Genetic Regulation of NKT Cell Function
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Single-Cell Profiling Identifies Impaired Adaptive NK Cells Expanded After HCMV Reactivation in Haploidentical HSCT
Single-cell profiling identifies impaired adaptive NK cells expanded after HCMV reactivation in haploidentical HSCT Elisa Zaghi, … , Enrico Lugli, Domenico Mavilio JCI Insight. 2021;6(12):e146973. https://doi.org/10.1172/jci.insight.146973. Research Article Hematology Immunology Graphical abstract Find the latest version: https://jci.me/146973/pdf RESEARCH ARTICLE Single-cell profiling identifies impaired adaptive NK cells expanded after HCMV reactivation in haploidentical HSCT Elisa Zaghi,1 Michela Calvi,1,2 Simone Puccio,3 Gianmarco Spata,1 Sara Terzoli,1 Clelia Peano,4 Alessandra Roberto,3 Federica De Paoli,3 Jasper J.P. van Beek,3 Jacopo Mariotti,5 Chiara De Philippis,5 Barbara Sarina,5 Rossana Mineri,6 Stefania Bramanti,5 Armando Santoro,5 Vu Thuy Khanh Le-Trilling,7 Mirko Trilling,7 Emanuela Marcenaro,8 Luca Castagna,5 Clara Di Vito,1,2 Enrico Lugli,3,9 and Domenico Mavilio1,2 1Unit of Clinical and Experimental Immunology, IRCCS Humanitas Research Hospital, Rozzano, Milan, Italy. 2BIOMETRA, Università degli Studi di Milano, Milan, Italy. 3Laboratory of Translational Immunology, 4Institute of Genetic and Biomedical Research, UoS Milan, National Research Council, and Genomic Unit, 5Bone Marrow Transplant Unit, and 6Molecular Biology Section, Clinical Investigation Laboratory, IRCCS Humanitas Research Hospital, Milan, Italy. 7Institute for Virology, University Hospital Essen, University Duisburg-Essen, Essen, Germany. 8Department of Experimental Medicine, University of Genoa, Genoa, Italy. 9Flow Cytometry Core, IRCCS Humanitas Research Hospital, Milan, Italy. Haploidentical hematopoietic stem cell transplantation (h-HSCT) represents an efficient curative approach for patients affected by hematologic malignancies in which the reduced intensity conditioning induces a state of immunologic tolerance between donor and recipient. -

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -

Role of RUNX1 in Aberrant Retinal Angiogenesis Jonathan D
Page 1 of 25 Diabetes Identification of RUNX1 as a mediator of aberrant retinal angiogenesis Short Title: Role of RUNX1 in aberrant retinal angiogenesis Jonathan D. Lam,†1 Daniel J. Oh,†1 Lindsay L. Wong,1 Dhanesh Amarnani,1 Cindy Park- Windhol,1 Angie V. Sanchez,1 Jonathan Cardona-Velez,1,2 Declan McGuone,3 Anat O. Stemmer- Rachamimov,3 Dean Eliott,4 Diane R. Bielenberg,5 Tave van Zyl,4 Lishuang Shen,1 Xiaowu Gai,6 Patricia A. D’Amore*,1,7 Leo A. Kim*,1,4 Joseph F. Arboleda-Velasquez*1 Author affiliations: 1Schepens Eye Research Institute/Massachusetts Eye and Ear, Department of Ophthalmology, Harvard Medical School, 20 Staniford St., Boston, MA 02114 2Universidad Pontificia Bolivariana, Medellin, Colombia, #68- a, Cq. 1 #68305, Medellín, Antioquia, Colombia 3C.S. Kubik Laboratory for Neuropathology, Massachusetts General Hospital, 55 Fruit St., Boston, MA 02114 4Retina Service, Massachusetts Eye and Ear Infirmary, Department of Ophthalmology, Harvard Medical School, 243 Charles St., Boston, MA 02114 5Vascular Biology Program, Boston Children’s Hospital, Department of Surgery, Harvard Medical School, 300 Longwood Ave., Boston, MA 02115 6Center for Personalized Medicine, Children’s Hospital Los Angeles, Los Angeles, 4650 Sunset Blvd, Los Angeles, CA 90027, USA 7Department of Pathology, Harvard Medical School, 25 Shattuck St., Boston, MA 02115 Corresponding authors: Joseph F. Arboleda-Velasquez: [email protected] Ph: (617) 912-2517 Leo Kim: [email protected] Ph: (617) 912-2562 Patricia D’Amore: [email protected] Ph: (617) 912-2559 Fax: (617) 912-0128 20 Staniford St. Boston MA, 02114 † These authors contributed equally to this manuscript Word Count: 1905 Tables and Figures: 4 Diabetes Publish Ahead of Print, published online April 11, 2017 Diabetes Page 2 of 25 Abstract Proliferative diabetic retinopathy (PDR) is a common cause of blindness in the developed world’s working adult population, and affects those with type 1 and type 2 diabetes mellitus. -
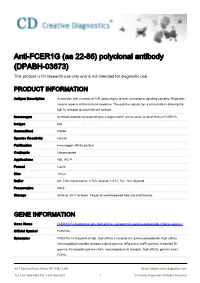
