Final Program
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hepatic Surgery
Hepatic Surgery Honorary Editors: Tan To Cheung, Long R. Jiao Editors: Zhiming Wang, Giovanni Battista Levi Sandri, Alexander Parikh Associate Editors: Yiming Tao, Michael D. Kluger, Romaric Loffroy Editors: Zhiming Wang, Giovanni Battista Levi Sandri, Levi Battista Giovanni Alexander Parikh Hepatic Surgery Honorary Editors: Tan To Cheung, Long R. Jiao Editors: Zhiming Wang, Giovanni Battista Levi Sandri, Alexander Parikh Associate Editors: Yiming Tao, Michael D. Kluger, Romaric Loffroy AME Publishing Company Room C 16F, Kings Wing Plaza 1, NO. 3 on Kwan Street, Shatin, NT, Hong Kong Information on this title: www.amegroups.com For more information, contact [email protected] Copyright © AME Publishing Company. All rights reserved. This publication is in copyright. Subject to statutory exception and to the provisions of relevant collective licensing agreements, no reproduction of any part may take place without the written permission of AME Publishing Company. First published in 2018 Printed in China by AME Publishing Company Editors: Zhiming Wang, Giovanni Battista Levi Sandri, Alexander Parikh Hepatic Surgery (Hard Cover) ISBN: 978-988-78919-1-8 AME Publishing Company, Hong Kong AME Publishing Company has no responsibility for the persistence or accuracy of URLs for external or third-party internet websites referred to in this publication, and does not guarantee that any content on such websites is, or will remain, accurate or appropriate. The advice and opinions expressed in this book are solely those of the authors and do not necessarily represent the views or practices of the publisher. No representation is made by the publisher about the suitability of the information contained in this book, and there is no consent, endorsement or recommendation provided by the publisher, express or implied, with regard to its contents. -

Rectal Free Perforation After Stapled Hemorrhoidopexy: a Case Report
CASE REPORT – OPEN ACCESS International Journal of Surgery Case Reports 30 (2017) 40–42 View metadata, citation and similar papers at core.ac.uk brought to you by CORE Contents lists available at ScienceDirect provided by Elsevier - Publisher Connector International Journal of Surgery Case Reports journal homepage: www.casereports.com Rectal free perforation after stapled hemorrhoidopexy: A case report ଝ of laparoscopic peritoneal lavage and repair without stoma a b,∗ Seokyong Ryu , Byung-Noe Bae a Department of Emergency Medicine, Inje University Snaggye Paik Hospital, Seoul, Republic of Korea b Department of General Surgery, Inje University Snaggye Paik Hospital, Seoul,Republic of Korea a r t i c l e i n f o a b s t r a c t Article history: INTRODUCTION: Stapled hemorrhoidopexy is widely performed for treatment of prolapsed hemorrhoids Received 30 August 2016 because of advantages, including shorter hospital stay and less discomfort, compared with conventional Received in revised form hemorrhoidectomy. However, it can have severe adverse effects, such as rectal bleeding, perforation, and 18 November 2016 sepsis. Accepted 18 November 2016 PRESENTATION OF CASE: We report the case of a healthy 28-year-old man who presented to the emer- Available online 21 November 2016 gency department with sudden-onset diffuse abdominal pain and hematochezia. He had undergone stapled hemorrhoidopexy 5 days earlier and was discharged after an uneventful postoperative course. For Keywords: the present condition, after immediate evaluation, we successfully performed emergency laparoscopic Rectal perforation repair of the rectal perforation without any stoma. His postoperative course was uneventful, and he was Stapled hemorrhoidopexy Laparoscopic surgery discharged on postoperative day 16. -

Rectal Foreign Body: a Primer for Emergency Physicians Bobby Desai
Desai International Journal of Emergency Medicine 2011, 4:73 http://www.intjem.com/content/4/1/73 CASEREPORT Open Access Visual diagnosis: Rectal foreign body: A primer for emergency physicians Bobby Desai Abstract We present a case that is occasionally seen within emergency departments, namely a rectal foreign body. After presentation of the case, a discussion concerning this entity is given, with practical information on necessity of an accurate and thorough history and removal of the object for clinicians. Case anoscope inserted. The object could not be visualized, A 39-year-old male presented to the Emergency Depart- and therefore no attempt was made to remove it. Gen- ment with vague complaints of abdominal pain and con- eral surgery was consulted to see the patient and stipation. He stated that the abdominal pain was dull decided to take him to the operating room for removal. and crampy in nature and generalized in distribution. The patient agreed to this. Furthermore, he stated that he had not had a bowel The object was noted to be the extension arm of a movement in 2 days, though he felt as if he had to have vacuum cleaner. It was removed according to notes with one. He denied constitutional complaints of fevers, some difficulty and the patient was admitted to the hos- chills, nausea, and vomiting, and denied urinary com- pital for observation and intravenous antibiotics. The plaints as well. patient was subsequently discharged 2 days later in The patient’s vital signs were: temperature 37.2°C, excellent condition. Upon social work discharge, he was pulse 87 beats per minute, respiratory rate of 20 per again asked how that apparatus managed to be placed minute, and blood pressure 130/84 mmHg. -

