Guidance on the Diagnosis Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Siphoning Diesel: a Fatal Mistake
CASE REPORT Siphoning diesel: a fatal mistake Leong Wei Cheng, MRCP, Brian Cheong Mun Keong, FRCP Department of Medicine, Hospital Teluk Intan cervical lymphadenopathy and auscultation of his lungs SUMMARY revealed normal findings. Examination of other systems did Diesel is commonly used as fuel for engines and is distilled not reveal any abnormalities. from petroleum. Diesel has toxic potential and can affect multiple organs. Exposure can occur after ingestion, Initial blood investigations showed evidence of acute kidney inhalation or through the dermal route. The practice of injury (urea: 16.7 mmol/l, sodium 129 mmol/l, potassium 3.7 siphoning diesel using a rubber tubing and the mouth is mmol/l and creatinine 937 µmol/l). There was presence of common in rural communities. This can lead to accidental protein and erythrocytes (2+) in his urine. His full blood count ingestion and aspiration. Here we report a case of a patient showed elevated white cell count of 11,600/µl (neutrophil who accidentally ingested diesel during siphoning, which 85%) with normal haemoglobin concentration (15.9 g/dl) caused extensive erosion of the oral cavity and oesophagus and platelets (185,000/µl). Liver transaminases were normal. leading to pneumomediastinum and severe chemical lung Chest radiograph showed clear lung fields. His provisional injury. The patient responded well initially to steroids and diagnosis was acute tonsillitis with post- infectious Rapidly supportive care but required prolonged hospitalisation. He Progressive Glomerolonephritis (RPGN). Intravenous (IV) developed complications of nosocomial infection and Ceftriaxone 2 g daily was started. succumbed 23 days after admission. He became progressively more tachypnoeic in the ward with KEY WORDS: Diesel; siphon; chemical pneumonitis; oesophageal perforation; worsening renal function and metabolic acidosis. -

Review of Succimer for Treatment of Lead Poisoning
Review of Succimer for treatment of lead poisoning Glyn N Volans MD, BSc, FRCP. Department of Clinical Pharmacology, School of Medicine at Guy's, King's College & St Thomas' Hospitals, St Thomas' Hospital, London, UK Lakshman Karalliedde MB BS, DA, FRCA Consultant Medical Toxicologist, CHaPD (London), Health Protection Agency UK, Visiting Senior Lecturer, Division of Public Health Sciences, King's College Medical School, King's College , London Senior Research Collaborator, South Asian Clinical Toxicology Research Collaboration, Faculty of Medicine, Peradeniya, Sri Lanka. Heather M Wiseman BSc MSc Medical Toxicology Information Services, Guy’s and St Thomas’ NHS Foundation Trust, London SE1 9RT, UK. Contact details: Heather Wiseman Medical Toxicology Information Services Guy’s & St Thomas’ NHS Foundation Trust Mary Sheridan House Guy’s Hospital Great Maze Pond London SE1 9RT Tel 020 7188 7188 extn 51699 or 020 7188 0600 (admin office) Date 10th March 2010 succimer V 29 Nov 10.doc last saved: 29-Nov-10 11:30 Page 1 of 50 CONTENTS 1 Summary 2. Name of the focal point in WHO submitting or supporting the application 3. Name of the organization(s) consulted and/or supporting the application 4. International Nonproprietary Name (INN, generic name) of the medicine 5. Formulation proposed for inclusion 6. International availability 7. Whether listing is requested as an individual medicine or as an example of a therapeutic group 8. Public health relevance 8.1 Epidemiological information on burden of disease due to lead poisoning 8.2 Assessment of current use 8.2.1 Treatment of children with lead poisoning 8.2.2 Other indications 9. -

