information is current as Ke Zhang, Michael Elias, Hong Zhang, Jeffrey Liu, of September 27, 2021. Christopher Kepley, Yun Bai, Dean D. Metcalfe, Zachary Schiller, Yang Wang and Andrew Saxon J Immunol published online 21 October 2019 http://www.jimmunol.org/content/early/2019/10/19/jimmun ol.1900112 Downloaded from Why The JI? Submit online. http://www.jimmunol.org/ • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average by guest on September 27, 2021 Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2019 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Published October 21, 2019, doi:10.4049/jimmunol.1900112 The Journal of Immunology Inhibition of Allergic Reactivity through Targeting Fc«RI-Bound IgE with Humanized Low-Affinity Antibodies Ke Zhang,* Michael Elias,† Hong Zhang,* Jeffrey Liu,* Christopher Kepley,† Yun Bai,‡ Dean D. Metcalfe,‡ Zachary Schiller,x Yang Wang,x and Andrew Saxon* Options for effective prevention and treatment of epidemic allergic diseases remain limited, and particularly so for IgE-mediated 26 28 food allergies. -

Characterization of Conformational B-Cell
PEPTIDE-BASED B-CELL EPITOPE VACCINES TARGETING HER-2/NEU DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy in the Graduate School of The Ohio State University By Joan T. Garrett, B.S./B.A. ***** The Ohio State University 2007 Dissertation Committee: Approved by Professor Pravin Kaumaya, Advisor ___________________________ Advisor Professor Dehua Pei, Advisor Professor Ross Dalbey ___________________________ Advisor Professor Thomas Magliery Graduate Program in Chemistry ABSTRACT HER-2/neu (ErbB2), a member of the epidermal growth factor family of receptors (EGFR) is overexpressed in a significant fraction of breast cancers. It is an attractive target for receptor-directed antitumor therapy using monoclonal antibodies. Trastuzumab and pertuzumab are growth-inhibitory humanized antibodies targeting the oncogenic protein HER-2/neu. Although passive immunotherapy with trastuzumab is approved for treatment of breast cancer, a number of concerns exist with passive immunotherapy. Treatment is expensive, and has a limited duration of action, necessitating repeated administrations of the monoclonal antibody. Active immunotherapy with conformational B-cell epitopes affords the possibility of generating an enduring immune response, eliciting protein-reactive high-affinity anti-peptide antibodies. The three-dimensional structure of human HER-2 in complex with trastuzumab reveals that the antigen binding region of HER-2 spans residues 563-626 that comprises an extensive disulfide bonding pattern. In order to minimally dissect the interacting binding region of HER-2, we have designed four synthetic peptides with different levels of conformational flexibility. Chimeric peptides incorporating the measles virus fusion ‘promiscuous’ T cell epitope via a four-residue linker sequence were synthesized, purified, and characterized. -

Protein Epitope Mapping by Mass Spectrometry
Anal. Chem. 1994,66, 3723-3726 Protein Epitope Mapping By Mass Spectrometry Ylngmlng Zhao and Brian T. Chalt’ The Rockefeller University, 1230 York Avenue, New York, New York 10021 A mass spectrometricmethod is described for the rapid mapping antigen bound to an antibody. Alternatively, these workers of linear epitopes in proteins that are bound by monoclonal subjected the peptide to proteolytic digestion and identified antibodies. The method consists of three steps. In the first products that bound to the immobilized antibody. In both step, an antigen protein is digested by a proteolytic enzyme to cases, the peptides of interest were identified by 2Wfplasma produce an appropriate set of peptide fragments. In the second desorption mass spectrometry. step, peptide fragments containing the linear epitope are selected Matrix-assisted laser desorption mass spectrometry (MAL- and separated from the pool of peptide fragments by immu- DI-MS) is a recently developed method for measuring the noprecipitation with the monoclonal antibody. In the final molecular weights of peptides and proteins.12-14 The technique step, the immunoprecipitated peptides are identified by matrix- allows the accurate (better than O.l%), rapid (<1 min), and assisted laser desorption mass spectrometry. The method sensitive (<1 pmol) determination of the molecular weights allows the rapid determination of antigenic sites without tedious of components of complex mixtures of peptides. MALDI- peptide synthesis or protein mutagenesis. The approach is MS is finding wide use for the rapid identification of proteins demonstrated through the mapping of epitopes in two peptides and the elucidation of their primary structures (in particular, (melittin and glucagon-like peptide-1 7-37) against which the definition of posttranslational modifications.) monoclonal antibodies were raised. -