A 20-Year Experience of Rectovaginal Fistula Management in a Tertiary University Hospital in Thailand
A 20-year Experience of Rectovaginal Fistula Management in a Tertiary University Hospital in Thailand Varut Lohsiriwat MD, PhD*, Danupon Arsapanom MD*, Siriluck Prapasrivorakul MD*, Cherdsak Iramaneerat MD*, Woramin Riansuwan MD*, Wiroon Boonnuch MD*, Darin Lohsiriwat MD* * Colorectal Surgery Unit, Division of General Surgery, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand Objective: The purpose of this study was to determine etiology, treatment and outcome of patients with rectovaginal fistula (RVF) who were treated in a tertiary university hospital in Thailand. Material and Method: The authors retrospectively reviewed the medical records of patients with RVF treating from 1994 to 2013 at the Faculty of Medicine Siriraj Hospital. Data were recorded including patient’s demographics, etiology, treatment and outcome. Results: This study included 108 patients with median age of 55 years (range 24 to 81). Radiation injury was the most common cause of RVF (44%) followed by direct invasion of rectal or gynecologic malignancies (20%), postoperative complication (16%) (notably from 10 low anterior resections, 5 transabdominal hysterectomies, 1 stapled hemorrhoidopexy and 1 injection sclerotherapy for hemorrhoid) and obstetric injury (11%). Diverting colostomy was the most frequent operation performed for both radiation-related RVF and malignancy-related RVF. Most operation-related RVF were healed after fecal diversion with or without either local repair or major resection. All obstetric-related RVFs were successfully treated by local tissue repair with or without anal sphincteroplasty. Conclusion: Radiation injury and advanced pelvic malignancies were two most common causes of RVF in this study. Fecal diversion can be either initial operation or definite treatment in most patients with RVF. -