Anti-FCER1G (Aa 22-86) Polyclonal Antibody (DPABH-03673) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-FCER1G (aa 22-86) polyclonal antibody (DPABH-03673) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description Associates with a variety of FcR alpha chains to form a functional signaling complex. Regulates several aspects of the immune response. The gamma subunit has a critical role in allowing the IgE Fc receptor to reach the cell surface. Immunogen Synthetic peptide corresponding to a region within amino acids 22-86 of Human FCER1G. Isotype IgG Source/Host Rabbit Species Reactivity Human Purification Immunogen affinity purified Conjugate Unconjugated Applications WB, IHC-P Format Liquid Size 100 μl Buffer pH: 7.00; Constituents: 0.75% Glycine, 1.21% Tris, 10% Glycerol Preservative None Storage Store at -20°C or lower. Aliquot to avoid repeated freezing and thawing. GENE INFORMATION Gene Name FCER1G Fc fragment of IgE, high affinity I, receptor for; gamma polypeptide [ Homo sapiens ] Official Symbol FCER1G Synonyms FCER1G; Fc fragment of IgE, high affinity I, receptor for; gamma polypeptide; high affinity immunoglobulin epsilon receptor subunit gamma; fcRgamma; fceRI gamma; fc-epsilon RI- gamma; Fc receptor gamma-chain; immunoglobulin E receptor, high affinity, gamma chain; FCRG; 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved Entrez Gene ID 2207 Protein Refseq NP_004097 UniProt ID P30273 Chromosome Location 1q23 Pathway Asthma; Cell surface interactions at the vascular wall; Fc epsilon RI signaling pathway; Fc- epsilon receptor I signaling in mast cells; GPVI-mediated activation cascade; Function IgE binding; IgG binding; receptor activity; transmembrane signaling receptor activity; 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 2 © Creative Diagnostics All Rights Reserved. -

Supplementary Figures and Tables
SUPPLEMENTARY DATA Supplementary Figure 1. Isolation and culture of endothelial cells from surgical specimens of FVM. (A) Representative pre-surgical fundus photograph of a right eye exhibiting a FVM encroaching on the optic nerve (dashed line) causing tractional retinal detachment with blot hemorrhages throughout retina (arrow heads). (B) Magnetic beads (arrows) allow for separation and culturing of enriched cell populations from surgical specimens (scale bar = 100 μm). (C) Cultures of isolated cells stained positively for CD31 representing a successfully isolated enriched population (scale bar = 40 μm). ©2017 American Diabetes Association. Published online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db16-1035/-/DC1 SUPPLEMENTARY DATA Supplementary Figure 2. Efficient siRNA knockdown of RUNX1 expression and function demonstrated by qRT-PCR, Western Blot, and scratch assay. (A) RUNX1 siRNA induced a 60% reduction of RUNX1 expression measured by qRT-PCR 48 hrs post-transfection whereas expression of RUNX2 and RUNX3, the two other mammalian RUNX orthologues, showed no significant changes, indicating specificity of our siRNA. Functional inhibition of Runx1 signaling was demonstrated by a 330% increase in insulin-like growth factor binding protein-3 (IGFBP3) RNA expression level, a known target of RUNX1 inhibition. Western blot demonstrated similar reduction in protein levels. (B) siRNA- 2’s effect on RUNX1 was validated by qRT-PCR and western blot, demonstrating a similar reduction in both RNA and protein. Scratch assay demonstrates functional inhibition of RUNX1 by siRNA-2. ns: not significant, * p < 0.05, *** p < 0.001 ©2017 American Diabetes Association. Published online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db16-1035/-/DC1 SUPPLEMENTARY DATA Supplementary Table 1. -
Microarray Analysis of Novel Genes Involved in HSV- 2 Infection
