Thoracic Wall,Pleura & Lungs
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Part 1 the Thorax ECA1 7/18/06 6:30 PM Page 2 ECA1 7/18/06 6:30 PM Page 3
ECA1 7/18/06 6:30 PM Page 1 Part 1 The Thorax ECA1 7/18/06 6:30 PM Page 2 ECA1 7/18/06 6:30 PM Page 3 Surface anatomy and surface markings The experienced clinician spends much of his working life relating the surface anatomy of his patients to their deep structures (Fig. 1; see also Figs. 11 and 22). The following bony prominences can usually be palpated in the living subject (corresponding vertebral levels are given in brackets): •◊◊superior angle of the scapula (T2); •◊◊upper border of the manubrium sterni, the suprasternal notch (T2/3); •◊◊spine of the scapula (T3); •◊◊sternal angle (of Louis) — the transverse ridge at the manubrio-sternal junction (T4/5); •◊◊inferior angle of scapula (T8); •◊◊xiphisternal joint (T9); •◊◊lowest part of costal margin—10th rib (the subcostal line passes through L3). Note from Fig. 1 that the manubrium corresponds to the 3rd and 4th thoracic vertebrae and overlies the aortic arch, and that the sternum corre- sponds to the 5th to 8th vertebrae and neatly overlies the heart. Since the 1st and 12th ribs are difficult to feel, the ribs should be enu- merated from the 2nd costal cartilage, which articulates with the sternum at the angle of Louis. The spinous processes of all the thoracic vertebrae can be palpated in the midline posteriorly, but it should be remembered that the first spinous process that can be felt is that of C7 (the vertebra prominens). The position of the nipple varies considerably in the female, but in the male it usually lies in the 4th intercostal space about 4in (10cm) from the midline. -

Six Steps to the “Perfect” Lip Deborah S
September 2012 1081 Volume 11 • Issue 9 Copyright © 2012 ORIGINAL ARTICLES Journal of Drugs in Dermatology SPECIAL TOPIC Six Steps to the “Perfect” Lip Deborah S. Sarnoff MD FAAD FACPa and Robert H. Gotkin MD FACSb,c aRonald O. Perelman Department of Dermatology, New York University School of Medicine, New York, NY bLenox Hill Hospital—Manhattan Eye, Ear & Throat Institute, New York, NY cNorth Shore—LIJ Health Systems, Manhasset, NY ABSTRACT Full lips have always been associated with youth and beauty. Because of this, lip enhancement is one of the most frequently re- quested procedures in a cosmetic practice. For novice injectors, we recommend hyaluronic acid (HA) as the filler of choice. There is no skin test required; it is an easily obtainable, “off-the-shelf” product that is natural feeling when skillfully implanted in the soft tissues. Hyaluronic acid is easily reversible with hyaluronidase and, therefore, has an excellent safety profile. While Restylane® is the only FDA-approved HA filler with a specific indication for lip augmentation, one can use the following HA products off-label: Juvéderm® Ultra, Juvéderm Ultra Plus, Juvéderm Ultra XC, Juvéderm Ultra PLUS XC, Restylane-L®, Perlane®, Perlane-L®, and Belotero®. We present our six steps to achieve aesthetically pleasing augmented lips. While there is no single prescription for a “perfect” lip, nor a “one size fits all” approach for lip augmentation, these 6 steps can be used as a basic template for achieving a natural look. For more comprehensive, global perioral rejuvenation, our 6-step technique can be combined with the injection of neuromodulating agents and fractional laser skin resurfacing during the same treatment session. -