Asbestos, So That the Statement That
Br J Ind Med: first published as 10.1136/oem.48.6.430 on 1 June 1991. Downloaded from 430 Forum 49 Muehleck E. Letter to WWF Sheperd bles paranoia. In the so that the statement (Turner and Newall). 8 March, 1943. fully developed asbestos, that 50 Hardy HL. Personal communications, form of this psychosis the individual the disease was "discovered by the 1982, 1989. adopts a false premise and then uses ancients," while adding historical 51 Brown V. Letter to E Muehleck (Keas- every device of selection and bias to colour and apparent verisimilitude, is bey & Mattison Co) and JFD Rohr- bach (Raybestos-Manhattan). 22 support it. In the case of a person who manifest nonsense. October, 1948. thinks he is Napoleon or she is the This temptation to dramatise and 52 Brown V. Letter to sponsors (Amer Virgin Mary it is easy to recognise the emotionalise is apparent throughout Brake Shoe, Gatke Corp, Keasbey false premise. is the whole book. I have not and Mattison, Raybestos-Manhattan, It less easy with a counted the Thermoid Corp, Union Asbestos and subject which has been ventilated in emotional adjectives but the book is Rubber Co, Russell Manufacturing the media over the last 25 years to such liberally besprinkled with them while Co, United States Gypsum Co). 27 an extent that the average man in the the author flogs himselfinto a lather of October 1948. 53 Brown V. Letter to WT Kelly (Amer street tends to agree with the premise indignation. One early example is a Brake Shoe). 12 November, 1948. -

Sodium Cellulose Phosphate Sodium Edetate
Sevelamer/Sodium Edetate 1463 excreted by the kidneys. It may be used as a diagnostic is not less than 9.5% and not more than 13.0%, all calculated on supplement should not be given simultaneously with test for lead poisoning but measurement of blood-lead the dried basis. The calcium binding capacity, calculated on the sodium cellulose phosphate. dried basis, is not less than 1.8 mmol per g. concentrations is generally preferred. Sodium cellulose phosphate has also been used for the Sodium calcium edetate is also a chelator of other Adverse Effects and Precautions investigation of calcium absorption. heavy-metal polyvalent ions, including chromium. A Diarrhoea and other gastrointestinal disturbances have Preparations cream containing sodium calcium edetate 10% has been reported. USP 31: Cellulose Sodium Phosphate for Oral Suspension. been used in the treatment of chrome ulcers and skin Sodium cellulose phosphate should not be given to pa- Proprietary Preparations (details are given in Part 3) sensitivity reactions due to contact with heavy metals. tients with primary or secondary hyperparathyroidism, Spain: Anacalcit; USA: Calcibind. Sodium calcium edetate is also used as a pharmaceuti- hypomagnesaemia, hypocalcaemia, bone disease, or cal excipient and as a food additive. enteric hyperoxaluria. It should be used cautiously in pregnant women and children, since they have high Sodium Edetate In the treatment of lead poisoning, sodium calcium calcium requirements. Sodu edetynian. edetate may be given by intramuscular injection or by Patients should be monitored for electrolyte distur- intravenous infusion. The intramuscular route may be Эдетат Натрия bances. Uptake of sodium and phosphate may increase CAS — 17421-79-3 (monosodium edetate). -

Uses and Administration Adverse Effects and Precautions Pharmacokinetics Uses and Administration
1549 The adverse effects of dicobalt edetate are more severe in year-old child: case report and review of literature. Z Kardiol 2005; 94: References. 817-2 3. the absence of cyanide. Therefore, dicobalt edetate should I. Schaumann W, et a!. Kinetics of the Fab fragments of digoxin antibodies and of bound digoxin in patients with severe digoxin intoxication. Eur 1 not be given unless cyanide poisoning is confirmed and 30: Administration in renal impairment. In renal impairment, Clin Pharmacol 1986; 527-33. poisoning is severe such as when consciousness is impaired. 2. Ujhelyi MR, Robert S. Pharmacokinetic aspects of digoxin-specific Fab elimination of antibody-bound digoxin or digitoxin is therapy in the management of digitalis toxicity. Clin Pharmacokinet 1995; Oedema. A patient with cyanide toxicity developed delayed1·3 and antibody fragments can be detected in the 28: 483-93. plasma for 2 to 3 weeks after treatment.1 The rebound in 3. Renard C, et al. Pharmacokinetics of dig,'><i<1-sp,eei1ie Fab: effects of severe facial and pulmonary oedema after treatment with decreased renal function and age. 1997; 44: 135-8. dicobalt edetate.1 It has been suggested that when dicobalt free-digoxin concentrations that has been reported after edetate is used, facilities for intubation and resuscitation treatment with digoxin-specific antibody fragments (see P (Jrations should be immediately available. Poisoning, below), occurred much later in patients with r.�p renal impairment than in those with normal renal func Proprietary Preparations (details are given in Volume B) 1. Dodds C, McKnight C. Cyanide toxicity after immersion and the hazards tion. -

