Gandaki Province
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Code Under Name Girls Boys Total Girls Boys Total 010290001
P|D|LL|S G8 G10 Code Under Name Girls Boys Total Girls Boys Total 010290001 Maiwakhola Gaunpalika Patidanda Ma Vi 15 22 37 25 17 42 010360002 Meringden Gaunpalika Singha Devi Adharbhut Vidyalaya 8 2 10 0 0 0 010370001 Mikwakhola Gaunpalika Sanwa Ma V 27 26 53 50 19 69 010160009 Phaktanglung Rural Municipality Saraswati Chyaribook Ma V 28 10 38 33 22 55 010060001 Phungling Nagarpalika Siddhakali Ma V 11 14 25 23 8 31 010320004 Phungling Nagarpalika Bhanu Jana Ma V 88 77 165 120 130 250 010320012 Phungling Nagarpalika Birendra Ma V 19 18 37 18 30 48 010020003 Sidingba Gaunpalika Angepa Adharbhut Vidyalaya 5 6 11 0 0 0 030410009 Deumai Nagarpalika Janta Adharbhut Vidyalaya 19 13 32 0 0 0 030100003 Phakphokthum Gaunpalika Janaki Ma V 13 5 18 23 9 32 030230002 Phakphokthum Gaunpalika Singhadevi Adharbhut Vidyalaya 7 7 14 0 0 0 030230004 Phakphokthum Gaunpalika Jalpa Ma V 17 25 42 25 23 48 030330008 Phakphokthum Gaunpalika Khambang Ma V 5 4 9 1 2 3 030030001 Ilam Municipality Amar Secondary School 26 14 40 62 48 110 030030005 Ilam Municipality Barbote Basic School 9 9 18 0 0 0 030030011 Ilam Municipality Shree Saptamai Gurukul Sanskrit Vidyashram Secondary School 0 17 17 1 12 13 030130001 Ilam Municipality Purna Smarak Secondary School 16 15 31 22 20 42 030150001 Ilam Municipality Adarsha Secondary School 50 60 110 57 41 98 030460003 Ilam Municipality Bal Kanya Ma V 30 20 50 23 17 40 030460006 Ilam Municipality Maheshwor Adharbhut Vidyalaya 12 15 27 0 0 0 030070014 Mai Nagarpalika Kankai Ma V 50 44 94 99 67 166 030190004 Maijogmai Gaunpalika -

Sustainable Tourism Enhancement in Nepal's Protected Areas Public Disclosure Authorized
Sustainable Tourism Enhancement in Nepal's Protected Areas Public Disclosure Authorized Environmental and Social Management Framework Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized National Trust for Nature Conservation GPO Box 3712, Khumaltar, Lalitpur, Nepal May 2020 Executive Summary 1. Description of the Project: Tourism is one of the major contributors to the sustainable economy of Nepal. The direct contribution of the tourism sector in the national GDP was at 4% in 2017 and is forecasted to rise by 3.8% per annum to reach 4.2% in 2028 (World Travel and Tourism Council, 2018). Despite tremendous growth potential in tourism sector, Nepal stands as a low-cost tourist destination with much lower daily tourist spending than the regional average. This is a high time for Nepal to think about and harness high value nature-based tourism. Nature based tourism is a key driver of Nepal's tourism, providing the sector both comparative and competitive advantages in the unique setting of rich topographic, biological and cultural diversity. In this context, the World Bank is supporting GoN to implement the project entitled “Sustainable Tourism Enhancement in Nepal’s Protected Areas (STENPA)". Project Destinations: The project focuses on areas with Nature-Based Tourism (NBT) potential with the aim of piloting a sustainable tourism approach that can be replicated across Nepal’s protected areas (PAs). The project destinations include PA at their core, nearby gateway cities and surrounding areas with NBT potential, and has identified six PAs as the initial project destinations (Bardia, Banke Shukla Phanta and Rara National Parks, and their buffer zones; and Annapurna and Manaslu conservation Areas). -