THORAX ANATOMY LAB 1: LEARNING OBJECTIVES Thoracic Wall, Pleural Cavities, and Lungs
THORAX ANATOMY LAB 1: LEARNING OBJECTIVES Thoracic Wall, Pleural Cavities, and Lungs Primary Learning Objectives 1. Define thorax and state the structures that form its anatomical boundaries. 2. Describe the locations and boundaries of the superior thoracic aperture (clinical: thoracic outlet) and the inferior thoracic aperture. Identify the costal arch (margin) and state the ribs that form the arch. 3. Identify and palpate the bones that compose the sternum (manubrium, body, and xiphoid process) and associated osteological features: jugular notch, clavicular notch, and sternal angle. 4. For the sternal angle, identify its associated vertebral level, state its anatomical relationship to the trachea and aorta, state its significance in creating an anatomical division of the mediastinum, and identify the ribs that join the sternum at its location. 5. Identify and palpate the clavicle, sternum, ribs, costal cartilages, intercostal spaces, and thoracic vertebrae. 6. Differentiate true ribs from false and floating ribs. 7. Identify the following osseous features on a rib: head, necK, rib (costal) tubercle, body, shaft, and the costal groove. 8. State the weaKest region of the rib that is commonly fractured and describe the anatomy and physiology involving flail chest. 9. Describe the possible clinical manifestations of supernumerary ribs. 10. Identify the following rib joints: costovertebral (costotransverse joint and vertebral body joint) and sternocostal. 11. Identify the transversus thoracis muscle, the external, internal, and innermost intercostal muscles, and state their innervation, blood supply, and functions. 12. State the structures that compose the neurovascular bundle within each intercostal space and identify each neurovascular bundle by number. 13. Identify the neurovascular bundle inferior to the twelfth rib and state the names of each structure composing the bundle (subcostal artery, subcostal vein, and subcostal nerve). -

E Pleura and Lungs
Bailey & Love · Essential Clinical Anatomy · Bailey & Love · Essential Clinical Anatomy Essential Clinical Anatomy · Bailey & Love · Essential Clinical Anatomy · Bailey & Love Bailey & Love · Essential Clinical Anatomy · Bailey & Love · EssentialChapter Clinical4 Anatomy e pleura and lungs • The pleura ............................................................................63 • MCQs .....................................................................................75 • The lungs .............................................................................64 • USMLE MCQs ....................................................................77 • Lymphatic drainage of the thorax ..............................70 • EMQs ......................................................................................77 • Autonomic nervous system ...........................................71 • Applied questions .............................................................78 THE PLEURA reections pass laterally behind the costal margin to reach the 8th rib in the midclavicular line and the 10th rib in the The pleura is a broelastic serous membrane lined by squa- midaxillary line, and along the 12th rib and the paravertebral mous epithelium forming a sac on each side of the chest. Each line (lying over the tips of the transverse processes, about 3 pleural sac is a closed cavity invaginated by a lung. Parietal cm from the midline). pleura lines the chest wall, and visceral (pulmonary) pleura Visceral pleura has no pain bres, but the parietal pleura covers -

Variations in Dimensions and Shape of Thoracic Cage with Aging: an Anatomical Review
REVIEW ARTICLE Anatomy Journal of Africa, 2014; 3 (2): 346 – 355 VARIATIONS IN DIMENSIONS AND SHAPE OF THORACIC CAGE WITH AGING: AN ANATOMICAL REVIEW ALLWYN JOSHUA, LATHIKA SHETTY, VIDYASHAMBHAVA PARE Correspondence author: S.Allwyn Joshua, Department of Anatomy, KVG Medical College, Sullia- 574327 DK, Karnataka,India. Email: [email protected]. Phone number; 09986380713. Fax number – 08257233408 ABSTRACT The thoracic cage variations in dimensions and proportions are influenced by age, sex and race. The objective of the present review was to describe the age related changes occurring in thoracic wall and its influence on the pattern of respiration in infants, adult and elderly. We had systematically reviewed, compared and analysed many original and review articles related to aging changes in chest wall images and with the aid of radiological findings recorded in a span of four years. We have concluded that alterations in the geometric dimensions of thoracic wall, change in the pattern and mechanism of respiration are influenced not only due to change in the inclination of the rib, curvature of the vertebral column even the position of the sternum plays a pivotal role. Awareness of basic anatomical changes in thoracic wall and respiratory physiology with aging would help clinicians in better understanding, interpretation and to differentiate between normal aging and chest wall deformation. Key words: Thoracic wall; Respiration; Ribs; Sternum; vertebral column INTRODUCTION The thoracic skeleton is an osteocartilaginous cage movement to the volume displacement of the frame around the principal organs of respiration lungs was evaluated by (Agostoni et al,m 1965; and circulation. It is narrow above and broad Grimby et al., 1968; Loring, 1982) for various below, flattened antero-posteriorly and longer human body postures. -

