Role of Serologic Testing in Rheumatic Diseases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ige – the Main Player of Food Allergy
DDMOD-431; No of Pages 8 Vol. xxx, No. xx 2016 Drug Discovery Today: Disease Models Editors-in-Chief Jan Tornell – AstraZeneca, Sweden DRUG DISCOVERY Andrew McCulloch – University of California, SanDiego, USA TODAY DISEASE MODELS IgE – the main player of food allergy 1 2,3 2 Henrike C.H. Broekman , Thomas Eiwegger , Julia Upton , 4, Katrine L. Bøgh * 1 Department of Dermatology/Allergology, University Medical Centre Utrecht (UMCU), Utrecht, The Netherlands 2 Division of Immunology and Allergy, Food Allergy and Anaphylaxis Program, The Department of Paediatrics, Hospital for Sick Children, Toronto, Canada 3 Research Institute, Physiology and Experimental Medicine, The University of Toronto, Toronto, Canada 4 National Food Institute, Technical University of Denmark, Søborg, Denmark Food allergy is a growing problem worldwide, presently Section editor: affecting 2–4% of adults and 5–8% of young children. IgE Michelle Epstein – Medical University of Vienna, is a key player in food allergy. Consequently huge Department of Dermatology, DIAID, Experimental Allergy, Waehringer Guertel 18-20, Room 4P9.02, A1090, efforts have been made to develop tests to detect Vienna, Austria. either the presence of IgE molecules, their allergen binding sites or their functionality, in order to provide allergen ingestion [1], and involve one or more of the follow- information regarding the patient’s food allergy. The ing systems; the skin (pruritus, urticaria, or angioedema), the ultimate goal is to develop tools that are capable of gastro-intestinal tract (diarrhea, vomiting, contractions, in- creased bowel movement), the respiratory tract (asthma at- discriminating between asymptomatic sensitization tack, hoarseness, stridor/laryngeal angioedema) or the and a clinically relevant food allergy, and between cardiovascular system (dizziness, drop in blood pressure, loss different allergic phenotypes in an accurate and trust- of consciousness) [2,3]. -

Importance of Ag-Ab Reactions
Ag-Ab reactions Tests for Ag-Ab reactions EISA SALEHI PhD. Immunology Dept. TUMS Importance of Ag-Ab Reactions • Understand the mechanisms of defense • Abs as tools in: – Treatment – Diagnosis • As biomarkers • As tools to measure analytes Nature of Ag/Ab Reactions http://www.med.sc.edu:85/chime2/lyso-abfr.htm • Lock and Key Concept • Non-covalent Bonds – Hydrogen bonds – Electrostatic bonds – Van der Waal forces – Hydrophobic bonds • Multiple Bonds • Reversible Source: Li, Y., Li, H., Smith-Gill, S. J., Mariuzza, R. A., Biochemistry 39, 6296, 2000 Affinity • Strength of the reaction between a single antigenic determinant and a single Ab combining site High Affinity Low Affinity Ab Ab Ag Ag Affinity = ( attractive and repulsive forces Calculation of Affinity Ag + Ab ↔ Ag-Ab Applying the Law of Mass Action: [[gAg-Ab] Keq = [Ag] x [Ab] Avidity • The overall strength of binding between an Ag with many determinants and multivalent Abs 4 6 10 Keq = 10 10 10 Affinity Avidity Avidity SifiitSpecificity • The ability of an individual antibody combining site to react with only one antigenic determinant. • The ability of a population of antibody molecules to react with only one antigen. Cross Reactivity • The ability of an individual Ab combining site to react with more than one antigenic determinant. • The ability of a population of Ab molecules to react with more than one Ag Cross reactions Anti-A Anti-A Anti-A Ab Ab Ab Ag A Ag B Ag C Shared epitope Similar epitope Factors Affecting Measurement of A/AbRAg/Ab Reac tions • Affinity • Avidity Ab excess Ag excess • AAbiAg:Ab ratio •Phyygsical form of Ag Equivalence – Lattice formation Do you need to know what happens in Lab. -