Nepal Human Rights Year Book 2021 (ENGLISH EDITION) (This Report Covers the Period - January to December 2020)
Nepal Human Rights Year Book 2021 (ENGLISH EDITION) (This Report Covers the Period - January to December 2020) Editor-In-Chief Shree Ram Bajagain Editor Aarya Adhikari Editorial Team Govinda Prasad Tripathee Ramesh Prasad Timalsina Data Analyst Anuj KC Cover/Graphic Designer Gita Mali For Human Rights and Social Justice Informal Sector Service Centre (INSEC) Nagarjun Municipality-10, Syuchatar, Kathmandu POBox : 2726, Kathmandu, Nepal Tel: +977-1-5218770 Fax:+977-1-5218251 E-mail: [email protected] Website: www.insec.org.np; www.inseconline.org All materials published in this book may be used with due acknowledgement. First Edition 1000 Copies February 19, 2021 © Informal Sector Service Centre (INSEC) ISBN: 978-9937-9239-5-8 Printed at Dream Graphic Press Kathmandu Contents Acknowledgement Acronyms and Abbreviations Foreword CHAPTERS Chapter 1 Situation of Human Rights in 2020: Overall Assessment Accountability Towards Commitment 1 Review of the Social and Political Issues Raised in the Last 29 Years of Nepal Human Rights Year Book 25 Chapter 2 State and Human Rights Chapter 2.1 Judiciary 37 Chapter 2.2 Executive 47 Chapter 2.3 Legislature 57 Chapter 3 Study Report 3.1 Status of Implementation of the Labor Act at Tea Gardens of Province 1 69 3.2 Witchcraft, an Evil Practice: Continuation of Violence against Women 73 3.3 Natural Disasters in Sindhupalchok and Their Effects on Economic and Social Rights 78 3.4 Problems and Challenges of Sugarcane Farmers 82 3.5 Child Marriage and Violations of Child Rights in Karnali Province 88 36 Socio-economic -
![Wild Mammals of the Annapurna Conservation Area Cggk"0F{ ;+/If0f If]Qsf :Tgwf/L Jgohgt' Wild Mammals of the Annapurna Conservation Area - 2019](https://docslib.b-cdn.net/cover/7316/wild-mammals-of-the-annapurna-conservation-area-cggk-0f-if0f-if-qsf-tgwf-l-jgohgt-wild-mammals-of-the-annapurna-conservation-area-2019-127316.webp)
Wild Mammals of the Annapurna Conservation Area Cggk"0F{ ;+/If0f If]Qsf :Tgwf/L Jgohgt' Wild Mammals of the Annapurna Conservation Area - 2019
Wild Mammals of the Annapurna Conservation Area cGgk"0f{ ;+/If0f If]qsf :tgwf/L jGohGt' Wild Mammals of the Annapurna Conservation Area - 2019 ISBN 978-9937-8522-8-9978-9937-8522-8-9 9 789937 852289 National Trust for Nature Conservation Annapurna Conservation Area Project Khumaltar, Lalitpur, Nepal Hariyo Kharka, Pokhara, Kaski, Nepal National Trust for Nature Conservation P.O. Box: 3712, Kathmandu, Nepal P.O. Box: 183, Kaski, Nepal Tel: +977-1-5526571, 5526573, Fax: +977-1-5526570 Tel: +977-61-431102, 430802, Fax: +977-61-431203 Annapurna Conservation Area Project Email: [email protected] Email: [email protected] Website: www.ntnc.org.np Website: www.ntnc.org.np 2019 Wild Mammals of the Annapurna Conservation Area cGgk"0f{ ;+/If0f If]qsf :tgwf/L jGohGt' National Trust for Nature Conservation Annapurna Conservation Area Project 2019 Wild Mammals of the Annapurna Conservation Area cGgk"0f{ ;+/If0f If]qsf :tgwf/L jGohGt' Published by © NTNC-ACAP, 2019 All rights reserved Any reproduction in full or in part must mention the title and credit NTNC-ACAP. Reviewers Prof. Karan Bahadur Shah (Himalayan Nature), Dr. Naresh Subedi (NTNC, Khumaltar), Dr. Will Duckworth (IUCN) and Yadav Ghimirey (Friends of Nature, Nepal). Compilers Rishi Baral, Ashok Subedi and Shailendra Kumar Yadav Suggested Citation Baral R., Subedi A. & Yadav S.K. (Compilers), 2019. Wild Mammals of the Annapurna Conservation Area. National Trust for Nature Conservation, Annapurna Conservation Area Project, Pokhara, Nepal. First Edition : 700 Copies ISBN : 978-9937-8522-8-9 Front Cover : Yellow-bellied Weasel (Mustela kathiah), back cover: Orange- bellied Himalayan Squirrel (Dremomys lokriah). -
