Willingness and Status of Social Health Insurance Among People of Pokhara Lekhnath, Nepal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
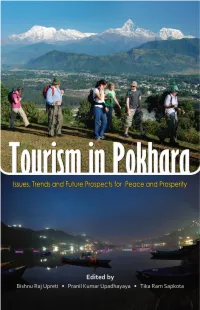
Tourism in Pokhara: Issues, Trends and Future Prospects for Peace and Prosperity
Tourism in Pokhara: Issues, Trends and Future Prospects for Peace and Prosperity 1 Tourism in Pokhara Issues, Trends and Future Prospects for Peace and Prosperity Edited by Bishnu Raj Upreti Pranil Kumar Upadhayaya Tikaram Sapkota Published by Pokhara Tourism Council, Pokhara South Asia Regional Coordination Office of NCCR North-South and Nepal Centre for Contemporary Research, Kathmandu Kathmandu 2013 Citation: Upreti BR, Upadhayaya PK, Sapkota T, editors. 2013. Tourism in Pokhara Issues, Trends and Future Prospects for Peace and Prosperity. Kathmandu: Pokhara Tourism Council (PTC), South Asia Regional Coordination Office of the Swiss National Centre of Competence in Research (NCCR North- South) and Nepal Center for Contemporary Research (NCCR), Kathmandu. Copyright © 2013 PTC, NCCR North-South and NCCR, Kathmandu, Nepal All rights reserved. ISBN: 978-9937-2-6169-2 Subsidised price: NPR 390/- Cover concept: Pranil Upadhayaya Layout design: Jyoti Khatiwada Printed at: Heidel Press Pvt. Ltd., Dillibazar, Kathmandu Cover photo design: Tourists at the outskirts of Pokhara with Mt. Annapurna and Machhapuchhre on back (top) and Fewa Lake (down) by Ashess Shakya Disclaimer: The content and materials presented in this book are of the respective authors and do not necessarily reflect the views and opinions of Pokhara Tourism Council (PTC), the Swiss National Centre of Competence in Research (NCCR North-South) and Nepal Centre for Contemporary Research (NCCR). Dedication To the people who contributed to developing Pokhara as a tourism city and paradise The editors of the book Tourism in Pokhara: Issues, Trends and Future Prospects for Peace and Prosperity acknowledge supports of Pokhara Tourism Council (PTC) and the Swiss National Centre of Competence in Research (NCCR) North-South, co-funded by the Swiss National Science Foundation (SNSF), the Swiss Agency for Development and Cooperation (SDC), and the participating institutions. -

An Overview of Tourism Diversity in Nepal
Patan Pragya (Volume: 6, Number: 1 2020) Received Date: Jan. 2020 Revised: April 2020 Accepted: June 2020 An Overview of Tourism Diversity in Nepal Minesh Kumar Ghimire Abstract Tourism is the most important service industry of Nepal. It provided big opportunities of national development and income to maintain international harmony. It will argue the more descriptive nature of information. The diversity of tourism has a huge benefit of tourism development. The tourism activities in Nepal are different attractions such as adventure, natural, cultural etc. The Airway is means of Tourist Arrival means of Nepal and Average Length of Stay is 12 days. Key Words: Tourism activities, Tourism Opportunities, diversity, Eco-tourism. Background Tourism is one of the important factors in the economic sector of Nepal. It doesn’t just create employment opportunities but attracts many international tourists which bring in foreign currency. In this regard, to have more international tourist means to be in more foreign currency and as the exchange rate varies, the foreign currency can be a boon for the economic progress of the country. People working in the tourism industry are the direct beneficiary but the people working in agriculture, airlines, hospital, hotels are the indirect beneficiary. The products from the indirect beneficiary can be promoted via tourism and get to the international market as well. It helps people to understand each other and respect each other which helps to maintain harmony in the country and around the world. Various relevant policy documents, proceedings of various seminars, study reports and such other documents can be reviewed for extracting secondary information of tourism and how tourism has been influential in the life of people who are dependent on it. -