Principles of Immunochemical Techniques Used in Clinical Laboratories
Review Received 2.11.06 | Revisions Received 3.1.06 | Accepted 3.2.06 Principles of Immunochemical Techniques Used in Clinical Laboratories Marja E. Koivunen, Richard L. Krogsrud (Antibodies Incorporated, Davis, CA) DOI: 10.1309/MV9RM1FDLWAUWQ3F Abstract binding site. The type of antibody and its diseases. Immunoassays can measure low Immunochemistry offers simple, rapid, robust affinity and avidity for the antigen determines levels of disease biomarkers and therapeutic or yet sensitive, and easily automated methods assay sensitivity and specificity. Depending on illicit drugs in patient’s blood, serum, plasma, for routine analyses in clinical laboratories. the assay format, immunoassays can be urine, or saliva. Immunostaining is an example Immunoassays are based on highly specific qualitative or quantitative. They can be used for of an immunochemical technique, which binding between an antigen and an antibody. the detection of antibodies or antigens specific combined with fluorescent labels allows direct An epitope (immunodeterminant region) on the for bacterial, viral, and parasitic diseases as visualization of target cells and cell structures. antigen surface is recognized by the antibody’s well as for the diagnosis of autoimmune Immunochemistry offers simple, rapid, robust yet sensitive, bind to an antigen. The third domain (complement-binding Fc and in most cases, easily automated methods applicable to routine fragment) forms the base of the Y, and is important in immune analyses in clinical laboratories. Immunochemical methods do not system function and regulation. usually require extensive and destructive sample preparation or The region of an antigen that interacts with an antibody is expensive instrumentation. In fact, most methods are based on called an epitope or an immunodeterminant region. -

Igm Autoantibody Testing by Latex Agglutination Nephelometry and Elisa in Patients with Rheumatoid Arthritis
European Journal of Molecular & Clinical Medicine ISSN 2515-8260 Volume 07, Issue 08, 2020 Comparative Study Of Rheumatoid Factor - Igm Autoantibody Testing By Latex Agglutination Nephelometry And Elisa In Patients With Rheumatoid Arthritis Dr.C. Devi1, Dr.R. Ravichandran2, Dr. Logeswari Selvaraj3, Dr.S. Ramesh4, Dr.T. Aarthipriya5 1,2,3,4,5Senior Assistant professor Department of Microbiology, Government Kilpauk Medical College, Chennai mail id: [email protected] ABSTRACT Objectives: To test Rheumatoid factor (RF) IgM autoantibody in Patients with Rheumatoid Arthritis by various methods like latex agglutination, Nephelometer and ELISA. Comparative analysis of the sensitivity and specificity of the tests performed. Materials and Methods: The study was conducted for a period of six months from June 2018 to November 2018 in a tertiary care hospital in Chennai. 90 patients attending Rheumatology OPD or admitted in the ward with the diagnosis of Rheumatoid arthritis, satisfying the inclusion and exclusion criteria were taken up for the study. Inclusion criteria: Clinically diagnosed Rheumatoid Arthritis patient as per revised ACR 1987 classification criteria. Duration of symptoms (1yr- early (RA) 1 Yr. (Established RA). Exclusion Criteria: Those with systemic connective tissue diseases like SLE, Scleroderma, MCTD, Sjogren syndrome, those with chronic liver diseases, tuberculosis, subacute Bacterial endocarditis, Pregnancy, Lympho reticular malignancies are excluded for the study. Those with onset 16 years of age are also excluded. Under aseptic precautions about 3ml of blood was collected from each Patient. Rheumatoid factor (RF) IgM was tested for each patient by all three methods Latex agglutination, Nephelometry and ELISA. Results: IgM rheumatoid factor (RF) was detected in the sera of 90 patients with Rheumatoid Arthritis. -

Prospective Comparison of Laser Nephelometry with Standard Agglutination Techniques for Detection of Rheumatoid Factor
J Clin Pathol: first published as 10.1136/jcp.40.2.216 on 1 February 1987. Downloaded from J Clin Pathol 1987;40:216-220 Prospective comparison of laser nephelometry with standard agglutination techniques for detection of rheumatoid factor A G PRENTICE,* P HICKLING,t I C WISEMAN,* C J HOLWILL,* J NORTHWOODt From the Departments oftRheumatology, *Haematology, and IMicrobiology, Derriford Hospital, Plymouth, Devon SUMMARY IgM rheumatoid factor was assayed by three routine methods: latex fixation; haem- agglutination; and end point laser nephelometry in 69 patients with definite or classical rheumatoid arthritis and 58 patients with other non-rheumatoid arthropathies, selected prospectively according to the American Rheumatism Association clinical criteria. The operators of the assays were unaware of the clinical diagnoses. In the group with rheumatoid arthritis 75-4% were positive by latex fixation, 73*9% by haemagglutination, and 55 1% by nephelometry. In the group with non- rheumatoid arthropathies 10-4% were positive by latex fixation, 8-6% by haemagglutination, and 10-4% by nephelometry. Thus the simple and inexpensive latex fixation test was as good as the haemagglutination test, and both were significantly better than nephelometry in the laboratory = confirmation of the clinical diagnosis ofdefinite or classic rheumatoid arthritis (X2 5.40 and 4 56,copyright. and p < 0 025 and < 0 05, respectively). None of these tests was significantly better or worse than the others in producing positive results in the group with non-rheumatoid arthropathies. The diagnosis of rheumatoid arthritis is largely based complexes, which scatter a beam of light in propor- on clinical evidence and depends on the fulfilment of tion to the concentration of the antibody in the test the criteria for definite or classic disease, as described serum. -

