From Annual Wellness Visit to Adrenalectomy!
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ACTH Stimulation Tests for the Diagnosis of Adrenal Insufficiency: Systematic Review and Meta-Analysis
ORIGINAL ARTICLE ACTH Stimulation Tests for the Diagnosis of Adrenal Insufficiency: Systematic Review and Meta-Analysis Naykky Singh Ospina,* Alaa Al Nofal,* Irina Bancos, Asma Javed, Khalid Benkhadra, Ekta Kapoor, Aida N. Lteif, Neena Natt, and M. Hassan Murad Evidence-Based Practice Research Program (N.S.O., A.A.N., K.B., M.H.M.), Mayo Clinic, Rochester, Downloaded from https://academic.oup.com/jcem/article/101/2/427/2810551 by guest on 29 September 2021 Minnesota; Knowledge and Evaluation Research Unit (N.S.O., K.B., M.H.M.), Mayo Clinic, Rochester, Minnesota; Division of Endocrinology, Diabetes, Metabolism, and Nutrition (N.S.O., N.N., I.B.), Mayo Clinic, Rochester, Minnesota; Division of Pediatric Endocrinology and Metabolism (A.A.N., A.J., A.N.L.), Mayo Clinic, Rochester, Minnesota; Division of General Internal Medicine (E.K.), Mayo Clinic, Rochester, Minnesota 55905 Context: The diagnosis of adrenal insufficiency is clinically challenging and often requires ACTH stimulation tests. Objective: To determine the diagnostic accuracy of the high- (250 mcg) and low- (1 mcg) dose ACTH stimulation tests in the diagnosis of adrenal insufficiency. Methods: We searched six databases through February 2014. Pairs of independent reviewers se- lected studies and appraised the risk of bias. Diagnostic association measures were pooled across studies using a bivariate model. Data Synthesis: For secondary adrenal insufficiency, we included 30 studies enrolling 1209 adults and 228 children. High- and low-dose ACTH stimulation tests had similar diagnostic accuracy in adults and children using different peak serum cortisol cutoffs. In general, both tests had low sensitivity and high specificity resulting in reasonable likelihood ratios for a positive test (adults: high dose, 9.1; low dose, 5.9; children: high dose, 43.5; low dose, 7.7), but a fairly suboptimal likelihood ratio for a negative test (adults: high dose, 0.39; low dose, 0.19; children: high dose, 0.65; low dose, 0.34). -

SNAP Cortisol Testing Guide
SNAP® Cortisol Testing Guide Diagnosing and Treating Cases of Suspected Canine Hyperadrenocorticism or Addison’s Disease IMPORTANT: Review history of any administration of corticosteroids as these may influence the reported results. Diagnose ACTH Stimulation Test Diagnostic Protocol for Cases of Suspected Canine Hyperadrenocorticism or Addison’s Disease History, physical exam, CBC, chemistry panel, electrolytes and urinalysis consistent with Canine Hyperadrenocorticism or Addison’s disease Draw baseline cortisol sample. Perform an ACTH stimulation test with Cortrosyn® 5 µg/kg IV or ACTH gel 2.2 U/kg IM. Draw 1-hour cortisol (Cortrosyn®) or 1 and 2-hour cortisol (ACTH gel). Pre-ACTH: 2–6 µg/dL Pre- and Post-ACTH Post-ACTH Post-ACTH Post-ACTH 2 6 µg/dL >22 µg/dL <2 µg/dL – Post-ACTH: 6–18 µg/dL 18–22 µg/dL If both results are <2 µg/dL, results are Equivocal, Consistent Inconclusive consistent with Normal Cushing’s possible with Cushing’s hypoadrenocorticism Perform high-dose dexamethasone* Begin treatment with suppression to mineralocorticoid discriminate between and/or glucocorticoid PDH and ATH, as appropriate. ACTH level and/or abdominal ultrasound. * Do not exceed 0.1 mg/kg of dexamethasone. Diagnose Low-Dose Dexamethasone Suppression Protocol For Cases of Suspected Canine Hyperadrenocorticism History, physical exam, CBC, chemistry panel, electrolytes and urinalysis consistent with Canine Hyperadrenocorticism Draw baseline cortisol sample. Perform a low-dose dexamethasone suppression test with 0.01 mg/kg of dexamethasone IV. Draw 4-hour -
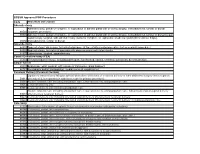
Code Procedure Description Adrenalectomy 60540 Adrenalectomy, Partial Or Complete, Or Exploration of Adrenal Gland with Or Witho