Microarray analysis of novel genes involved in HSV- 2 infection Hao Zhang Nanjing University of Chinese Medicine Tao Liu ( [email protected] ) Nanjing University of Chinese Medicine https://orcid.org/0000-0002-7654-2995 Research Article Keywords: HSV-2 infection,Microarray analysis,Histospecic gene expression Posted Date: May 12th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-517057/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/19 Abstract Background: Herpes simplex virus type 2 infects the body and becomes an incurable and recurring disease. The pathogenesis of HSV-2 infection is not completely clear. Methods: We analyze the GSE18527 dataset in the GEO database in this paper to obtain distinctively displayed genes(DDGs)in the total sequential RNA of the biopsies of normal and lesioned skin groups, healed skin and lesioned skin groups of genital herpes patients, respectively.The related data of 3 cases of normal skin group, 4 cases of lesioned group and 6 cases of healed group were analyzed.The histospecic gene analysis , functional enrichment and protein interaction network analysis of the differential genes were also performed, and the critical components were selected. Results: 40 up-regulated genes and 43 down-regulated genes were isolated by differential performance assay. Histospecic gene analysis of DDGs suggested that the most abundant system for gene expression was the skin, immune system and the nervous system.Through the construction of core gene combinations, protein interaction network analysis and selection of histospecic distribution genes, 17 associated genes were selected CXCL10,MX1,ISG15,IFIT1,IFIT3,IFIT2,OASL,ISG20,RSAD2,GBP1,IFI44L,DDX58,USP18,CXCL11,GBP5,GBP4 and CXCL9.The above genes are mainly located in the skin, immune system, nervous system and reproductive system. -

Haplotype Analysis in Multiple Crosses to Identify a QTL Gene
Downloaded from genome.cshlp.org on September 27, 2021 - Published by Cold Spring Harbor Laboratory Press Methods Haplotype Analysis in Multiple Crosses to Identify a QTL Gene Xiaosong Wang,1 Ron Korstanje, David Higgins, and Beverly Paigen The Jackson Laboratory, Bar Harbor, Maine 04609, USA Identifying quantitative trait locus (QTL) genes is a challenging task. Herein, we report using a two-step process to identify Apoa2 as the gene underlying Hdlq5, a QTL for plasma high-density lipoprotein cholesterol (HDL) levels on mouse chromosome 1. First, we performed a sequence analysis of the Apoa2 coding region in 46 genetically diverse mouse strains and found five different APOA2 protein variants, which we named APOA2a to APOA2e. Second, we conducted a haplotype analysis of the strains in 21 crosses that have so far detected HDL QTLs; we found that Hdlq5 was detected only in the nine crosses where one parent had the APOA2b protein variant characterized by an Ala61-to-Val61 substitution. We then found that strains with the APOA2b variant had significantly higher (P Յ 0.002) plasma HDL levels than those with either the APOA2a or the APOA2c variant. These findings support Apoa2 as the underlying Hdlq5 gene and suggest the Apoa2 polymorphisms responsible for the Hdlq5 phenotype. Therefore, haplotype analysis in multiple crosses can be used to support a candidate QTL gene. [Supplemental material is available online at www.genome.org. The following individuals kindly provided reagents, samples, or unpublished information as indicated in the paper: D. Puppione.] Most common human diseases, such as atherosclerosis, diabetes, 46 genetically diverse mouse strains, and a haplotype analysis of and obesity, are complex traits determined by many genetic and strains both in the nine crosses that detected Hdlq5 and in the 12 environmental factors. -

Bioinformatic Analysis Reveals Novel Hub Genes Pathways Associated
Bioinformatic Analysis Reveals Novel Hub Genes pathways associated with IgA nephropathy xue Jiang Hangzhou Hospital of Traditional Chinese Medicine Zhijie Xu Zhejiang University School of Medicine First Aliated Hospital Yuanyuan Du Hangzhou Hospital of Traditional Chinese Medicine Hongyu Chen ( [email protected] ) Hangzhou Hospital of Traditional Chinese Medicine https://orcid.org/0000-0002-8207-1421 Research Keywords: IgA nephropathy, Gene Expression Proling, Bioinformatic Analysis Posted Date: May 22nd, 2020 DOI: https://doi.org/10.21203/rs.3.rs-29974/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published on September 7th, 2020. See the published version at https://doi.org/10.1186/s40001-020-00441-2. Page 1/18 Abstract Background Immunoglobulin A nephropathy (IgAN) is the most