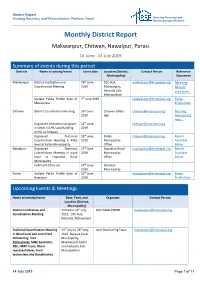
Monthly District Report
District Report Housing Recovery and Reconstruction Platform, Nepal Housing Recovery and Reconstruction Platform Monthly District Report Makwanpur, Chitwan, Nawalpur, Parasi 14 June - 14 July 2019 Summary of events during this period Districts Name of activity/event Event date Location (District, Contact Person Reference Municipality) Document Makwanpur District Facilitation and 18th June DCC Hall, [email protected] Meeting Coordination Meeting 2019 Makwanpur, Minute Hetauda Sub- click here.. Metropolitan Update Palika Profile data of 7th June 2019 [email protected] Palika Makwanpur Profile Data Chitwan District Coordination Meeting 26th June Chitwan GMaLi [email protected] Meeting 2019 Hall Minute click here... Organized interaction program 24th June, [email protected] in GMALI DLPIU and Building 2019 DLPIU at Chitwan Organized Technical 26th june, Kalika [email protected] Report Coordination Meeting in Plika 2019 Municipality Available level at Kalika Municipality Office Below Nawalpur Organized Technical 27th June Hupsekot Rural [email protected] Report Coordination Meeting in ward 2019 Municipality Available level at Hupsekot Rural Office Below Municipality Field visit Carry out 27th June, Devchuli 2019 Municipality Parasi Update Palika Profile data of 12th June [email protected] Palika Nawalpur 2019 Profile Data Upcoming Events & Meetings Name of activity/event Date, Time, and Organizer Contact Person Location (District, Municipality) District Facilitation and Tentative 19th July, DCC/GMaLI/HRRP [email protected] Coordination Meeting 2019; DCC Hall, Hetauda, Makwanpur Technical Coordination Meeting 24th July to 26th July, Joint Monitoring Team [email protected] in Ward level and Joint Field 2019 Bakaiya Rural Monitoring Visit Municipality, Participants: M&E Specialist, Makwanpur Gadhi DSE, HRRP team, Ward and Hetauda Sub- representatives, local Metropolitan technicians and Beneficiaries. -

Assessing the Impact of Nepal's 2015 Earthquake On
Assessing the Impact of Nepal’s 2015 Earthquake on Older People and Persons with Disabilities and How Gender and Ethnicity Factor into That Impact STUDY REPORT A Joint Initiative of HelpAge International, CBM International and NDRC Nepal Submitted to HelpAge International Jawalakhel, Lalitpur Submitted by National Disaster Risk Reduction Centre (NDRC Nepal) New Baneshwor, Kathmandu Nepal P.O. Box: 19532 Telephone/Fax: 01-4115619; 01-2299380 Email: [email protected] ; [email protected] URL: www.ndrcnepal.org March 2016 1 NDRC Nepal’s Study Team Senior Researchers 1. Dr. Dhruba Gautam, Team Leader/Thematic Expert 2. Mr. Madhusudan Gautam, Quantitative Analyst/Survey Expert 3. Ms Pratistha Koirala, Gender Expert Research Supervisors 1. Ms Salina Bhattarai 2. Mr. Chetan Singh Ter 3. Mr. Bijay Tharu 4. Mr. Raj Kumar Chaudhari Research Assistants 1. Ms Samita Tamrakar 2. Ms Pratikshya Sharma 3. Ms Akriti Poudyal 4. Ms Lemina Bhattarai 5. Mr Nitesh Acharya 6. Mr Saphal Sapkota 7. Mr Lavraj Purie 8. Mr Sanjog Risal 9. Mr Mangal Lama 10. Mr Santosh Basnet 11. Mr Prabin Thapa 12. Mr Sivan Lamichhane 13. Mr Santa Bahadur Jirel 14. Mr Saroj Simkhada 15. Ms Grishma Paneru 16. Ms Alina Chantel Research associates 1. Mr. Ankit Adhikari 2. Mr Pratap Maharjan Disclaimer The findings, interpretations, and conclusions expressed herein are of NDRC Nepal and do not necessarily reflect the view of HelpAge International and CBM International. For more information, please contact either at NDRC Nepal, CBM and HAI. 2 List of acronyms DAO District Administration -