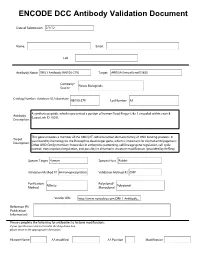
ENCODE DCC Antibody Validation Document
ENCODE DCC Antibody Validation Document Date of Submission Name: Email: Lab Antibody Name: Target: Company/ Source: Catalog Number, database ID, laboratory Lot Number Antibody Description: Target Description: Species Target Species Host Validation Method #1 Validation Method #2 Purification Polyclonal/ Method Monoclonal Vendor URL: Reference (PI/ Publication Information) Please complete the following for antibodies to histone modifications: if your specifications are not listed in the drop-down box, please write-in the appropriate information Histone Name AA modified AA Position Modification Validation #1 Analysis Insert Validation Image (click here) ARID3A (NB100-279) & (sc-8821) Immunoblot / Immunoprecipitation A. MW (kD) B. MW (kD) C. MW (kD) D. MW (kD) 150 150 150 150 100 100 100 100 75 75 75 75 50 50 50 50 38 38 38 38 25 25 25 20 20 20 25 15 15 15 15 Lane : 1 2 3 4 Lane : 1 2 3 Lane : 1 2 Lane : 1 2 3 A. Western Blot using NB100-279 on nuclear lysates from cell lines GM12878 (Lane1), K562 (Lane2), HeLaS3 (Lane3), and HepG2 (Lane4). B. Immunoprecipitation was performed on nuclear lysates from K562 cells using antibody NB100-279. Lane1: Nuclear lysate. Lane 3: Bound material from control immunoprecipitation with rabbit IgG. Lane 2: Bound material from immunoprecipitation with NB100-279. C. Western Blot using sc-8821 on nuclear lysates from cell lines GM12878 (Lane1), K562 (Lane2). D. Immunoprecipitation was performed on nuclear lysates from K562 cells using antibody sc-8821 and immunoblot with NB100-279. Lane1: Nuclear lysate. Lane 2: Bound material from immunoprecipitation with sc-8821. Lane 3: Bound material from control immunoprecipitation with Goat IgG. -
![Epitope Mapping of an Uncertain Endogenous Antigen Implies Secretogranin II Peptide Splicing [Version 2; Peer Review: 1 Approved, 2 Approved with Reservations]](https://docslib.b-cdn.net/cover/9315/epitope-mapping-of-an-uncertain-endogenous-antigen-implies-secretogranin-ii-peptide-splicing-version-2-peer-review-1-approved-2-approved-with-reservations-409315.webp)
Epitope Mapping of an Uncertain Endogenous Antigen Implies Secretogranin II Peptide Splicing [Version 2; Peer Review: 1 Approved, 2 Approved with Reservations]
F1000Research 2019, 8:1732 Last updated: 26 JUL 2021 RESEARCH ARTICLE Epitope mapping of an uncertain endogenous antigen implies secretogranin II peptide splicing [version 2; peer review: 1 approved, 2 approved with reservations] David R. Howlett 1, Iain J. Clarke2, Russell P. Newton3, John E. Hart4 1Wolfson Centre for Age Related Disease, Kings College London, London, SE1 1UL, UK 2School of Agriculture and Veterinary Science, Melbourne University, Parkville, Victoria, VIC 3010, Australia 3Biochemistry Group, Institute of Life Sciences, Medical School, Swansea University, Swansea, Wales, SA2 8PP, UK 4Endocrine Pharmaceuticals Ltd, Tadley, Hampshire, RG26 3TA, UK v2 First published: 09 Oct 2019, 8:1732 Open Peer Review https://doi.org/10.12688/f1000research.20633.1 Latest published: 05 Dec 2019, 8:1732 https://doi.org/10.12688/f1000research.20633.2 Reviewer Status Invited Reviewers Abstract Background: The search for a tissue-mass reducing reproductive 1 2 3 hormone involved a bioassay-guided physicochemical fractionation of sheep blood plasma. This brought forth a candidate protein whose version 2 apparent mass on gels and in mass spectrometry (MS) was 7-8 kDa, (revision) report report implying a polypeptide of ~70 residues. Four purification runs gave 05 Dec 2019 Edman N-terminal sequences relating to 1MKPLTGKVKEFNNI14. This is bioinformatically obscure and has been resistant to molecular version 1 biological investigation. The sequence was synthesized as the peptide 09 Oct 2019 report report EPL001, against which was raised a goat polyclonal antiserum, G530. Used in an antigen capture campaign, G530 pointed to the existence of a novel derivative of secretogranin II (SgII), the neuroendocrine 1. -
Highly Accurate and Reproducible Diagnosis of Peanut Allergy Using Epitope Mapping