Surface and Regional Anatomy 297
Van De Graaff: Human IV. Support and Movement 10. Surface and Regional © The McGraw−Hill Anatomy, Sixth Edition Anatomy Companies, 2001 Surface and Regional 10 Anatomy Introduction to Surface Anatomy 297 Surface Anatomy of the Newborn 298 Head 300 Neck 306 Trunk 309 Pelvis and Perineum 318 Shoulder and Upper Extremity 319 Buttock and Lower Extremity 326 CLINICAL CONSIDERATIONS 330 Clinical Case Study Answer 339 Chapter Summary 340 Review Activities 341 Clinical Case Study A 27-year-old female is brought to the emergency room following a motor vehicle accident. You examine the patient and find her to be alert but pale and sweaty, with breathing that is rapid and shallow. You see that she has distension of her right internal jugular vein visible to the jaw and neck. Her trachea is deviated 3 cm to the right of midline. She has tender contu- sions on her left anterior chest wall with minimal active bleeding over one of the ribs. During the brief period of your examination, the patient exhibits more respiratory distress, and her blood pressure begins to drop. You urgently insert a large-gauge needle into her left hemitho- rax and withdraw 20 cc of air. This results in immediate improvement in the patient’s breath- ing and blood pressure. Why does the patient have a distended internal jugular vein on the right side of her neck? Could this be related to a rapid drop in blood pressure? What is the clinical situation of this patient? Hint: As you read this chapter, note that knowledge of normal surface anatomy is vital to the FIGURE: In order to effectively administer medical treatment, it is imperative for a recognition of abnormal surface anatomy, and that the latter may be an easy clue to the pathol- physician to know the surface anatomy of each ogy lying deep within the body. -

Thoracic Wall Foreign Bodies Following Penetrating Trauma in Pediatric Age Group: Report of Two Cases with Literature Review
CASE REPORT East J Med 25(1): 173-176, 2020 DOI: 10.5505/ejm.2020.68094 Thoracic Wall Foreign Bodies Following Penetrating Trauma In Pediatric Age Group: Report of Two Cases With Literature Review Volkan Sarper Erikci Department of Pediatric Surgery, Sağlık Bilimleri University Tepecik Training Hospital, Izmir, Turkey ABSTRACT Penetrating chest trauma is rarely seen in childhood. Following penetrative trauma various foreign objects may be detected as embedded in the tissues. A precise and prompt diagnosis together with an appropriate surgical management is paramount in these cases for a good prognosis. Here we present 2 cases with 2 different foreign bodies embedded in thoracic wall following different penetrating thoracic traumas. The purpose this report to critique the properties and handling of penetrative chest wall trauma in children with regard to post-traumatic retained FBs in thoracic wall and the topic is discussed under the light of relevant literature. Key Words: Chest wall trauma-retained foreign body-children Introduction cartridge bullet (Figure 1). There were not any findings consistent with hemo-pneumothorax or Penetrating chest injury may pose difficulty in pulmonary parenchymal injury in imaging studies like diagnosis of these cases for the health provider. chest roentgenogram and computed tomography. An Foreign bodies (FB) in thoracic wall after a easily palpable radiopaque FB was observed in the left penetrative injury are scarcely seen in childhood. hemithoracic wall adjacent to thoracic vertebrae There is a wide spectrum of foreign objects retained (Figure 2). Under general anesthesia during surgical in thorax following a trauma and these include bullets, intervention a midline rigid object was palpated 5 cm shrapnel, a piece of wearing, bones, rib particles and medial and away from to the wound. -