common primary glomerulopathy worldwide. However, the molecular events underlying IgAN remain to be fully elucidated. The aim of the study is to identify novel biomarkers of IgAN through bioinformatics analysis and elucidate the possible molecular mechanism. Methods Based on the microarray data GSE93798 and GSE37460 were downloaded from the Gene Expression Omnibus database, the differentially expressed genes (DEGs) between IgAN samples and normal controls were identied. With DEGs, we further performed a series of functional enrichment analyses. Protein- protein interaction (PPI) networks of the DEGs were built with the STRING online search tool and visualized by using Cytoscape, then further identied the hub gene and most important module in DEGs, Biological Networks Gene Oncology tool (BiNGO) were then performed to elucidate the molecular mechanism of IgAN. -

FCER1G Rabbit Polyclonal Antibody – TA339393 | Origene
OriGene Technologies, Inc. 9620 Medical Center Drive, Ste 200 Rockville, MD 20850, US Phone: +1-888-267-4436 [email protected] EU: [email protected] CN: [email protected] Product datasheet for TA339393 FCER1G Rabbit Polyclonal Antibody Product data: Product Type: Primary Antibodies Applications: WB Recommended Dilution: WB Reactivity: Human Host: Rabbit Isotype: IgG Clonality: Polyclonal Immunogen: The immunogen for anti-FCER1G antibody: synthetic peptide directed towards the N terminal of human FCER1G. Synthetic peptide located within the following region: MIPAVVLLLLLLVEQAAALGEPQLCYILDAILFLYGIVLTLLYCRLKIQV Formulation: Liquid. Purified antibody supplied in 1x PBS buffer with 0.09% (w/v) sodium azide and 2% sucrose. Note that this product is shipped as lyophilized powder to China customers. Concentration: lot specific Purification: Protein A purified Conjugation: Unconjugated Storage: Store at -20°C as received. Stability: Stable for 12 months from date of receipt. Predicted Protein Size: 8 kDa Gene Name: Fc fragment of IgE receptor Ig Database Link: NP_004097 Entrez Gene 2207 Human P30273 Background: The high affinity IgE receptor is a key molecule involved in allergic reactions. It is a tetramer composed of 1 alpha, 1 beta, and 2 gamma chains. The gamma chains are also subunits of other Fc receptors. [provided by RefSeq, Jul 2008] Synonyms: FCRG This product is to be used for laboratory only. Not for diagnostic or therapeutic use. View online » ©2021 OriGene Technologies, Inc., 9620 Medical Center Drive, Ste 200, Rockville, MD 20850, US 1 / 2 FCER1G Rabbit Polyclonal Antibody – TA339393 Note: Immunogen Sequence Homology: Dog: 100%; Pig: 100%; Human: 100%; Mouse: 100%; Bovine: 100%; Guinea pig: 100%; Rat: 93% Protein Families: Transmembrane Protein Pathways: Asthma, Fc epsilon RI signaling pathway, Natural killer cell mediated cytotoxicity Product images: WB Suggested Anti-FCER1G Antibody Titration: 0.2-1 ug/ml; ELISA Titer: 1: 62500; Positive Control: Hela cell lysate This product is to be used for laboratory only. -

The Diverse Functions of the Ubiquitous Fc Receptors and Their
pathogens Review The Diverse Functions of the Ubiquitous Fcγ Receptors and Their Unique Constituent, FcRγ Subunit Thamer A. Hamdan 1,*, Philipp A. Lang 2 and Karl S. Lang 1 1 Institute of Immunology, Medical Faculty, University of Duisburg-Essen, Hufelandstraße 55, 45147 Essen, Germany 2 Department of Molecular Medicine II, Medical Faculty, Heinrich Heine University, Universitätsstrasse 1, 40225 Düsseldorf, Germany * Correspondence: [email protected] Received: 8 December 2019; Accepted: 17 February 2020; Published: 20 February 2020 Abstract: Fc gamma receptors (FcγRs) are widely expressed on a variety of immune cells and play a myriad of regulatory roles in the immune system because of their structural diversity. Apart from their indispensable role in specific binding to the Fc portion of antibody subsets, FcγRs manifest diverse biological functions upon binding to their putative ligands. Examples of such manifestation include phagocytosis, presentation of antigens, mediation of antibody-dependent cellular cytotoxicity, anaphylactic reactions, and the promotion of apoptosis of T cells and natural killer cells. Functionally, the equilibrium