A Short History of Occupational Disease: 2. Asbestos, Chemicals
Ulster Med J 2021;90(1):32-34 Medical History A SHORT HISTORY OF OCCUPATIONAL DISEASE: 2. ASBESTOS, CHEMICALS, RADIUM AND BEYOND Petts D, Wren MWD, Nation BR, Guthrie G, Kyle B, Peters L, Mortlock S, Clarke S, Burt C. ABSTRACT OCCUPATIONAL CANCER Historically, the weighing out and manipulation of dangerous Towards the end of the 18th century, a possible causal link chemicals frequently occurred without adequate protection between chemicals and cancer was reported by two London from inhalation or accidental ingestion. The use of gloves, surgeons. In 1761, John Hill reported an association between eye protection using goggles, masks or visors was scant. snuff, a tobacco product, and nasopharyngeal cancer, From Canary Girls and chimney sweeps to miners, stone and, in 1775, Percival Pott described a high incidence of cutters and silo fillers, these are classic exemplars of the subtle scrotal cancer in chimney sweeps. Pott, a surgeon at St (and in some cases not so subtle) effects that substances, Bartholomew’s Hospital in London, published his findings,6 environments and practices can have on individual health. which he attributed to contamination with soot. This excellent INTRODUCTION epidemiological study is considered to be the first report of a potential carcinogen. Pott’s work led to the foundation of It has been known for many centuries that certain diseases occupational medicine and to the Chimney Sweep Act of were associated with particular occupations (i.e. wool- 1788. In 1895, Ludwig Reyn reported that aromatic amines sorters disease in the textile industry, cowpox in milk maids used in certain dye industries in Germany were linked and respiratory problems in miners and stone workers). -

Prevention of Osteonecrosis of the Jaw (ONJ) in Patients On
Guideline Department of Health, NSW 73 Miller Street North Sydney NSW 2060 Locked Mail Bag 961 North Sydney NSW 2059 Telephone (02) 9391 9000 Fax (02) 9391 9101 http://www.health.nsw.gov.au/policies/ space space Prevention of Osteonecrosis of the Jaw (ONJ) in Patients on Bisphosphonate Therapies space Document Number GL2010_010 Publication date 23-Jul-2010 Functional Sub group Clinical/ Patient Services - Dental/Oral Clinical/ Patient Services - Pharmaceutical Clinical/ Patient Services - Medical Treatment Summary This document provides a consensus based guideline, drawing on current documented best practices, for the undertaking of invasive dental/oral surgical procedures on patients taking bisphosphonate agents so as to minimise the risk, or prevent the development of osteonecrosis of the jaws. Replaces Doc. No. Bisphosphonate Related Osteonecrosis of the Jaws - Prevention [GL2008_010] Author Branch Centre for Oral Health Strategy Branch contact Peter List 8821 4310 Applies to Area Health Services/Chief Executive Governed Statutory Health Corporation, Board Governed Statutory Health Corporations, Affiliated Health Organisations - Non Declared, Affiliated Health Organisations - Declared, Community Health Centres, Dental Schools and Clinics, Public Hospitals Audience Public Oral Health Practitioners, Medical Practitioners, Private Dental Practitioners Distributed to Public Health System, Divisions of General Practice, Government Medical Officers, NSW Ambulance Service, NSW Department of Health, Private Hospitals and Day Procedure Centres, -