Invitation for Bids
Invitation for Bids Government of Nepal (GoN) Rupa Rural Municipality Invitation for Bids for the Supply and Delivery of HDPE Pipe Contract Identification No: NCB/GOODS/RUPA/2075/76-01 Date of publication: 03-03-2019 10:00 1. The Government of Nepal has allocated funds to cover eligible payment under the Contract for Supply and Delivery of HDPE Pipe (IFB No: NCB/GOODS/RUPA/2075/76-01). Bidding is open to all eligible Nepaleses. 2. Rupa Rural Municipality invites electronic bids from eligible bidders for the procurement of Supply and Delivery of HDPE Pipe of Rupa Rural Municipality under National Competitive Bidding procedures. 3. Eligible Bidders may obtain further information and inspect the Bidding Documents at the office of Rupa Rural Municipality Rupa Rural Municipality Rupakot,Kaski Nepal or may visit PPMO website www.bolpatra.gov.np/egp. 4. A complete set of Bidding Documents may be purchased from the following bank/office by eligible Bidders on the submission of a written application, along with the copy of company/firm registration certificate, and upon payment of a non-refundable fee of 3000.0 NRs till 02-04-2019 12:00. If so requested Bidding Documents can also be sent by post/ service upon payment of additional fee for post/courier. However the Employer will not be responsible for delay or non-delivery of the document to sent Name of the Bank: Sunrise Bank Ltd. , POKHARA BRANCH ,Pokhara Kathmandu Name of the Office: Rupa Rural Municipality Office Code no: 47-365-11 Office Account no: 0720518864703001 5. Electronic bids must be submitted to the office Rupa Rural Municipality ,Raupakot,Kaski Rupakot, Kaski Nepal through PPMO website www.bolpatra.gov.np. -

Vulnerability and Impacts Assessment for Adaptation Planning In
VULNERABILITY AND I M PAC T S A SSESSMENT FOR A DA P TAT I O N P LANNING IN PA N C H A S E M O U N TA I N E C O L O G I C A L R E G I O N , N EPAL IMPLEMENTING AGENCY IMPLEMENTING PARTNERS SUPPORTED BY Ministry of Forest and Soil Conservation, Department of Forests UNE P Empowered lives. Resilient nations. VULNERABILITY AND I M PAC T S A SSESSMENT FOR A DA P TAT I O N P LANNING IN PA N C H A S E M O U N TA I N E C O L O G I C A L R E G I O N , N EPAL Copyright © 2015 Mountain EbA Project, Nepal The material in this publication may be reproduced in whole or in part and in any form for educational or non-profit uses, without prior written permission from the copyright holder, provided acknowledgement of the source is made. We would appreciate receiving a copy of any product which uses this publication as a source. Citation: Dixit, A., Karki, M. and Shukla, A. (2015): Vulnerability and Impacts Assessment for Adaptation Planning in Panchase Mountain Ecological Region, Nepal, Kathmandu, Nepal: Government of Nepal, United Nations Environment Programme, United Nations Development Programme, International Union for Conservation of Nature, German Federal Ministry for the Environment, Nature Conservation, Building and Nuclear Safety and Institute for Social and Environmental Transition-Nepal. ISBN : 978-9937-8519-2-3 Published by: Government of Nepal (GoN), United Nations Environment Programme (UNEP), United Nations Development Programme (UNDP), International Union for Conservation of Nature (IUCN), German Federal Ministry for the Environment, Nature Conservation, Building and Nuclear Safety (BMUB) and Institute for Social and Environmental Transition-Nepal (ISET-N). -

Typology and Distribution in Pokhara Lekhnath Metropolitan City
The Geographical Journal of Nepal Vol. 11: 25-44, 2018 Central Department of Geography, Tribhuvan University, Kathmandu, Nepal Open space: Typology and distribution in Pokhara Lekhnath metropolitan city Ramjee Prasad Pokharel1*; and Narendra Raj Khanal2 1Department of Geography, Prithvi Narayan Campus, Pokhara (Tribhuvan University) Nepal; 2Central Department of Geography, Tribhuvan University, Kathmandu, Nepal (*Corresponding Author: [email protected]) Open space is essential part of city life because it provides an opportunity for recreation, playing, religious activities, political activities, cultural activities and so on. This paper discusses the types of open space and its distribution in Pokhara Lekhanath Metropolitan City (PLMC). An inventory of open spaces was prepared based on the available analog maps with intensive field verification. There are eight major and 32 subtypes of open spaces with a total number of 246 within the PLMC. The main types of open spaces are park, playground, religious site, water surface, cave, aesthetic view point, river strip and messy places. Those open spaces vary in form, size, ownership and functions. The distribution of open spaces is not uniform among the 33 Wards in the Pokhara Lekhanath Metropolitan City. The number of open space varies from only one to twenty-one and total area of open space varies from only 51 ha to 4786 ha among those Wards. Per capita area of open space ranges from 0.16 to 659 m2 among those wards. In many wards, per capita area of open space is less than 9 m² which is recommended by FAO. Such a poor situation is created mainly due to the lack of public land use planning, encroachment in open space for development of infrastructure such as public buildings, and lack of knowledge about the importance of open spaces among decision makers and local people and weak capacity of local people to protect and conserve open space from encroachment. -