medRxiv preprint doi: https://doi.org/10.1101/2020.06.19.20136002; this version posted June 20, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Highly Accurate and Reproducible Diagnosis of Peanut Allergy Using Epitope Mapping Paul Kearney1, Robert Getts1, Clive Hayward1, David Luta1, Alex Porter1, Marc Witmer1, George du Toit2, Gideon Lack2, R. Sharon Chinthrajah3, Stephen J Galli3,4, Kari Nadeau3, Galina Grishina5, Mayte Suárez-Fariñas5, Maria Suprun5, Hugh A Sampson5 1. AllerGenis LLC, Hatfield, PA, USA 2. King’s College London, London, UK 3. Sean N. Parker Center for Allergy and Asthma Research at Stanford University, Stanford, USA 4. Departments of Pathology and Microbiology & Immunology, Stanford University. 5. Department of Pediatrics, Allergy and Immunology, Icahn School of Medicine at Mount Sinai, New York, NY, USA Abstract Background: Misdiagnosis of peanut allergy is a significant clinical challenge. Here, a novel diagnostic blood-based test using a Bead-Based Epitope Assay (“peanut BBEA”) has been developed on the LEAP cohort and then independently validated on the CoFAR2 and POISED cohorts. Methods: Development of the peanut BBEA followed the National Academy of Medicine’s established guidelines with discovery performed on 133 subjects from the non- interventional arm of the LEAP trial and an independent validation performed on 81 subjects from the CoFAR2 study and 84 subjects from the POISED study. All subject samples were analyzed using the BBEA methodology. -
Role of Serologic Testing in Rheumatic Diseases
Role of Serologic Testing in Rheumatic Diseases Debendra Pattanaik MD FACP Associate professor of Medicine UTHSC, Memphis TN Disclosure None Objectives Discuss commonly available serologic testing useful in daily clinical practice Recognize the serologic associations of rheumatic diseases Recognize their diagnostic utilities and limitations Diagnostic Accuracy for Lupus and other autoimmune diseases in the community setting 476 patients were evaluated at Autoimmunity Center of University of Florida, Gainesville for 13 months which were by from primary care physicians SLE was over diagnosed on many patients on the basis of + ANA 39 patients are taking prednisone 60 mg/day who have no autoimmune disease but only have + ANA Inappropriate diagnosis leads to inappropriate therapy, emotional and financial consequences The authors suggested continuing education in screening for autoimmune disease and identify patients who may benefit from early referral. Arch Intern Med. 2004;164:2435-2441 Antinuclear Antibody (ANA) Testing for Connective Tissue Disease British Columbia Population: 4.631 million. More than 94,000 ANA tests were performed in B.C. in fiscal year 2011/12 at a cost of $2.24 million annually. Incidence and Estimated New Cases in B.C. for Selected CTDs Connective Tissue Disease Disease incidence per million population Estimated new BC cases/year * Systemic lupus erythematosus 56 259 Scleroderma 19 88 Dermatomyositis & polymyositis < 10 < 46 Eighteen percent of first-time tested outpatients underwent unnecessary repeat testing in 2010/2011. In 57.2% of the repeat testing, both the initial and the repeat ANA tests were ordered by a GP. In 24.8% the initial test was ordered by a GP and the repeat test was ordered by a specialist, and in 10.2% both the initial and the repeat test were ordered by the same specialist. -

Welcoming Guests with Food Allergies
Welcoming Guests With Food Allergies A comprehensive program for training staff to safely prepare and serve food to guests who have food allergies The Food Allergy & Anaphylaxis Network 11781 Lee Jackson Hwy., Suite 160 Fairfax, VA 22033 (800) 929-4040 www.foodallergy.org Produced and distributed by the Food Allergy & Anaphylaxis Network (FAAN). FAAN is a nonprofit organization established to raise public awareness, to provide advocacy and education, and to advance research on behalf of all those affected by food allergies and anaphylaxis. All donations are tax-deductible. © 2001. Updated 2010, the Food Allergy & Anaphylaxis Network. All Rights Reserved. ISBN 1-882541-21-9 FAAN grants permission to photocopy this document for limited internal use. This consent does not extend to other kinds of copying, such as copying for general distribution (excluding the materials in the Appendix, which may be customized, reproduced, and distributed for and by the establishment), for advertising or promotional purposes, for creating new collective works, or for resale. For information, contact FAAN, 11781 Lee Jackson Hwy., Suite 160, Fairfax, VA 22033, www.foodallergy.org. Disclaimer This guide was designed to provide a guideline for restaurant and food service employees. FAAN and its collaborators disclaim any responsibility for any adverse effects resulting from the information presented in this guide. FAAN does not warrant or guarantee that following the procedures outlined in this guide will eliminate or prevent allergic reactions. The food service facility should not rely on the information contained herein as its sole source of information to prevent allergic reactions. The food service facility should make sure that it complies with all local, state, and federal requirements relating to the safe handling of food and other consumable items, in addition to following safe food-handling procedures to prevent food contamination.