BCBSM Approved POP Procedures Code Procedure Description Adrenalectomy Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal 60540 (separate procedure) 60545 Adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, transabdominal, lumbar or dorsal (separate procedure); with excision of adjacent retroperitoneal tumor Laparoscopy, surgical, with adrenalectomy, partial or complete, or exploration of adrenal gland with or without biopsy, 60650 transabdominal, lumbar or dorsal Appendectomy 44955 Appendectomy; when done for indicated purpose at time of other major procedure (not as separate procedure) 44960 Appendectomy; for ruptured appendix with abscess or generalized peritonitis 44970 Laparoscopy, surgical, appendectomy Carotid Endarterectomy (CEA) 35301 Thromboendarterectomy, including patch graft, if performed; carotid, vertebral, subclavian, by neck incision Carpal Tunnel 29848 Endoscopy, wrist, surgical, with release of transverse carpal ligament 64721 Neuroplasty and/or transposition; median nerve at carpal tunnel Cesarean Delivery (Cesarean Section) Ligation or transection of fallopian tube(s) when done at the time of cesarean delivery or intra-abdominal surgery (not a separate 58611 procedure) (List separately in addition to code for primary procedure) 59510 Routine obstetric care including antepartum care, cesarean delivery, and postpartum care 59514 Cesarean delivery only 59515 Cesarean delivery only; including postpartum care -

Adrenalectomy Patient Information Leaflet
Adrenalectomy Patient information leaflet UHB is a no smoking Trust To see all of our current patient information leaflets please visit www.uhb.nhs.uk/patient-information-leaflets.htm What is an adrenalectomy? An adrenalectomy (ad-renal-ect-omy) is an operation to remove one or both of the adrenal glands. The adrenal glands sit above the kidneys. Right Left adrenal adrenal gland gland Kidney Kidney The main role of the adrenal glands is to release hormones into the body. The main hormones released are stress related hormones (cortisol, noradrenaline and adrenaline), hormones that regulate metabolism, hormones that affect immune system function, androgens (sex hormones) and hormones for saltwater balance (aldosterone). 2 | PI18/1289/03 Adrenalectomy An adrenalectomy can be done: • ‘Open’ with one large surgical cut below the ribcage • Or ‘laparoscopic’ which involves four smaller cuts being made allowing the inside of the abdomen to be seen using a camera Some laparoscopic operations may have be converted to ‘open’ at the time of the surgery due to the surgeon not being able to see the inside of the abdomen clearly enough (about 5% of cases). The surgery is performed under general anaesthetic so you will be asleep and will not feel any pain. The surgery normally takes 1–2 hours. The adrenal gland(s) will be sent to a pathologist after it is removed for further tests in a laboratory using a microscope. Why is an adrenalectomy performed? The adrenal gland(s) need to be removed if there is a mass/ tumour in the gland(s). An adrenalectomy is performed if: 1. -

Advances in Risk-Oriented Surgery for Multiple Endocrine Neoplasia Type 2
25 2 Endocrine-Related A Machens et al. Advances in risk-oriented 25:2 T41–T52 Cancer surgery for MEN2 THEMATIC REVIEW Advances in risk-oriented surgery for multiple endocrine neoplasia type 2 Andreas Machens1 and Henning Dralle2 1Department of General, Visceral and Vascular Surgery, Martin Luther University Halle-Wittenberg, Halle, Saale, Germany 2Department of General, Visceral and Transplantation Surgery, Section of Endocrine Surgery, University of Duisburg-Essen, Essen, Germany Correspondence should be addressed to A Machens: [email protected] This paper is part of a thematic review section on 25 Years of RET and MEN2. The guest editors for this section were Lois Mulligan and Frank Weber. Abstract Genetic association studies hinge on definite clinical case definitions of the disease of Key Words interest. This is why more penetrant mutations were overrepresented in early multiple f biochemical screening endocrine neoplasia type 2 (MEN2) studies, whereas less penetrant mutations went f DNA-based screening underrepresented. Enrichment of genetic association studies with advanced disease f RET proto-oncogene may produce a flawed understanding of disease evolution, precipitating far-reaching f gene test surgical strategies like bilateral total adrenalectomy and 4-gland parathyroidectomy in f gene carrier MEN2. The insight into the natural course of the disease gleaned over the past 25 years f multiple endocrine caused a paradigm shift in MEN2: from the removal of target organs at the expense of neoplasia type 2A greater operative -