COVID19 Reporting of Naukunda RM, Rasuwa.Pdf
स्थानिय तहको विवरण प्रदेश जिल्ला स्थानिय तहको नाम Bagmati Rasuwa Naukunda Rural Mun सूचना प्रविधि अधिकृत पद नाम सम्पर्क नं. वडा ठेगाना कैफियत सूचना प्रविधि अधिकृतसुमित कुमार संग्रौला 9823290882 ६ गोसाईकुण्ड गाउँपालिका जिम्मेवार पदाधिकारीहरू क्र.स. पद नाम सम्पर्क नं. वडा ठेगाना कैफियत 1 प्रमुख प्रशासकीय अधिकृतनवदीप राई 9807365365 १३ विराटनगर, मोरङ 2 सामजिक विकास/ स्वास्थ्यअण प्रसाद शाखा पौडेल प्रमुख 9818162060 ५ शुभ-कालिका गाउँपालिका, रसुवा 3 सूचना अधिकारी डबल बहादुर वि.के 9804669795 ५ धनगढी उपमहानगरपालिका, कालिका 4 अन्य नितेश कुमार यादव 9816810792 ६ पिपरा गाउँपालिका, महोत्तरी 5 6 n विपद व्यवस्थापनमा सहयोगी संस्थाहरू क्र.स. प्रकार नाम सम्पर्क नं. वडा ठेगाना कैफियत 1 2 3 4 5 6 7 8 9 n ारेाइन केको ववरण ID ारेाइन केको नाम वडा ठेगाना केन्द्रको सम्पर्क व्यक्तिसम्पर्क नं. भवनको प्रकार बनाउने निकाय वारेटाइन केको मता Geo Location (Lat, Long) Q1 गौतम बुद्ध मा.वि क्वारेन्टाइन स्थल ३ फाम्चेत नितेश कुमार यादव 9816810792 विध्यालय अन्य (वेड संया) 10 28.006129636870693,85.27118702477858 Q2 Q3 Q4 Q5 Q6 Q7 Q8 Q9 Q10 Q11 Qn भारत लगायत विदेशबाट आएका व्यक्तिहरूको विवरण अधारभूत विवरण ारेाइन/अताल रफर वा घर पठाईएको ववरण विदेशबाट आएको हो भने मात्र कैिफयत ID नाम, थर लिङ्ग उमेर (वर्ष) वडा ठेगाना सम्पर्क नं. -
Final Report
Detail Study of Self-Reliant Industrial Goods in Nepal Final Report Submitted To: Government of Nepal Ministry of Industry, Commerce and Supplies Department of Industry Tripureswor, Kathmandu, Nepal Submitted By: Quality & Environmental Management Service Pvt. Ltd. Kathmandu, Nepal Telephone-01-5705455, E-mail- [email protected] June, 2021 ACKNOWLEDGEMENT Quality and Environmental Management Service Pvt. Ltd. takes an opportunity to express its’ gratitude to those Experts/stakeholders who contributed their valuable time and added precious value in this study. Particularly it extends sincere appreciation to Mr. Jiblal Bhusal, Director General, Mr. Krishna Prasad Kharel, Director; Mr. Pushpa Raj Shiwakoti, Statistical Officer, Mr. Santosh Koirala Mechanical Engineer and others staff of the Department of Industry for their kind inputs and guidance to bring this report to the final stage. We would also like to appreciate for the time and inputs of Mr. Jiblal Kharel Board member of Nepal Tea and Coffee Development Board (NTCDB), Mr. Naresh Katwal Chairperson of Federation of Nepalese Business Association, Mr. Dilli Baskota Member Sectary of HOTPA, Mr. Asish Sigdel Chairperson of NEEMA, Mr. Chandra khadgi member Sectary of NPMA, Mr Suresh Mittal Chairperson NTPA Jhapa and Mr. Rudra Prasad Neupane Board Member of FMAN. We would also like to thank for valuable input from Mr. Bikash Keyal Director of Narayani Strips Pvt. Ltd, Mr. A.K Jha GM of Hulas Steel Pvt. Ltd, Mr. Dibya Sapkota GM of Aarati Strip Pvt. Ltd., Mr Devendra Sahoo GM of Panchakanya Steel Pvt. Ltd, Mr. Laxman Aryal Chairperson of Jasmin Paints Pvt. Ltd. Mr.Buddhi Bahadur K.C chairperson of Applo Paints Pvt. -

Bagmati Province Emergency Response Preparedness