FAO Fishery Country Profile
FISHERY COUNTRY PROFILE Food and Agriculture FID/CP/NEP Organization of the United Nations PROFIL DE LA PÊCHE PAR PAYS Organisation des Nations Unies pour l'alimentation et May 1997 l'agriculture RESUMEN INFORMATIVO Organización de las Naciones SOBRE Unidas para la Agricultura y la LA PESCA POR PAISES Alimentación THE KINGDOM OF NEPAL GENERAL ECONOMIC DATA Area: 2 147,181 km Water area 1 818 500 ha . 2 20.5 millions Population : 3 4 GDP at purchasers' value (1995/1996) : US$ 4 462 millions GDP per head: US$ 218 Agricultural GDP: US$ 1 720 millions FISHERIES DATA 5 Commodity balance 1995/1996 : Production Imports Exports Total Supply Per caput Supply Thousand tons liveweight equivalent kg/year Fish for direct human 21.9 NA NA 21.9 1.1 consumption Fish for animal feed and 1.0 - - 1.0 0 other non-food purposes Estimated employment (1996): (i) Primary sector: Total employment in the sector is about 266000 (including subsistence and part-time) (ii) Secondary sector: Gross value of fisheries output (at ex-vessel prices) (1995/1996): US$ 29.3 millions 6 Trade (1995/1996) : Value of imports: n.a. Value of exports: n.a. THE STRUCTURE AND CHARACTERISTICS OF THE INDUSTRY Inland fisheries Capture fisheries in Nepal have an artisanal character and no industrial fisheries have developed. Fishermen living scattered along lakes and rivers use traditional gear mainly for subsistence fishing. It has been estimated that there are some 395 000 ha. of rivers and about 5 000 ha. of small and medium sized lakes in the country. Fishing also takes place in irrigated paddy fields and marginal swamp areas, together constituting some 410 000 ha. -

Kathmandu-Pokhara -Ghandruk (9Nights and 10 Days) – a Glimpse of Mountains Along with Culture
KATHMANDU-POKHARA -GHANDRUK (9NIGHTS AND 10 DAYS) – A GLIMPSE OF MOUNTAINS ALONG WITH CULTURE Nepal; the glorious land of Himalayas lies peacefully between the two-giant economy of the world, India and China. Though being a landlock country Nepal is blessed with white fast flowing rivers, lakes, ponds and many more. You will always be surprised with the snake like turning highways and the incredible view of green hills and the feel of villages throughout your journey. Kathmandu; the capital of the nation is also known as land of temples as you will encounter with either big or small temple in almost every step you take. Kathmandu is an incredibly diverse historic city with breathtaking architecture, centuries old Hindu and Buddhist religious sites. Not only in Kathmandu but in every part of Nepal you will experience different culture and its unique magnificence. Nepal will surely win your hearts with her cultural beauty, natural beauty and warmhearted people!!! Currency: 1 USD = NPR. 118.96 (*subject to change) TOUR HIGHLIGHTS: DESTINATION KATHMANDU, POKHARA , GHANDRUK AND DHAMPUS TOUR DURATION 9 NIGHTS AND 10 DAYS HOTEL CATEGORY 3 STAR AT KATHMANDU AND POKHARA SIMPLE LODGES DURING TREK MEAL PLAN BREAKFAST BASIS (LUNCH AND DINNER ONLY DURING TREK) BRIEF ITINERARY: DAY 1: ARRIVAL IN KATHMANDU DAY 2: FULL DAY KATHMANDU CITY TOUR DAY 3: DRIVE TO POKHARA DAY 4: DRIVE TO NAYAPOOL AND TREK TO GHANDRUK DAY 5: TREK GHANDRUK TO JHINU DANDA DAY 6: TREK TO DHAMPUS DAY 7: TREK TO PHEDI AND DRIVE TO POKHARA DAY 8: FULL DAY POKHARA SIGHTSEEING DAY 9: DRIVE BACK TO KATHMANDU DAY 10: DEPARTURE DETAIL ITINERARY DAY 1: ARRIVAL IN KATHMANDU Welcome to the vibrant capital of Nepal. -