Use of Dexmedetomidine in a Parturient with Multiple Endocrine Neoplasia Type 2A Undergoing Adrenalectomy and Thyroidectomy
PRACTICE CASE REPORT Use of Dexmedetomidine in a Parturient With Multiple Endocrine Neoplasia Type 2A Undergoing Adrenalectomy and Thyroidectomy: A Case Report Amanda L. Faulkner, MD, Eric Swanson, MD, Thomas L. McLarney, MD, Cortney Y. Lee, MD, and Annette Rebel, MD * * * † * 08/15/2018 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3yRlXg5VZA8uqNuqWFo8dRhJiNZRTFLkCeIa0nEMHM2KbYm37VRaE3A== by https://journals.lww.com/aacr from Downloaded Dexmedetomidine is a selective α2-agonist, frequently used in perioperative medicine as anes- thesia adjunct. The medication carries a Food and Drug Administration pregnancy category C Downloaded designation and is therefore rarely used for parturients undergoing nonobstetric surgery. We are reporting the use of dexmedetomidine in the anesthetic management of a parturient undergoing minimally invasive unilateral adrenalectomy for pheochromocytoma during the second trimester from https://journals.lww.com/aacr of pregnancy. Additionally, because of the multiple endocrine neoplasia type 2A constellation with diagnosis of medullary thyroid cancer, the patient underwent a total thyroidectomy 1 week after the adrenalectomy. (A&A Practice. XXX;XXX:00–00.) exmedetomidine is a selective α2-agonist, fre- CASE REPORT by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3yRlXg5VZA8uqNuqWFo8dRhJiNZRTFLkCeIa0nEMHM2KbYm37VRaE3A== quently used in perioperative medicine. It has A 34-year-old gravida 3 para 2 woman (body weight, 61 Dfound favor in this setting because of its sedative kg; -

Surgical Indications and Techniques for Adrenalectomy Review
THE MEDICAL BULLETIN OF SISLI ETFAL HOSPITAL DOI: 10.14744/SEMB.2019.05578 Med Bull Sisli Etfal Hosp 2020;54(1):8–22 Review Surgical Indications and Techniques for Adrenalectomy Mehmet Uludağ,1 Nurcihan Aygün,1 Adnan İşgör2 1Department of General Surgery, Sisli Hamidiye Etfal Training and Research Hospital, Istanbul, Turkey 2Department of General Surgery, Bahcesehir University Faculty of Medicine, Istanbul, Turkey Abstract Indications for adrenalectomy are malignancy suspicion or malignant tumors, non-functional tumors with the risk of malignancy and functional adrenal tumors. Regardless of the size of functional tumors, they have surgical indications. The hormone-secreting adrenal tumors in which adrenalectomy is indicated are as follows: Cushing’s syndrome, arises from hypersecretion of glucocorticoids produced in fasciculata adrenal cortex, Conn’s syndrome, arises from an hypersecretion of aldosterone produced by glomerulosa adrenal cortex, and Pheochromocytomas that arise from adrenal medulla and produce catecholamines. Sometimes, bilateral adre- nalectomy may be required in Cushing's disease due to pituitary or ectopic ACTH secretion. Adenomas arise from the reticularis layer of the adrenal cortex, which rarely releases too much adrenal androgen and estrogen, may also develop and have an indication for adrenalectomy. Adrenal surgery can be performed by laparoscopic or open technique. Today, laparoscopic adrenalectomy is the gold standard treatment in selected patients. Laparoscopic adrenalectomy can be performed transperitoneally or retroperitoneoscopi- cally. Both approaches have their advantages and disadvantages. In the selection of the surgery type, the experience and habits of the surgeon are also important, along with the patient’s characteristics. The most common type of surgery performed in the world is laparoscopic transabdominal lateral adrenalectomy, which most surgeons are more familiar with. -