Unit #2 - Abdomen, Pelvis and Perineum
UNIT #2 - ABDOMEN, PELVIS AND PERINEUM 1 UNIT #2 - ABDOMEN, PELVIS AND PERINEUM Reading Gray’s Anatomy for Students (GAFS), Chapters 4-5 Gray’s Dissection Guide for Human Anatomy (GDGHA), Labs 10-17 Unit #2- Abdomen, Pelvis, and Perineum G08- Overview of the Abdomen and Anterior Abdominal Wall (Dr. Albertine) G09A- Peritoneum, GI System Overview and Foregut (Dr. Albertine) G09B- Arteries, Veins, and Lymphatics of the GI System (Dr. Albertine) G10A- Midgut and Hindgut (Dr. Albertine) G10B- Innervation of the GI Tract and Osteology of the Pelvis (Dr. Albertine) G11- Posterior Abdominal Wall (Dr. Albertine) G12- Gluteal Region, Perineum Related to the Ischioanal Fossa (Dr. Albertine) G13- Urogenital Triangle (Dr. Albertine) G14A- Female Reproductive System (Dr. Albertine) G14B- Male Reproductive System (Dr. Albertine) 2 G08: Overview of the Abdomen and Anterior Abdominal Wall (Dr. Albertine) At the end of this lecture, students should be able to master the following: 1) Overview a) Identify the functions of the anterior abdominal wall b) Describe the boundaries of the anterior abdominal wall 2) Surface Anatomy a) Locate and describe the following surface landmarks: xiphoid process, costal margin, 9th costal cartilage, iliac crest, pubic tubercle, umbilicus 3 3) Planes and Divisions a) Identify and describe the following planes of the abdomen: transpyloric, transumbilical, subcostal, transtu- bercular, and midclavicular b) Describe the 9 zones created by the subcostal, transtubercular, and midclavicular planes c) Describe the 4 quadrants created -

LATISSIMUS DORSI FLAP for HEAD and NECK RECONSTRUCTION Patrik Pipkorn, Ryan Jackson, Bruce Haughey
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY LATISSIMUS DORSI FLAP FOR HEAD AND NECK RECONSTRUCTION Patrik Pipkorn, Ryan Jackson, Bruce Haughey The latissimus dorsi is the largest muscle in Benefits the body by surface area. It can be as large as 20 x 40cms, enabling latissimus dorsi • Easy flap to learn to harvest flaps to cover very large defects (Figure 1). • Large thin muscle that can cover very large defects • Long (5-15cm) vascular pedicle if dis- sected up to the subscapular artery • The subscapular artery has a diameter of 2-5mm • Minimal long-term donor site morbidity • Can be harvested as a muscle flap or with a skin paddle • Can be harvested as a chimeric flap (multiple otherwise independent flaps that each have an independent vascular supply with all pedicles linked to a common source vessel) along with other flaps based on a singular subscapular artery Caveats • Donor site is close to head and neck area making two team harvest difficult, though not impossible Figure 1: Large pedicled latissimus dorsi • Because the donor site is on the back, it flap makes positioning more tedious • Large wound and potential dead space The flap can be harvested as a pedicled or after harvest has high risk of a seroma free flap and as a muscular or myocuta- neous flap with an overlying skin paddle. It can also be harvested along with any other Surgical anatomy flap based on the subscapular vascular system as a chimeric or subscapular “mega- The latissimus dorsi mainly adducts and flap”. Despite its size it can be harvested medially rotates the arm. -