Kingdom of Nepal Were Referenced the Country a Dictatorship That Would Last About 100 Years
Grids & Datums KINGDOM OF NEPAL by Clifford J. Mugnier, C.P., C.M.S. “Nepal has been a kingdom for at least 1,500 years. During most of conflicted with the monarchy’s views of its own dignity and with the that period, the Kathmandu Valley has been Nepal’s political, eco- interests of the army. Instead of condoning or encouraging a mul- nomic, and cultural center. The valley’s fertile soil supported thriving tiparty democracy, King Mahendra Bir Bikram Shah Dev launched a village farming communities, and its location along trans-Himalayan coup in late 1960 against Bishweshwar Prasad (B.P.) Koirala’s popularly trade routes allowed merchants and rulers alike to profit. Since the elected government and set up a system of indirect elections that fourth century, the people of the Kathmandu Valley have developed created a consultative democracy. The system served as a sounding a unique variant of South Asian civilization based on Buddhism and board for public opinion and as a tool for economic development Hinduism but influenced as well by the cultures of local Newar citizens without exercising effective political power. Nepal remained until and neighboring Tibetans. One of the major themes in the history of 1990 one of the few nations in the world where the king, wielding Nepal has been the transmission of influences from both the north absolute authority and embodying sacred tradition, attempted to and the south into an original culture. During its entire history, Nepal lead his country towards the twenty-first century” Country( Study, has been able to continue this process while remaining independent. -

Sarangkot Hiking Tours - 7 Days
GPO Box: 384, Ward No. 17, Pushpalal Path Khusibun, Nayabazar, Kathmandu, Nepal Tel: +977-01-4388659 E-Mail: [email protected] www.iciclesadventuretreks.com Sarangkot Hiking Tours - 7 Days Sarangkot hiking is the short hike up towards the hill from Pokhara city. When the rays of sun slowly strikes the snow- capped Himalayan range, the glorious Himalayas changes to a magnificent golden color which quite looks like the range of golden Himalayas. Explore the cultural Kathmandu city and world heritage sites before heading towards Sarangkot,short hiking Pokhara. We begin our Sarangkot hiking tour after driving 200kms west of Kathmandu valley. Pokhara is the most beautiful city of Nepal ad it is famous for sightseeing around the valley, boating in Phewa Lake, Island temple, visiting Mahendra cave, Davis fall and nightlife around lakeside area. Sarangkot village resides at an altitude of 1600m north of Pokhara exhibiting the bird’s eye view of Pokhara city and Phewa Lake. Upon reaching there after short hike through forest, view the magnificent Annapurna Himalayan range, Dhaulagiri Himalayan range, Macchapuchre (Fishtail Mountain) along with scenic view of Pokhara valley. Finally we drive back to Kathmandu and conclude this amazing scenic Sarangkot hiking tour. Experience the best sunrise and sunset views over tallest Himalayan ranges and immerse yourself in the natural beauty of Nepal with Icicles Adventure Treks. GPO Box: 384, Ward No. 17, Pushpalal Path Khusibun, Nayabazar, Kathmandu, Nepal Tel: +977-01-4388659 E-Mail: [email protected] www.iciclesadventuretreks.com PRICE INCLUDES Airport / hotel / airport transfer by private car / van / bus as per above itinerary. -