IMMUNOCHEMICAL TECHNIQUES Antigens Antibodies
Imunochemical Techniques IMMUNOCHEMICAL TECHNIQUES (by Lenka Fialová, translated by Jan Pláteník a Martin Vejražka) Antigens Antigens are macromolecules of natural or synthetic origin; chemically they consist of various polymers – proteins, polypeptides, polysaccharides or nucleoproteins. Antigens display two essential properties: first, they are able to evoke a specific immune response , either cellular or humoral type; and, second, they specifically interact with products of this immune response , i.e. antibodies or immunocompetent cells. A complete antigen – immunogen – consists of a macromolecule that bears antigenic determinants (epitopes) on its surface (Fig. 1). The antigenic determinant (epitope) is a certain group of atoms on the antigen surface that actually interacts with the binding site on the antibody or lymphocyte receptor for the antigen. Number of epitopes on the antigen surface determines its valency. Low-molecular-weight compound that cannot as such elicit production of antibodies, but is able to react specifically with the products of immune response, is called hapten (incomplete antigen) . antigen epitopes Fig. 1. Antigen and epitopes Antibodies Antibodies are produced by plasma cells that result from differentiation of B lymphocytes following stimulation with antigen. Antibodies are heterogeneous group of animal glycoproteins with electrophoretic mobility β - γ, and are also called immunoglobulins (Ig) . Every immunoglobulin molecule contains at least two light (L) and two heavy (H) chains connected with disulphidic bridges (Fig. 2). One antibody molecule contains only one type of light as well as heavy chain. There are two types of light chains - κ and λ - that determine type of immunoglobulin molecule; while heavy chains exist in 5 isotypes - γ, µ, α, δ, ε; and determine class of immunoglobulins - IgG, IgM, IgA, IgD and IgE . -

EUROPEAN PHARMACOPOEIA Free Access to Supportive Pharmacopoeial Texts in the Field of Vaccines for Human Use During the Coronavirus Disease (COVID-19) Pandemic
EUROPEAN PHARMACOPOEIA Free access to supportive pharmacopoeial texts in the field of vaccines for human use during the coronavirus disease (COVID-19) pandemic Updated package - October 2020 Published in accordance with the Convention on the Elaboration of a European Pharmacopoeia (European Treaty Series No. 50) European Directorate Direction européenne for the Quality de la qualité of Medicines du médicament & HealthCare & soins de santé Council of Europe Strasbourg Free access to supportive pharmacopoeial texts in the field of vaccines for human use during the coronavirus disease (COVID-19) pandemic Updated package The EDQM is committed to supporting users during the coronavirus disease (COVID-19) pandemic – as well as contributing to the wider global effort to combat the virus – by openly sharing knowledge and providing access to relevant guidance/standards. To support organisations involved in the development, manufacture or testing of COVID-19 vaccines worldwide, many of which are universities and small and medium-sized enterprises, the EDQM is offeringte mporary free access to texts of the European Pharmacopoeia (Ph. Eur.) in the field of vaccines. This package includes quality standards for vaccines which developers can take into account to help build appropriate analytical control strategies for their COVID-19 candidate vaccines and ensure the quality and safety of the final product. Application of such quality requirements may ultimately help to facilitate regulatory acceptance of a subsequent marketing authorisation application. For ease of reading, a summary table listing the pharmacopoeial texts, with information regarding the vaccine types or vaccine platforms concerned (e.g. live attenuated viral vaccine, recombinant viral-vectored vaccines) is provided. -