Consumption, Silicosis, and the Social Construction of Industrial Disease
City University of New York (CUNY) CUNY Academic Works Publications and Research Baruch College 1991 Consumption, silicosis, and the social construction of industrial disease. D. Rosner CUNY Bernard M Baruch College G. Markowitz CUNY Bernard M Baruch College How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/bb_pubs/24 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] THE YALE JOURNAL OF BIOLOGY AND MEDICINE 64 (1991), 481-498 Consumption, Silicosis, and the Social Construction of Industrial Disease* DAVID ROSNER, Ph.D.,a AND GERALD MARKOWITZ, Ph.D." aProfessor ofHistory, Baruch College and CUNYGraduate Center, New York; "Professor ofHistory, John Jay College, City University ofNew York New York, New York Received September 10, 1991 In the wake of the bacterial revolution after Robert Koch identified the tuberculosis bacillus, medical and public health professionals classified the various forms of consumption and phthisis as a single disease-tuberculosis. In large measure, historians have adopted that perspective. While there is undoubtedly a great deal of truth in this conceptualization, we argue that it obscures almost as much as it illuminates. By collapsing the nineteenth-century terms phthisis and consumption into tuberculosis, we maintain that historians have not understood the effect of non-bacterial consumption on working-class populations who suffered from the symptoms of coughing, wasting away, and losing weight. In this essay, we explore how, in the nineteenth century, what we now recognize as silicosis was referred to as miners' "con," stonecutters' phthisis, and other industry-specific forms of phthisis and consumption. -
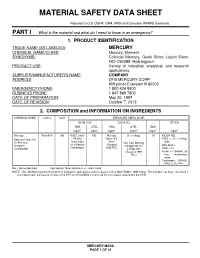
Material Safety Data Sheet
MATERIAL SAFETY DATA SHEET Prepared to U.S. OSHA, CMA, ANSI and Canadian WHMIS Standards PART I What is the material and what do I need to know in an emergency? 1. PRODUCT IDENTIFICATION TRADE NAME (AS LABELED) : MERCURY CHEMICAL NAME/CLASS : Mercury; Element SYNONYMS: Colloidal Mercury, Quick Silver; Liquid Silver; NCI-C60399; Hydrargyrum PRODUCT USE : Variety of industrial, analytical, and research applications. SUPPLIER/MANUFACTURER'S NAME : COMPANY ADDRESS : DFG MERCURY CORP 909 pitner Evanston Ill 60202 EMERGENCY PHONE : 1 800 424 9300 BUSINESS PHONE : 1 847 869 7800 DATE OF PREPARATION : May 20, 1997 DATE OF REVISION : October 7, 2013 2. COMPOSITION and INFORMATION ON INGREDIENTS CHEMICAL NAME CAS # %w/w EXPOSURE LIMITS IN AIR ACGIH-TLV OSHA-PEL OTHER TWA STEL TWA STEL IDLH mg/m 3 mg/m 3 mg/m 3 mg/m 3 mg/m 3 mg/m 3 Mercury 7439-97-6 100 0.025, (skin) NE Mercury 0.1 (ceiling) 10 NIOSH REL: Exposure limits are A4 (Not Vapor: 0.5, STEL = 0.1 (ceiling, for Mercury, Classifiable Skin; Non-alkyl Mercury skin) Inorganic as a Human (Vacated Compounds: 0.1 DFG MAKs: Compounds Carcinogen) 1989 PEL) Ceiling, skin TWA = 0.1 (Vacated 1989 PEAK = 10 •MAK 30 PEL) min., momentary value Carcinogen: EPA-D; IARC-3, TLV-A4 NE = Not Established. See Section 16 for Definitions of Terms Used. NOTE: ALL WHMIS required information is included in appropriate sections based on the ANSI Z400.1-1998 format. This product has been classified in accordance with the hazard criteria of the CPR and the MSDS contains all the information required by the CPR. -

Development of the International and Egyptian Occupational Diseases’ Lists - Review
Egyptian Journal of Occupational Medicine, 2012; 36 (2) : 215-237 DEVELOPMENT OF THE INTERNATIONAL AND EGYPTIAN OCCUPATIONAL DISEASES’ LISTS - REVIEW By Abo El-Ata GA Department of Occupational and Environmental Medicine, Faculty of Medicine, Cairo University. Abstract: An occupational disease is typically identified when it is shown that it is more prevalent in a given group of workers than in the general population, or in other worker populations. The present review study aims at eliciting development of the occupational diseases concepts and lists in Egypt and internationally, in order to anticipate the future trends in enhancing the supportive activities targeting healthcare activities of the Egyptian workers. The historical and present situation of occupational diseases are carefully reviewed and discussed, emphasizing the foot prints of related conceptions in Egypt and ILO. Future ambitions are expressed by the current study. Adopt the ILO list as well as its future amendments. In addition, re-formatting the schedule, in a similar way the ILO list is organized in three categories of occupational diseases: 1) Diseases caused by agents (chemical, physical, biological) ; 2) Diseases of target organ systems (respiratory, skin and mucous membranes, musculoskeletal, liver, kidney, endocrine, etc.) ; and 3) Occupational cancer. Restructure the basic occupational health services (BOHS) to insure provision of comprehensive and continuous benefits for every worker in his workplace. A series of guidelines and codes of practice should be issued to facilitate adoption of BOHS with detailed required procedures. The study recommended continued improving the Egyptian schedule, with establishment of proper guidelines and codes of practice to lead surveillance of the worker’s health and the workplace, an important item in basic occupational health services (BOHS). -