Influenza Del Tipo Di Vinificatore Sulla Qualità Del Vino Dolcetto D'ovada
L’ENOLOGO ❏ LUGLIO/AGOSTO 2003 DOCUMENTO TECNICO Maria Carla Cravero Cristina Ponte Federica Bonello Da sinistra: M. Loredana Serpentino C. Ponte, Rocco Di Stefano M.C. Cravero, Istituto Sperimentale per F. Bonello, l’Enologia - Asti M.L. Serpentino INFLUENZA DEL TIPO DI VINIFICATORE SULLA QUALITÀ DEL VINO DOLCETTO D’OVADA Tre diversi sistemi di gestione della macerazione sono stati adottati nella vinificazione di uve Dolcetto della zona di Ovada. L’elevato livello di maturità delle uve ha indotto modeste differenze compositive e sensoriali fra i vini prodotti. Il tipo di vinificatore, tuttavia, ha condizionato l’evoluzione del gusto e dell’aroma dei vini. coside, meno sensibile alle prevalenza delle molecole Introduzione polifenol ossidasi (PPO) del- acetate rispetto alle cinnama- Il vitigno Dolcetto, come il le altre antocianine. Le bucce te. Le uve Barbera, oltre ad Barbera, il Nebbiolo, il Gri- ed i vinaccioli sono ricchi di essere poco astringenti, pos- gnolino, il Freisa - per citar- tannini facilmente estraibili siedono tannini difficilmente ne solo alcuni - è tipico delle in una comune vinificazione. estraibili e, per produrre da zone vitivinicole del Piemon- Tra i vitigni citati preceden- esse vini dotati di una discre- te dove, grazie alla sua pre- temente, il Barbera possiede ta tannicità, occorre conse- cocità, può raggiungere la antociani a prevalenza di guire livelli di maturità parti- piena maturazione, anche in molecole trisostituite, ma colarmente spinti. Nebbiolo, annate sfavorevoli. Gli anto- con percentuali importanti -
High Resolution Anoscopy Overview
High Resolution Anoscopy Overview Naomi Jay, RN, NP, PhD University of California San Francisco Email: [email protected] Disclosures No Disclosures Definition of HRA Examination of the anus, anal canal and perianus using a colposcope with 5% acetic acid and Lugol’s solution. Basic Principles • Office-based procedure • Adapted from gynecologic colposcopy. • Validated for anal canal. • Similar terminology and descriptors. may be unfamiliar to non-gyn providers. • Comparable to vaginal and vulvar colposcopy. • Clinicians familiar with cervical colposcopy may be surprised by the difficult transition. Anal SCJ & AnTZ • Original vs. current SCJ less relevant. • TZ features less common, therefore more difficult to appreciate. • SCJ more subtle, difficult to see in entirety requires more manipulation & acetic acid. • Larger area of metaplastic changes overlying columnar epithelium compared to endocervix. • Most lesions found in the AnTZ. Atypical Metaplasia • Atypical metaplasia may indicate the presence of HSIL. • Radiate over distal rectum from SCJ. • Thin, may wipe off. • Features to look for indicating potential lesions: • Atypical clustered glands (ACG) • Lacy metaplastic borders (LM) • Epithelial Honeycombing (EH) Lugol’s. Staining • More utility in anus compared to cervix. • Adjunctive to help define borders, distinguish between possible LSIL/HSIL. • Most HSIL will be Lugol’s negative • LSIL may be Lugol’s partial or negative • Applied focally with small cotton swabs to better define an acetowhite lesion. •NOT a short cut to determine presence or absence of lesions, acetic acid is used first and is applied frequently. Anal vs. Cervical Characteristics • Punctation & Mosaic rarely “fine” mostly “coarse”. • Mosaic pattern mostly associated with HSIL. • Atypical vessels may be HSIL or cancer • Epithelial honeycombing & lacy metaplasia unique anal descriptors. -
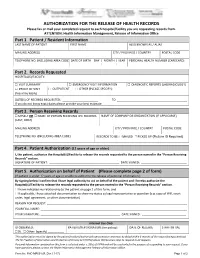
AUTHORIZATION for the RELEASE of HEALTH RECORDS Please Fax Or Mail Your Completed Request to Each Hospital/Facility You Are Requesting Records From
AUTHORIZATION FOR THE RELEASE OF HEALTH RECORDS Please fax or mail your completed request to each hospital/facility you are requesting records from. ATTENTION: Health Information Management, Release of Information Office Part 1. Patient / Resident Information LAST NAME OF PATIENT FIRST NAME ALSO KNOWN AS / ALIAS MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) DATE OF BIRTH DAY | MONTH | YEAR PERSONAL HEALTH NUMBER (CARECARD) | | Part 2. Records Requested HOSPITAL(S)/FACILITY: □ VISIT SUMMARY □ EMERGENCY VISIT INFORMATION □ DIAGNOSTIC REPORTS (LAB/RADIOLOGY) □ PROOF OF VISIT □ OUTPATIENT □ OTHER (PLEASE SPECIFY): (fees may apply) DATE(S) OF RECORDS REQUESTED: ______________________ TO ___________________________________________ If you do not know exact dates please provide your best estimate Part 3. Person Receiving Records □ MYSELF OR □ NAME OF PERSON RECEIVING THE RECORDS NAME OF COMPANY OR ORGANIZATION (IF APPLICABLE) (LAST, FIRST) MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) RECORDS TO BE: □ MAILED □ PICKED UP (Picture ID Required) Part 4. Patient Authorization (12 years of age or older) I, the patient, authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. SIGNATURE OF PATIENT: ___________________________________________ DATE SIGNED: ____________________________ Part 5. Authorization on behalf of Patient (Please complete page 2 of form) (If patient is under 12 years of age or unable to authorize the release of personal information.) By signing below I confirm that I have legal authority to act on behalf of the patient and I hereby authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. -