Adrenal Incidentalomas with Supraphysiologic Response to ACTH Stimulus: a Case Report
Hindawi Publishing Corporation Case Reports in Endocrinology Volume 2012, Article ID 503290, 4 pages doi:10.1155/2012/503290 Case Report Adrenal Incidentalomas with Supraphysiologic Response to ACTH Stimulus: A Case Report Marianna Antonopoulou1 and Asya Perelstein2 1 SUNY Downstate Medical Center, 450 Clarkson Avenue, Box 1205, Brooklyn, NY 11203, USA 2 VA Medical Center, 800 Poly Place, New York, NY 11209, USA Correspondence should be addressed to Marianna Antonopoulou, [email protected] Received 7 August 2012; Accepted 20 September 2012 Academic Editors: I. Broom, C. Capella, and T. Konrad Copyright © 2012 M. Antonopoulou and A. Perelstein. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. We present the diagnostic approach of a patient with adrenal incidentalomas. A 72-year-old African American male had a CT scan of the abdomen showing right and left adrenal masses measuring 5 × 3.5 cm and 3.7 × 2.9 cm, respectively. The patient had negative hormonal workup. The radiologist insisted that the CT findings are consistent with adrenal hyperplasia, and therefore he underwent ACTH stimulation to rule out late-onset congenital adrenal hyperplasia (CAH). The stimulation test revealed that 17-hydroxyprogesterone and 11-deoxycortisol increased to levels high enough to confirm CAH, but cortisol had exaggerated response as well, thus making the diagnosis of CAH unlikely where metabolism is shifted to precursors. Subsequently, the patient underwent screening for Cushing’s syndrome (CS) with a dexamethasone suppression test. Patient failed the suppresion test, raising the issue for subclinical CS (SCS), likely due to ACTH-independent macronodular adrenal hyperplasia. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Poster Presentations
______________________________________ P1-d1-164 Adrenals and HPA Axis 1 Arterial hypertension in children: alterations in mineralocorticoid and glucocorticoid axis and their impact on pro-inflammatory, endothelial damage, and oxidative stress parameters Carmen Campino1; Rodrigo Bancalari2; Alejandro Martinez-Aguayo2; Poster Presentations Marlene Aglony2; Hernan Garcia2; Carolina Avalos2; Lilian Bolte2; Carolina Loureiro2; Cristian Carvajal1; Lorena Garcia3; Sergio Lavanderos3; Carlos Fardella1 1Pontificia Universidad Catolica, Endocrinology, and Millennium Institute of Immunology and Immunotherapy, Santiago, Chile; 2Pontificia Universidad Catolica, pediatrics, Santiago, Chile; 3Universidad de Chile, School of Chemical Sciences, Santiago, Chile Background and aims: The pathogenesis of arterial hypertension and its impact and determining factors with respect to cardiovascular damage in chil- dren is poorly understood. We evaluated the prevalence of alterations in the mineralocorticoid and glucocorticoid axes and their impact on pro-inflam- matory, endothelial damage and oxidative stress parameters in hypertensive children. Methods: 306 children (5-16 years old); Group 1: Hypertensives (n=111); Group 2: normotensives with hypertensive parents (n=101); Group 3: normotensives with normotensives parents (n= 95). Fasting blood samples were drawn for hormone measurements (aldosterone, plasma renin activity (PRA), cortisol (F), cortisone (E)); inflammation vari- ______________________________________ ables (hsRCP, adiponectin, IL-6, IL-8, TNF-α); endothelial damage (PAI-I, P1-d1-163 Adrenals and HPA Axis 1 MMP9 and MMP2 activities) and oxidative stress (malondialdehyde). Famil- The role of S-palmitoylation of human ial hyperaldosteronism type 1 (FH-1) was diagnosed when aldosterone/PRA ratio >10 was associated with the chimeric CYP11B1/CYP11B2 gene. The glucocorticoid receptor in mediating the non- 11β-HSD2 activity was considered altered when the F/E ratio exceeded the genomic actions of glucocorticoids mean + 2 SD with respect to group 3. -

What's New in End Ocrine Surgery?