Surface Anatomy
BODY ORIENTATION OUTLINE 13.1 A Regional Approach to Surface Anatomy 398 13.2 Head Region 398 13.2a Cranium 399 13 13.2b Face 399 13.3 Neck Region 399 13.4 Trunk Region 401 13.4a Thorax 401 Surface 13.4b Abdominopelvic Region 403 13.4c Back 404 13.5 Shoulder and Upper Limb Region 405 13.5a Shoulder 405 Anatomy 13.5b Axilla 405 13.5c Arm 405 13.5d Forearm 406 13.5e Hand 406 13.6 Lower Limb Region 408 13.6a Gluteal Region 408 13.6b Thigh 408 13.6c Leg 409 13.6d Foot 411 MODULE 1: BODY ORIENTATION mck78097_ch13_397-414.indd 397 2/14/11 3:28 PM 398 Chapter Thirteen Surface Anatomy magine this scenario: An unconscious patient has been brought Health-care professionals rely on four techniques when I to the emergency room. Although the patient cannot tell the ER examining surface anatomy. Using visual inspection, they directly physician what is wrong or “where it hurts,” the doctor can assess observe the structure and markings of surface features. Through some of the injuries by observing surface anatomy, including: palpation (pal-pā sh ́ ŭ n) (feeling with firm pressure or perceiving by the sense of touch), they precisely locate and identify anatomic ■ Locating pulse points to determine the patient’s heart rate and features under the skin. Using percussion (per-kush ̆ ́ŭn), they tap pulse strength firmly on specific body sites to detect resonating vibrations. And ■ Palpating the bones under the skin to determine if a via auscultation (aws-ku ̆l-tā sh ́ un), ̆ they listen to sounds emitted fracture has occurred from organs. -
Anatomy of the Abdomen, Pelvis & Retroperitoneal Structures
Anatomy of the Abdomen, Pelvis & Retroperitoneal Structures Outline z Abdomen z Layers, muscles and organs z Innervation of abdominal organs z Retroperitoneum z Structures and innervation z Pelvic Organs and innervation Abdomen Surface Anatomy of Abdomen z Umbilicus z Linea alba = white line z Xiphoid process to pubic symphysis z Tendinous line z Inferior Boundaries z Iliac crest z Ant. Sup. Iliac spine z Inguinal ligament z Pubic crest z Superior Boundary z Diaphragm Abdominal wall Layers of abdominal wall z Fatty superficial layer - Camper’s fascia z Membranous deep layer - Scarpa’s fascia z Deep Fascial z External oblique muscle z Internal oblique muscle z Transverse abdominal muscle z Transversalis fascia z Parietal Peritoneum Muscles of Anterior Abdominal Wall z External Obliques z O: lower 8 ribs I: aponeurosis to linea alba z Function: Flex trunk, compress abd. wall (together) Rotate trunk (separate sides) z Internal Obliques z O: Lumbar fascia, iliac crest, inguinal ligament z I: Linea alba, pubic crest, last 3-4 ribs, costal margin z Function: Same as External obliques z Transversus Abdominis z O:same as Internals, plus last 6 ribs z I: Xiphoid process, costal cart. 5-7 z Function: Compress abdomen z Rectus Abdominis z O: Pubic crest, pubic symphysis I: Xiphoid, cost cart 5-7 z Function: Flex, rotate trunk, compress abdomen, fix ribs Peritoneum z Extension of serous membrane in the abdomino-pelvic cavity z Mesentery: Double layer of peritoneum z Hold organs in place z Store fat z Route for vessels + nerves z Retroperitoneal: some -
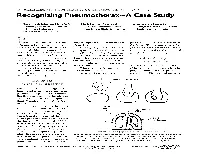
Recognizing Pneumothorax-A Case Study
Recognizing Pneumothorax-A Case Study Mary Black Johnson, PhD, ATC Mark Haines, MA, ATC Brian Barry, MA, ATC Metropolitan State College Assistant Athletic Trainer The Jim Davis Connection Denver, Colorado San Diego State University Carlsbad, California 9%-neumothorax injuries are lung to expand fully within its own position and air is expired from infrequent but can be life threat- pleural sac. the lungs. The passive expiration ening. They are most often associ- During inspiration, the dia- process becomes active and is facili- ated with blunt trauma of the phragm contracts and flattens tated by contraction of abdominal chest. The trauma causes rib frac- while the ribs are lifted by contrac- and chest muscles during exercise. ture, which in turn perforates the tion of the intercostal muscles. pleural wall. Thus, air or gas accu- Thus, the negative pressure in- 9njuw Changes mulates in the pleural cavity and creases, resulting in air flow from in Respiration causes the lung to collapse. It is the atmosphere into the increased critical to recognize the signs and area of the lungs. When the chest wall is pierced, in symptoms of this condition in or- When the muscles involved in either an open or closed chest in- der to provide prompt and suc- respiration relax, the diaphragm jury, normal pressure gradients cessful treatment in what can be a returns to its dome-shaped resting are altered. The normal pressure medical emergency. , fluid-filled balloon Dynamics 1 , of Normal Breathing Within the thoracic cage, each lung resides in a separate com- partment, the pleural sac. Between the thoracic wall and the pleural sac is a thin layer of intrapleural fluid (Vander et al., 1985) (Fig- ure 1).