DOC Dolcetto Di Ovada
DISCIPLINARE DI PRODUZIONE DELLA DENOMINAZIONE DI ORIGINE CONTROLLATA “DOLCETTO DI OVADA” Approvato con DPR 01.09.72 GU 311 - 30.11.72 Modificato con DM 17.09.08 GU 229 - 30.09.08 Modificato con DM 30.11.2011 Pubblicato sul sito ufficiale del Mipaaf Sezione Qualità e Sicurezza Vini DOP e IGP Articolo 1 Denominazione 1.La denominazione di origine controllata ”Dolcetto di Ovada” è riservata al vino rosso che risponde alle condizioni ed ai requisiti prescritti dal presente disciplinare di produzione: Articolo 2 Base ampelografica 1.Il vino a denominazione di origine controllata “Dolcetto di Ovada” deve essere ottenuto dalle uve provenienti da vigneti aventi in ambito aziendale la seguente composizione ampelografica: Dolcetto al 100%. Tuttavia è consentito che nell’ambito dei vigneti siano presenti, fino ad un massimo del 3%, i vitigni non aromatici idonei alla coltivazione dalla Regione Piemonte. Articolo 3 Zona di produzione delle uve 1.La zona di produzione delle uve atte alla produzione del vino a denominazione di origine controllata “Dolcetto di Ovada” comprende l’intero territorio dei seguenti comuni : Ovada, Belforte Monferrato, Bosio, Capriata d'Orba, Carpeneto, Casaleggio Boiro, Cassinelle, Castelletto d'Orba, Cremolino, Lerma, Molare, Montaldeo, Montaldo Bormida, Mornese, Morsasco, Parodi Ligure, Prasco, Rocca Grimalda, San Cristoforo, Silvano d'Orba, Tagliolo Monferrato, Trisobbio. Articolo 4 Norme per la viticoltura 1. Le condizioni ambientali e di coltura dei vigneti destinati alla produzione del vino a denominazione di origine controllata “Dolcetto di Ovada” devono essere quelle tradizionali della zona e comunque atte a conferire alle uve e al vino derivato le specifiche caratteristiche di qualità' previste dal presente disciplinare. -

Episodio Di Benedicta Bosio 06.04.1944 I.Storia
EPISODIO DI BENEDICTA BOSIO 06.04.1944 Nome del compilatore: BARBARA BERRUTI E PAOLO CARREGA I.STORIA Località Comune Provincia Regione Benedicta Bosio Alessandria Piemonte Data iniziale: 6 aprile 1944 Data finale: 7 aprile 1944 Vittime decedute: Totale U Bam Ragazz i Adult Anzia s.i. D. Bambi Ragazze Adult Anzian S. Ign bini (12 i ni (più ne (0- (12-16) e e (più i (011) - (1755) 55) 11) (1755) 55) 16) 95 95 1 94 Di cui Civili Partigiani Renitenti Disertori Carabinieri Militari Sbandati 95 Prigionieri Antifascisti Sacerdoti e Ebrei Legati a Indefinito di guerra religiosi partigiani Elenco delle vittime decedute: 1. Alice Agostino Antonio, Gavi Ligure, 15 febbraio 1923, studente 2. Allegro Luigi, Serravalle Scrivia, 21 marzo 1920, elettrotecnico 3. Badalacco Luigi Adamo, Cabella Ligure, 25 febbraio 1923, meccanico 4. Badino Giuseppe, Genova Mignanego, 13 ottobre 1925, studente 5. Bagnasco Benedetto, Voltaggio, 5 maggio 1924, contadino 6. Baracchi Elio Luigi, Genova Sampierdarena, 13 luglio 1924 7. Barbieri Giulio, Novi Ligure, 29 ottobre 1923, studente 8. Barbieri Tullio Giambattista, San Quirico (GE), 24 aprile 1924 9. Barisone Natale, Arquata Scrivia, 17 novembre 1923, manovale 10. Benasso Pietrino Carlo, Genova, 8 agosto 1923, operaio 11. Berti Francesco Angelo 12. Bianchini Ferruccio, Genova, 7 luglio 1925, contadino 13. Biava Angelo, Malvino di Sardigliano, 30 luglio 1922, contadino 14. Bisio Luigi, Tassarolo, 12 aprile 1923, muratore e operaio 15. Bonelli Arturo, Genova, 11 dicembre 1924, operaio 16. Briata Giuseppe, Lerma, 28 gennaio 1925, macellaio e contadino 17. Bricola Mario Enrico Antonio, Grosseto, 11 aprile 1923, operaio 18. Bricola Pio, Gavi Ligure, 21 marzo 1925 19. -