Gandaki Province
2020 PROVINCIAL PROFILES GANDAKI PROVINCE Surveillance, Point of Entry Risk Communication and and Rapid Response Community Engagement Operations Support Laboratory Capacity and Logistics Infection Prevention and Control & Partner Clinical Management Coordination Government of Nepal Ministry of Health and Population Contents Surveillance, Point of Entry 3 and Rapid Response Laboratory Capacity 11 Infection Prevention and 19 Control & Clinical Management Risk Communication and Community Engagement 25 Operations Support 29 and Logistics Partner Coordination 35 PROVINCIAL PROFILES: BAGMATI PROVINCE 3 1 SURVEILLANCE, POINT OF ENTRY AND RAPID RESPONSE 4 PROVINCIAL PROFILES: GANDAKI PROVINCE SURVEILLANCE, POINT OF ENTRY AND RAPID RESPONSE COVID-19: How things stand in Nepal’s provinces and the epidemiological significance 1 of the coronavirus disease 1.1 BACKGROUND incidence/prevalence of the cases, both as aggregate reported numbers The provincial epidemiological profile and population denominations. In is meant to provide a snapshot of the addition, some insights over evolving COVID-19 situation in Nepal. The major patterns—such as changes in age at parameters in this profile narrative are risk and proportion of females in total depicted in accompanying graphics, cases—were also captured, as were which consist of panels of posters the trends of Test Positivity Rates and that highlight the case burden, trend, distribution of symptom production, as geographic distribution and person- well as cases with comorbidity. related risk factors. 1.4 MAJOR Information 1.2 METHODOLOGY OBSERVATIONS AND was The major data sets for the COVID-19 TRENDS supplemented situation updates have been Nepal had very few cases of by active CICT obtained from laboratories that laboratory-confirmed COVID-19 till teams and conduct PCR tests. -
![S]Gb|Lo Cfof]Hgf Sfof{Gjog Osfo{ E"Sdklo Cfjf; K'glg{Df{0F Cfof]Hgf Hjfun, Nlntk'/ Pokhara सि.नं](https://docslib.b-cdn.net/cover/8424/s-gb-lo-cfof-hgf-sfof-gjog-osfo-e-sdklo-cfjf-kglg-df-0f-cfof-hgf-hjfun-nlntk-pokhara-1428424.webp)
S]Gb|Lo Cfof]Hgf Sfof{Gjog Osfo{ E"Sdklo Cfjf; K'glg{Df{0F Cfof]Hgf Hjfun, Nlntk'/ Pokhara सि.नं
g]kfn ;/sf/ ;+3Lo dfldnf tyf :yfgLo ljsf; dGqfno s]Gb|Lo cfof]hgf sfof{Gjog OsfO{ e"sDkLo cfjf; k'glg{df{0f cfof]hgf Hjfun, nlntk'/ Pokhara सि.नं. घरधनीको नाम, थर सिल्ला गासिि/नपा िडा टोल/िस्ति घ.क्र.िं सनस्सा नं ि륍झौता क्र.ि काडडको सकसिम काडड नं मोिाइल LATITUDE LONGITUDE ALTITUDE 1 Purna Bahadur Sai Kaski Pokhara 1 Adhikaritol 9 1059760 40-32-1-0-001 9804103410 28.23508181 83.98643232 888.0475091 2 Nirvaya Raj Shrestha Kaski Pokhara 1 Bagar 5 1059756 40-32-1-0-002 Citizenship Card 2 9817107628 28.23919646 83.98721391 876.9154081 3 Basudev Parajuli Kaski Pokhara 2 Archalbot 1 679508 40-32-2-0-001 9846066897 28.23494932 83.98137401 857.510786 4 Radha Regmi Kaski Pokhara 2 Bindabasini 18 1059753 40-32-2-0-002 9846101918 28.23692125 83.983984 878.0071361 5 Kedar Pariyar Kaski Pokhara 3 Nilgiri tole 10 607985 40-32-3-0-001 9806742276 28.23357438 83.98660705 872.7824949 6 Bal Bahadur Jalari Kaski Pokhara 3 Gyanmarg 1 607976 40-32-3-0-002 Citizenship Card 46101/14209 9846323144 28.22765526 83.99073982 846.5062842 7 Gopal Damai Kaski Pokhara 4 Firke pul 1 607987 40-32-4-0-001 9816182990 28.22882086 83.98104833 869.1887306 8 Radha Devi Parajuli Kaski Pokhara 5 Children park 1 646960 40-32-5-0-001 Citizenship Card 410 9846350869 28.22339906 83.9801289 837.8678465 9 Amrita Damai Kaski Pokhara 5 Bastari bagar 4 646963 40-32-5-0-002 9846778273 28.22782771 83.97303174 832.4448929 10 Jhalak Bahadur Karki Kaski Pokhara 5 Dharmasthali marga 2 646961 40-32-5-0-003 Citizenship Card 46017307808 9846039963 28.22315219 83.97701266 830.4867469 11 Guru Prasad -

Rural Municipality Profile
RURAL MUNICIPALITY PROFILE Office of Rural Municipality Arughat Province no. 4 2074 , ii , Abbreviation Acronyms Full Form VDC Village Development Committee RM Rural Municipality FY Fiscal Year M Meter Mm Millimeter Km Kilo meter DDC District Development Committee DCWB District Child Welfare Board DRCN District Road Core Network Ha Hector ECD Education for Child Development SLC School Leaving Certificate DEO District Education Office DHO District Health Office CLC Community Learning Center PS Primary School LSS Lower Secondary School SS Secondary School DCWB District Child Welfare Board iii , Contents 1 METHODOLOGY ................................................................................................................. 1 1.1 Background ...................................................................................................................... 1 1.2 Objective .......................................................................................................................... 1 1.3 Method ............................................................................................................................. 1 1.4 Limitation of Study .......................................................................................................... 2 2 INTRODUCTION .................................................................................................................. 3 2.1 Background ...................................................................................................................... 3 2.2 Geo-Physical