between activating and inhibiting FcγR maintains the balance between afferent and efferent immunity. The γ subunit of the immunoglobulin Fc receptor (FcRγ) is a key component of discrete immune receptors and Fc receptors including the FcγR family. Furthermore, FcγRs exert a key role in terms of crosslinking the innate and adaptive workhorses of immunity. Ablation of one of these receptors might positively or negatively influence the immune response. Very recently, we discovered that FcRγ derived from natural cytotoxicity triggering receptor 1 (NCR1) curtails CD8+ T cell expansion and thereby turns an acute viral infection into a chronic one. -
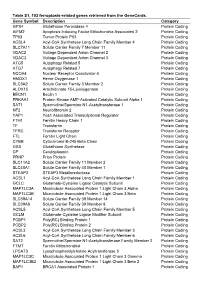
Table S1. 103 Ferroptosis-Related Genes Retrieved from the Genecards
Table S1. 103 ferroptosis-related genes retrieved from the GeneCards. Gene Symbol Description Category GPX4 Glutathione Peroxidase 4 Protein Coding AIFM2 Apoptosis Inducing Factor Mitochondria Associated 2 Protein Coding TP53 Tumor Protein P53 Protein Coding ACSL4 Acyl-CoA Synthetase Long Chain Family Member 4 Protein Coding SLC7A11 Solute Carrier Family 7 Member 11 Protein Coding VDAC2 Voltage Dependent Anion Channel 2 Protein Coding VDAC3 Voltage Dependent Anion Channel 3 Protein Coding ATG5 Autophagy Related 5 Protein Coding ATG7 Autophagy Related 7 Protein Coding NCOA4 Nuclear Receptor Coactivator 4 Protein Coding HMOX1 Heme Oxygenase 1 Protein Coding SLC3A2 Solute Carrier Family 3 Member 2 Protein Coding ALOX15 Arachidonate 15-Lipoxygenase Protein Coding BECN1 Beclin 1 Protein Coding PRKAA1 Protein Kinase AMP-Activated Catalytic Subunit Alpha 1 Protein Coding SAT1 Spermidine/Spermine N1-Acetyltransferase 1 Protein Coding NF2 Neurofibromin 2 Protein Coding YAP1 Yes1 Associated Transcriptional Regulator Protein Coding FTH1 Ferritin Heavy Chain 1 Protein Coding TF Transferrin Protein Coding TFRC Transferrin Receptor Protein Coding FTL Ferritin Light Chain Protein Coding CYBB Cytochrome B-245 Beta Chain Protein Coding GSS Glutathione Synthetase Protein Coding CP Ceruloplasmin Protein Coding PRNP Prion Protein Protein Coding SLC11A2 Solute Carrier Family 11 Member 2 Protein Coding SLC40A1 Solute Carrier Family 40 Member 1 Protein Coding STEAP3 STEAP3 Metalloreductase Protein Coding ACSL1 Acyl-CoA Synthetase Long Chain Family Member 1 Protein -

Role for High-Affinity Ige Receptor in Prognosis of Lung Adenocarcinoma Patients
Published OnlineFirst August 3, 2017; DOI: 10.1158/2326-6066.CIR-16-0392 Research Article Cancer Immunology Research Role for High-Affinity IgE Receptor in Prognosis of Lung Adenocarcinoma Patients Dalam Ly1,2, Chang-Qi Zhu3, Michael Cabanero3, Ming-Sound Tsao3,4, and Li Zhang1,2,4 Abstract Cancer development and biology is influenced by the host 10 additional independently published microarray datasets of immune system. Emerging data indicate that the context of lung adenocarcinoma [n ¼ 1,097; overall survival hazard ratio immune cell infiltrates may contribute to cancer prognosis. (HR), 2.05; 95% confidence interval, 1.64–2.56; P < 0.0001] However, the types of infiltrating immune cells that are critical and was found to be an independent prognostic indicator for cancer development remain controversial. In attempts to relative to tumor stage (overall survival HR, 2.09, 95% con- gain insights into the immune networks that regulate and/or fidence interval, 1.65–2.66; P < 0.0001). Network analysis predict tumor progression, gene expression analysis was con- revealed that genes associated with Fce complex (FCER1, ducted on microarray datasets of resected tumor samples from MS4A2) formed the largest and most significant pathway of 128 early-stage non–small cell lung cancer (NSCLC) adeno- the signature. Using immunohistochemistry, we validated that carcinoma patients. By limiting analysis to immune-related MS4A2, the b subunit of the IgE receptor expressed on mast genes, we identified a 9-gene signature using MAximizing R cells, is a favorable prognostic indicator and show that MS4A2 Square Algorithm that selected for the greatest separation gene expression is an independent prognostic marker for between favorable and adverse prognostic patient subgroups.