Perforation Due to a Rectal Foreign Body and Radiological Findings
Case Report Ann Colorectal Res 2021;9(1):44-46. Perforation Due to a Rectal Foreign Body and Radiological Findings Saim Turkoglu1, MD; Adem Yokuş2, MD; Fırat Aslan3, MD 1Van Traınıng and Research Hospıtal, Van, Turkey 2Department of Radiology, Medical Faculty, Yuzuncu Yıl University, Van, Turkey 3Department of General Surgery, Medical Faculty, Yuzuncu Yıl University, Van, Turkey *Corresponding authors: Received: 01-03-2021 Saim Turkoglu, Van Traınıng and Research Hospıtal, Van,Turkey Revised: 03-04-2021 Tel: +90 5356452865; Fax: +90 432 2150471 Accepted: 05-04-2021 Email: [email protected] Abstract Introduction: Rectal foreign bodies have been increasingly seen and cause urgent surgical complications. Diagnosis and treatment of these cases in emergency departments may be difficult. The effective use of radiological imaging techniques can accelerate and facilitate this process. Case Presentation: A 65-year-old male patient, who underwent computed tomography (CT) with the suspicion of a foreign body in the rectum, was admitted to the emergency outpatient clinic. The patient was a male with a psychiatric illness who later underwent emergency surgery. Since the patient had impaired consciousness during the examination, anamnesis could not be obtained, so the initial impression upon surgical consultation was perforation due to rectal tumoral thickening. In almost all cases, plain radiography is sufficient and can eliminate diagnostic difficulties. However, this is not possible for non-opaque objects. Therefore, the CT scan played an important role in the diagnosis of this patient. A 30 cm foreign body, identified as salami, was removed from the abdomen of the patient, who was later taken for emergency surgery. -

Lower Gastrointestinal Tract
Lower Gastrointestinal Tract Hemorrhoids—Office Management and Review for Gastroenterologists Mitchel Guttenplan, MD, FACS 1 and Robert A Ganz, MD, FASGE 2 1. Medical Director, CRH Medical Corp; 2. Minnesota Gastroenterology, Chief of Gastroenterology, Abbott-Northwestern Hospital, Associate Professor of Medicine, University of Minnesota Abstract symptomatic hemorrhoids and anal fissures are very common problems. This article provides a review of the anatomy and physiology of the anorectum along with a discussion of the diagnosis and treatment of hemorrhoids and the commonly associated matters of anal sphincter spasm and fissures. The various office treatment modalities for hemorrhoids are discussed, as are the specifics of rubber band ligation (rBL), and a strategy for the office treatment of these problems by the gastroenterologist is given. The crh o’regan system™ is a technology available to the gastroenterologist that provides a safe, effective, and efficient option for the non-surgical treatment of hemorrhoids in the office setting. Keywords hemorrhoids, anal fissure, rubber band ligation, crh o’regan system™ Disclosure: Mitchel guttenplan is Medical Director of crh Medical Products corporation, the manufacturer of the crh o’regan system™. robert A ganz is a consultant to and holds equity in crh Medical Products corporation. Received: 2 november 2011 Accepted: 30 november 2011 Citation: Touchgastroentorology.com ; December, 2011. Correspondence: Mitchel guttenplan, MD, fAcs, 3000 old Alabama rd, suite 119 #183, Alpharetta, gA 30022-8555, us. e: [email protected] Diseases of the anorectum, including hemorrhoids and anal fissures, are experience also makes it clear that hemorrhoid sufferers frequently very common. The care of these entities is typically left to general and have additional anorectal issues that may both confuse the diagnosis colorectal surgeons. -

Adherence to Surveillance Guidelines Following Colonic Polypectomy Is Abysmal
170 Original Article Adherence to surveillance guidelines following colonic polypectomy is abysmal Frederick H. Koh1, Dedrick K. H. Chan1,2, Jingyu Ng3, Ker-Kan Tan1,2 1Division of Colorectal Surgery, University Surgical Cluster, National University Hospital, National University Health Systems, Singapore, Singapore; 2Department of Surgery, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore; 3Division of Colorectal Surgery, Department of General Surgery, Ng Teng Fong General Hospital, Singapore, Singapore Contributions: (I) Conception and design: FH Koh, KK Tan; (II) Administrative support: All authors; (III) Provision of study materials or patients: All authors; (IV) Collection and assembly of data: FH Koh, DK Chan, J Ng; (V) Data analysis and interpretation: FH Koh, DK Chan, J Ng; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Ker-Kan Tan. Division of Colorectal Surgery, University Surgical Cluster, National University Health System, 1E Kent Ridge Road, Singapore 119228, Singapore. Email: [email protected]. Background: Surveillance guidelines following excision of colonic tubular adenomas are well established. However, adherence to the guidelines are rarely audited. The aim of our study was to evaluate the rate of compliance to the recommended guidelines following polyp removal. Methods: A review of a prospectively collected colonoscopy database in a single tertiary institution was conducted for all patients who underwent polypectomy in 2008. We excluded patients who were diagnosed with or had prior history of colorectal malignancy. The frequency of subsequent colonoscopic were evaluated against the recommended guidelines based on the clinico-histological characteristics of the removed polyps. Results: There were 419 colonoscopies with polypectomies performed in 2008.