VULNERABILITY INDICATORS BAGMATI PROVINCE EMERGENCY RESPONSE PREPAREDNESS as of June 2021 Water and Sanitation Human Development Indicators Source of Drinking Water Improved Source of Drinking water 30,636.40 Gross Domestic Product 97.3% NPR million ie n t Infant Mortality Rate (MICS) Unimproved Source of Drinking water 16 per thousand 2.7% Human Development Index (HDI) 0.66 Type of Toilet Used 72.01 Life expectancy (HDI) Improved Sanitation facilities 97.8 % Unimproved Sanitation facilities Note* : 2.2 % This is a living document. We will be continuously editing and updating with revisions. 76.7 % of household population with E. coli in source water Early Childhood Development Attitude towards Domestic Violence Index score of children age 3-4 years are developmentally on 29.5% of women age 15-49 years believes a husband is justi�ied in 73.9% beating his wife in various circumstances track in literacy- numeracy, physical, social-emotional, and learning domains 56.5 % of women age 15-49 years believes a mother-in-law is justi�ied in verbally abusing and threatening her daughter-in-law 6.9% of children age 0-17 living with neither in various circumstance biological parent Icons : https://thenounproject.com/ Source : Multiple Indicator Cluster Surveys 2019 and HDI 2019 report VULNERABILITY INDICATORS BAGMATI PROVINCE EMERGENCY RESPONSE PREPAREDNESS as of June 2021 Adult / Child Disfunctioning Shelter Natural floor Other Rudimentary wall Functional dif�iculties in at least one domain: Other Seeing, Hearing, Walking, Communication ie n t 2.4 % Mud bonded bricks/stone Age 18 - 49 1.3 % Finished floor Finished wall Age 02 - 04 1.0 % Type of House Foundation Type of Outer Wall Health Insurance covergae Finished roof It is one protection scheme that present the percentage of men and women covered by health insurance Age 15 - 49 5.2 % 6.3% Type of Roof Age 05 - 17 5.9% Rural Urban The Nepal Multiple Indicator Cluster Survey (MICS) is an international % of women using appropriate multi-purpose household survey. -

Participatory Ranking of Fodders in the Western Hills of Nepal
Journal of Agriculture and Natural Resources (2020) 3(1): 20-28 ISSN: 2661-6270 (Print), ISSN: 2661-6289 (Online) DOI: https://doi.org/10.3126/janr.v3i1.27001 Research Article Participatory ranking of fodders in the western hills of Nepal Bir Bahadur Tamang1, Manoj Kumar Shah2*, Bishnu Dhakal1, Pashupati Chaudhary3 and Netra Chhetri4 1Local Initiatives for Bo-diversity, Research and Development (LI-BIRD), Pokhara, Nepal 2Nepal Agricultural Research Council, Nepal 3International Center for Integrated Mountain Development (ICIMOD), Khumaltar, Nepal 4Arizona State University, America *Correspondence: [email protected] ORCID: https://orcid.org/0000-0003-4102-3869 Received: August 11, 2019; Accepted: November 12, 2019; Published: January 7, 2020 © Copyright: Tamang et al. (2020). This work is licensed under a Creative Commons Attribution-Non Commercial 4.0 International License. ABSTRACT Fodder is an important source of feed of the ruminants in Nepal. In the mid hills of Nepal, farmers generally practice integrated farming system that combines crop cultivation with livestock husbandry and agroforestry. Tree fodders are good sources of protein during the forage and green grass scarcity periods especially in dry season. Local communities possess indigenous knowledge for the selection of grasses and tree fodders at different seasons in mid hills of western Nepal. A study was conducted on the perception of farmers with respect to selection of fodder species in eight clusters in Kaski and Lumjung districts that range 900-2000 meter above sea level and receive average precipitation of 2000- 4500mm per annum. During the fodder preference ranking, farmers prepared the inventory of fodders found around the villages and nearby forests and selected top ten most important fodders in terms of their availability, palatability, fodder yield, milk yield and milk fat yield. -