Antibodies As Diagnostic Targets and As Reagents for Diagnostics
antibodies Editorial Antibodies as Diagnostic Targets and as Reagents for Diagnostics Nicole H. Trier and Gunnar Houen * Department of Neurology, Rigshospitalet Glostrup, Valdemar Hansens vej 13, 2600 Glostrup, Denmark; [email protected] * Correspondence: [email protected]; Tel.: +45-3863-3863 Received: 19 April 2020; Accepted: 22 April 2020; Published: 18 May 2020 Antibodies (Abs) were discovered around the turn of the 19th century and characterized in the following decades as an essential part of the human adaptive immune system [1,2]. Abs are produced in response to infections with pathogenic organisms and therefore have diagnostic potential. The levels of specific Abs reflect the burden of infection and the type of Abs produced may reflect the duration of infection and the site of infection, since Abs undergo class switching and affinity maturation in the course of infections [1,2]. Initially IgM is produced, but switching to IgG, IgA or IgE occurs during infections, depending on the type of pathogen and the site of infection. The use of Abs as targets of diagnostics can roughly be divided in five areas: 1. Infections The specificity, type and concentration of Abs have diagnostic value. The specificity giving information on the type of pathogen, the type and concentration giving information on the state of infection (IgM as an indication of early infection, IgG and IgA as indications of prolonged or chronic infections (IgA further indicating mucosal/epithelial infection)) [2]. 2. Autoimmune Diseases The specificity, type and concentration of auto-Abs have diagnostic value. The specificity and the type giving information on the tissue/organ involved (IgA indicating mucosal/epithelial affection, IgM being relevant in a few conditions), the concentration giving some information on the degree of affection [3]. -

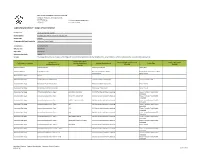
LABORATORY - TESTING for the Time Period : 10/01/16 and 09/30/2017
LABORATORY - TESTING For the Time Period : 10/01/16 and 09/30/2017 IF YOU ARE COVERED BY HEALTH INSURANCE , YOU ARE STRONGLY ENCOURAGED TO CONSULT WITH YOUR HEALTH INSURER TO DETERMINE ACCURATE INFORMATION ABOUT YOUR FINACIAL RESPONSIBILITY FOR A PARTICULAR HEALTH CARE SERVICE PROVIDED AT THIS HEALTHCARE FACILITY. IF YOU ARE NOT COVERED BY HEALTH INSURANCE YOU ARE STRONGLY ENCOURAGED TO CONTACT THE BUSINESS OFFICE AT (719)584-4508 OR TOLL FREE AT 800-543-4046 TO DISCUSS PAYMENT OPTIONS PRIOR TO RECEIVING A HEALTH CARE SERVICE FROM THIS HEALTH CARE FACILITY SINCE POSTED HEALTHCARE SERVICES MAY NOT REFLECT THE ACTUAL AMOUNT OF YOUR FINANCIAL RESPONSIBILITY. Note: 1. The pricing on this page is for Laboratory testing only. It is not combined pricing with other testing 2. Charging is based on the Length of Stay, amount of supplies used, therapies provided, testing given as well as other care provided 3. This pricing is an average charge and not intended to be the exact charge for any particular patient 4. The average charge shown is an estimate and that actual charges for the service depend on the circumstances at the time the service is provided and the patient. 5. Any discount is negotiated by the insurance provider. Most insurance providers should be able to tell their members what financial responsibility they will have. 6. Patients without insurance are able to receive a discount equal to the insurance provider with the lowest negotiated discount CPT Description Average Charge 80048 METABOLIC PANEL TOTAL CA $ 1,198.36 80050 GENERAL HEALTH -