Complete Issue (PDF)
Abstracts Eliminating Occupational Disease: areas in the country. The study studied 40 small scale industries, and collected 40 water samples (potable) for cyanide and mer- Translating Research into Action cury which are used in mining. Questionnaire-guided interviews EPICOH 2017 and work analysis covering mining practices and risk exposures were conducted, as well as chemical analysis through gas chro- 28–31 August 2017, Edinburgh, UK matography. Results of the study showed unsafe conditions in the industries such as risk of fall during erection and dismantling of scaffolds, guard rails were not provided in scaffoldings, man- Poster Presentation ual extraction of underground ores, use of explosives, poor visi- bility in looking for ores to take out to surface, exposure to Pesticides noise from explosives, and to dust from the demolished struc- tures. Mine waste was drained into soil or ground and/or rivers and streams. The most common health problems among miners 0007 ASSESSMENT OF PESTICIDE EXPOSURE AND were hypertension (62%), followed by hypertensive cardiovascu- OCCUPATIONAL SAFETY AND HEALTH OF FARMERS IN lar disease due to left wall ischemia (14%). Health symptoms THE PHILIPPINES such as dermatitis, and peripheral neuropathy were noted and Jinky Leilanie Lu. National Institutes of Health, Institute of Health Policy and Development these can be considered as manifestations of chronic cyanide poi- Studies, University of the Philippines Manila, Manila, The Philippines soning, further, aggravated by improper use of protective equip- ment. For the environmental samples of potable water, 88% and 10.1136/oemed-2017-104636.1 98% were positive with mercury and cyanide respectively. About 52% of drinking water samples exceeded the TLV for mercury Aims This is a study conducted among 534 farmers in an while 2% exceeded the TLV for cyanide. -

At Work in the World
Perspectives in Medical Humanities At Work in the World Proceedings of the Fourth International Conference on the History of Occupational and Environmental Health Edited by Paul D. Blanc, MD and Brian Dolan, PhD Page Intentionally Left Blank At Work in the World Proceedings of the Fourth International Conference on the History of Occupational and Environmental Health Perspectives in Medical Humanities Perspectives in Medical Humanities publishes scholarship produced or reviewed under the auspices of the University of California Medical Humanities Consortium, a multi-campus collaborative of faculty, students and trainees in the humanities, medi- cine, and health sciences. Our series invites scholars from the humanities and health care professions to share narratives and analysis on health, healing, and the contexts of our beliefs and practices that impact biomedical inquiry. General Editor Brian Dolan, PhD, Professor of Social Medicine and Medical Humanities, University of California, San Francisco (ucsf) Recent Monograph Titles Health Citizenship: Essays in Social Medicine and Biomedical Politics By Dorothy Porter (Fall 2011) Paths to Innovation: Discovering Recombinant DNA, Oncogenes and Prions, In One Medical School, Over One Decade By Henry Bourne (Fall 2011) The Remarkables: Endocrine Abnormalities in Art By Carol Clark and Orlo Clark (Winter 2011) Clowns and Jokers Can Heal Us: Comedy and Medicine By Albert Howard Carter iii (Winter 2011) www.medicalhumanities.ucsf.edu [email protected] This series is made possible by the generous support of the Dean of the School of Medicine at ucsf, the Center for Humanities and Health Sciences at ucsf, and a Multi-Campus Research Program grant from the University of California Office of the President.