NEPAL Earthquake ECHO CRISIS FLASH No
NEPAL Earthquake ECHO CRISIS FLASH No. 10 shortage Period covered 1. Map 25 April – 4 May 2015 Time of validity 18:00 (Kathmandu) – 12:15 (UTC) ECHO Field Office New Delhi – INDIA Number of dead (Government of Nepal): 7 276 Number of wounded (Government of Nepal): 14 362 2. Situation The death toll resulting from the earthquake which struck central Nepal on 25 April has risen to 7 276, with 14 362 injured (Government of Nepal-GoN figures, 4 May). It is anticipated that these figures will further increase as remote areas are becoming accessible for government officials and humanitarian actors. On 3 May, the GoN declared the USAR (Urban Search and Rescue) phase over; it is now paramount that the emergency humanitarian response is further scaled up to reach remote and most affected Village Development Committees (VDCs), ensuring speedy movement and delivery of relief items. According to UN estimates, up to 8 million people have been affected by the ECHO Emergency Contact earthquake. Over 54% of the deaths have been recorded in the districts of Tel.: +32 2 29 21112 Sindhupalchowk and Kathmandu, but there remain entire districts, such as Fax: +32 2 29 86651 Rasuwa, which have yet to be accessed. Approximately 2.8 million people are [email protected] believed to have been temporarily displaced from their homes (USAID Factsheet 7), though numbers are decreasing as people return home in the ECHO Crisis Flash No. 10 – NEPAL Earthquake Kathmandu Valley or are moving from there to their rural districts of origin. Over 10 700 houses have been reported destroyed, with over 14 700 damaged; the GoN estimates that over 200 000 houses have been destroyed and more than 188 000 damaged (GoN, 3 May). -

Club Health Assessment MBR0087
Club Health Assessment for District 325A1 through April 2021 Status Membership Reports Finance LCIF Current YTD YTD YTD YTD Member Avg. length Months Yrs. Since Months Donations Member Members Members Net Net Count 12 of service Since Last President Vice Since Last for current Club Club Charter Count Added Dropped Growth Growth% Months for dropped Last Officer Rotation President Activity Account Fiscal Number Name Date Ago members MMR *** Report Reported Report *** Balance Year **** Number of times If below If net loss If no When Number Notes the If no report on status quo 15 is greater report in 3 more than of officers thatin 12 months within last members than 20% months one year repeat do not haveappears in two years appears appears appears in appears in terms an active red Clubs less than two years old SC 138770 Bansbari 07/12/2019 Active 41 15 0 15 57.69% 26 0 N 1 $600.02 P,MC 138952 Bargachhi Green City 07/12/2019 Active 25 1 0 1 4.17% 24 4 N 5 142398 Biratnagar A One 08/09/2020 Active 32 32 0 32 100.00% 0 2 N 1 M,MC,SC 138747 Biratnagar Birat Medical 07/12/2019 Active 21 1 0 1 5.00% 20 3 N 3 90+ Days P,S,T,M,VP 138954 Biratnagar Capital City 07/12/2019 Active 20 0 0 0 0.00% 20 21 1 None N/R 90+ Days MC,SC M,MC,SC 140415 Biratnagar Entrepreneur 01/06/2020 Active 18 0 0 0 0.00% 20 10 2 R 10 90+ Days M 139007 Biratnagar Greater 07/12/2019 Active 31 8 3 5 19.23% 26 1 4 3 N 3 Exc Award (06/30/2020) VP 139016 Biratnagar Health Professional 07/12/2019 Active 26 4 1 3 13.04% 23 1 0 N 3 Exc Award (06/30/2020) 138394 Biratnagar Mahanagar