What’s new in endocrine surgery? Endocrine surgery has become a well-defined part of general surgery. EUGENIO PANIERI, FCS(SA) Head, Oncology Endocrine Surgery, Department of Surgery, University of Cape Town Eugenio Panieri is a graduate of the University of Cape Town, and is Head of the Endocrine and Surgical Oncology Unit at Groote Schuur Hospital. His main areas of interest are in minimally access surgery for endocrine conditions, and the use of sentinel lymph node biopsy and immediate reconstruction in breast cancer. Endocrine surgery has steadily evolved from relative obscurity into a well-defined subdiscipline of general surgery. Success in this area relies on close co-operation with endocrinologists, radiologists, nuclear physicians, and pathologists. Endocrine surgeons have a pivotal role in the management of nodular thyroid disease and thyroid cancer, hyperparathyroidism, as well as functional adrenal and pancreatic tumours. Unlike other solid tumours, endocrine neoplasms make their presence known by systemic effects of excess hormone production, rather than by local symptoms related to tumour size or local invasion. As laboratory diagnostic methods and radiology imaging techniques have improved, so the demand for surgical expertise in this area has increased. Techniques of minimally invasive surgery have transformed the practice of general surgery. In some cases, such as cholecystectomy or anti-reflux surgery, laparoscopy has become the unquestioned standard of care; in others, such as hernia or colorectal surgery the debate continues. In this article I will describe the role such Fig. 1. CT scan of the abdomen illustrating a 7 cm phaeochromocytoma techniques have to play in the surgical management of endocrine in the left adrenal gland. -
Preoperative and Intraoperative Methods of Parathyroid Gland Localization and the Diagnosis of Parathyroid Adenomas
molecules Review Preoperative and Intraoperative Methods of Parathyroid Gland Localization and the Diagnosis of Parathyroid Adenomas Jacek Baj 1,*, Robert Sitarz 1,2 , Marek Łokaj 2, Alicja Forma 1 , Marcin Czeczelewski 3 , Amr Maani 1 and Gabriella Garruti 4 1 Chair and Department of Anatomy, Medical University of Lublin, 20-950 Lublin, Poland; [email protected] (R.S.); [email protected] (A.F.); [email protected] (A.M.) 2 Department of Surgery, Center of Oncology of the Lublin Region St. Jana z Dukli, 20-090 Lublin, Poland; [email protected] 3 Chair and Department of Forensic Medicine, Medical University of Lublin, 20-950 Lublin, Poland; [email protected] 4 Section of Endocrinology, Andrology and Metabolic Diseases, Department of Emergency and Organ Transplantations, University of Bari “Aldo Moro” Medical School, 70124 Bari, Italy; [email protected] * Correspondence: [email protected]; Tel.: +48-662-094-014 Received: 24 February 2020; Accepted: 8 April 2020; Published: 9 April 2020 Abstract: Accurate pre-operative determination of parathyroid glands localization is critical in the selection of minimally invasive parathyroidectomy as a surgical treatment approach in patients with primary hyperparathyroidism (PHPT). Its importance cannot be overemphasized as it helps to minimize the harmful side effects associated with damage to the parathyroid glands such as in hypocalcemia, severe hemorrhage or recurrent laryngeal nerve dysfunction. Preoperative and intraoperative methods decrease the incidence of mistakenly