Modpathol201624.Pdf
ANNUAL MEETING ABSTRACTS 509A 2022 Quick Review of Fine Needle Aspiration Accuracy with Focus on mcg/L, which correlates with cirrhosis, was 76% specific for C282Y. Most C282Y Cytohistologic Correlation and Evaluation of Discrepant Cases in a Limited heterozygotes (4) and C282Y/C282Y (13) patients with available results met these cut Sample offs, and two C282Y patients met criteria based on family history alone. Somaye Yekezare, Niloufar Reisian, Xiaoyan Liao, Farnaz Hasteh. University of Conclusions: The proposed criteria of TS>45%, ferritin>1,000 mcg/L, or a positive California San Diego Health System, San Diego, CA; Kaiser Medical Center, San family history, was 100% sensitive and moderately specific for C282Y screening. Diego, CA. Our institution is now considering an approach to include measuring ferritin/TS, and Background: Fine needle aspiration biopsy (FNAB) is a minimally invasive procedure reflexive HFE gene testing only when criteria are met. If used broadly, the algorithm commonly utilized for the primary investigation of mass lesions. Correlation of FNAB should detect all at-risk patients and result in an estimated 43% reduction of unnecessary diagnosis with histopathologic results is part of quality assurance and quality control HFE tests and a lower cost per new diagnosis. in cytology laboratories. The aim of this study was to investigate the diagnostic performance of FNAB and to identify the specimen types that are prone to errors. Design: A total of 1125 FNABs performed at our institutes in 2013 were selected and Techniques (including Ultrastructure) 401 satisfactory cases with the follow-up surgical specimens were included for this study. FNAB results were classified as negative, atypia, or positive; whereas final pathologic 2024 Complementary Value of Electron Microscopy and diagnoses were classified as malignant or benign. -
Scope of Accreditation
DIAGNOSTIC ACCREDITATION PROGRAM College of Physicians and Surgeons of BC Telephone: 604-733-7758 300–669 Howe Street Vancouver BC V6C 0B4 Toll free: 1-800-461-3008 (in BC) www.cpsbc.ca Fax: 604-733-3503 Laboratory Medicine – Scope of Accreditation Facility name Vancouver General Hospital Facility address 855 West 12th Avenue, Vancouver, BC, V5Z 1M9 Facility code 0610LM Corporate entity/health authority Vancouver Coastal Health Accreditation Full Accreditation Effective date 2019-03-28 Expiry date 2024-02-27 Laboratory Standards Version 1.4 Services The College of Physicians and Surgeons of BC Diagnostic Accreditation Program accredits the capability of the named facility to perform the listed services and examinations/procedures. Examination – Other Examination Methodology/principle – Other Sample Type – Other DAP Scope Classification (Analyte/Procedure) Methodology/principle Sample Type (Analyte/Procedure) (Specify) (Specify) (Specify) Sample Collection Sample Collection Venous and Capillary Whole Blood Sample Collection Sample Processing Receipt, accessioning, storage, Blood, fluids, stool, tissues, swabs, transportation foreign bodies Anatomical Pathology Autopsy Anatomical Pathology Fixation and Gross examination Fixation and gross examination Tissue - Formalin Fixed Anatomical Pathology Fixation and Gross examination Fixation and gross examination Tissue - Fresh Anatomical Pathology Immunofluorescence microscopy Microscopy - Fluorescent Tissue - Frozen Anatomical Pathology Immunohistochemistry - Class I p63, CD15, CX2, CD56 IHC -

Distinction of Human Immunodeficiency Virus Type 1 Neutralization and Infection Enhancement by Human Monoclonal Antibodies to Glycoprotein 120 Akira Takeda,* James E
Distinction of Human Immunodeficiency Virus Type 1 Neutralization and Infection Enhancement by Human Monoclonal Antibodies to Glycoprotein 120 Akira Takeda,* James E. Robinson, David D. Ho, Chrisfine Debouck, Nancy L. Haigwood, and Francis A. Ennis* *Division ofInfectious Diseases, Department ofMedicine, University ofMassachusetts Medical School, Worcester, Massachusetts 01655; Department ofPediatrics and Microbiology, Immunology and Parasitology, Louisiana State University School ofMedicine, New Orleans, Louisiana 70112; Division ofInfectious Diseases, The Aaron Diamond AIDS Research Center, New York University School of Medicine, New York 10016; Department ofMolecular Genetics, Smith Kline Beecham Pharmaceuticals, King ofPrussia, Pennsylvania 19479; and Chiron Corporation, Emeryville, California 94608 Abstract reference to HIV vaccine development, since very low concen- trations of anti-HIV- 1 antibodies can enhance HIV-1 infec- There is increasing evidence that sera from HIV-1-infected tion. Robinson et al. first reported complement-mediated en- individuals contain antibodies that enhance infection by HIV-1 hancement of HIV- 1 infection in a T cell line bearing comple- in vitro. Previous work has demonstrated that complement re- ment receptors (1). We have previously demonstrated ceptors on T lymphoid cells and Fc receptors for IgG (Fc'yR) on antibody-dependent enhancement of HIV-l infection via Fc monocytic cells are required for enhanced infection by anti- receptor (FcR)'-mediated entry using a human monocytic cell body-complexed HIV-1. Characterization of such infection-en- line U937 that possesses FcRs for IgG (3). Heat-inactivated hancing antibodies is essential because immunogenic epitopes sera from HIV- 1 antibody-positive individuals enhanced infec- which induce enhancing antibodies should be excluded from tion ofU937 cells.