Coding Companion for Urology/Nephrology a Comprehensive Illustrated Guide to Coding and Reimbursement
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Partial Nephrectomy for Renal Cancer: Part I
REVIEW ARTICLE Partial nephrectomy for renal cancer: Part I BJUIBJU INTERNATIONAL Paul Russo Department of Surgery, Urology Service, and Weill Medical College, Cornell University, Memorial Sloan Kettering Cancer Center, New York, NY, USA INTRODUCTION The Problem of Kidney Cancer Kidney Cancer Is The Third Most Common Genitourinary Tumour With 57 760 New Cases And 12 980 Deaths Expected In 2009 [1]. There Are Currently Two Distinct Groups Of Patients With Kidney Cancer. The First Consists Of The Symptomatic, Large, Locally Advanced Tumours Often Presenting With Regional Adenopathy, Adrenal Invasion, And Extension Into The Renal Vein Or Inferior Vena Cava. Despite Radical Nephrectomy (Rn) In Conjunction With Regional Lymphadenectomy And Adrenalectomy, Progression To Distant Metastasis And Death From Disease Occurs In ≈30% Of These Patients. For Patients Presenting With Isolated Metastatic Disease, Metastasectomy In Carefully Selected Patients Has Been Associated With Long-term Survival [2]. For Patients With Diffuse Metastatic Disease And An Acceptable Performance Status, Cytoreductive Nephrectomy Might Add Several Additional Months Of Survival, As Opposed To Cytokine Therapy Alone, And Prepare Patients For Integrated Treatment, Now In Neoadjuvant And Adjuvant Clinical Trials, With The New Multitargeted Tyrosine Kinase Inhibitors (Sunitinib, Sorafenib) And Mtor Inhibitors (Temsirolimus, Everolimus) [3,4]. The second groups of patients with kidney overall survival. The explanation for this cancer are those with small renal tumours observation is not clear and could indicate (median tumour size <4 cm, T1a), often that aggressive surgical treatment of small incidentally discovered in asymptomatic renal masses in patients not in imminent patients during danger did not counterbalance a population imaging for of patients with increasingly virulent larger nonspecific abdominal tumours. -

Urology Services in the ASC
Urology Services in the ASC Brad D. Lerner, MD, FACS, CASC Medical Director Summit ASC President of Chesapeake Urology Associates Chief of Urology Union Memorial Hospital Urologic Consultant NFL Baltimore Ravens Learning Objectives: Describe the numerous basic and advanced urology cases/lines of service that can be provided in an ASC setting Discuss various opportunities regarding clinical, operational and financial aspects of urology lines of service in an ASC setting Why Offer Urology Services in Your ASC? Majority of urologic surgical services are already outpatient Many urologic procedures are high volume, short duration and low cost Increasing emphasis on movement of site of service for surgical cases from hospitals and insurance carriers to ASCs There are still some case types where patients are traditionally admitted or placed in extended recovery status that can be converted to strictly outpatient status and would be suitable for an ASC Potential core of fee-for-service case types (microsurgery, aesthetics, prosthetics, etc.) Increasing Population of Those Aged 65 and Over As of 2018, it was estimated that there were 51 million persons aged 65 and over (15.63% of total population) By 2030, it is expected that there will be 72.1 million persons aged 65 and over National ASC Statistics - 2017 Urology cases represented 6% of total case mix for ASCs Urology cases were 4th in median net revenue per case (approximately $2,400) – behind Orthopedics, ENT and Podiatry Urology comprised 3% of single specialty ASCs (5th behind -
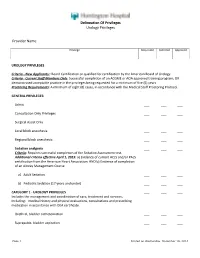
Delineation of Privileges Urology Privileges Provider Name
Delineation Of Privileges Urology Privileges Provider Name: Privilege Requested Deferred Approved UROLOGY PRIVILEGES Criteria - New Applicants:: Board Certification or qualified for certification by the American Board of Urology. Criteria - Current Staff Members Only: Successful completion of an ACGME or AOA approved training program; OR demonstrated acceptable practice in the privileges being requested for a minimum of five (5) years. Proctoring Requirements: A minimum of eight (8) cases, in accordance with the Medical Staff Proctoring Protocol. GENERAL PRIVILEGES: Admit ___ ___ ___ Consultation Only Privileges ___ ___ ___ Surgical Assist Only ___ ___ ___ Local block anesthesia ___ ___ ___ Regional block anesthesia ___ ___ ___ Sedation analgesia ___ ___ ___ Criteria: Requires successful completion of the Sedation Assessment test. Additional criteria effective April 1, 2015: a) Evidence of current ACLS and/or PALS certification from the American Heart Association; AND b) Evidence of completion of an Airway Management Course a) Adult Sedation ___ ___ ___ b) Pediatric Sedation (17 years and under) ___ ___ ___ CATEGORY 1 - UROLOGY PRIVILEGES ___ ___ ___ Includes the management and coordination of care, treatment and services, including: medical history and physical evaluations, consultations and prescribing medication in accordance with DEA certificate. Urethral, bladder catheterization ___ ___ ___ Suprapubic, bladder aspiration ___ ___ ___ Page 1 Printed on Wednesday, December 10, 2014 Delineation Of Privileges Urology Privileges Provider -

Urogenital System Surgery Urogenital System Anatomy
UROGENITAL SYSTEM SURGERY UROGENITAL SYSTEM ANATOMY Kidneys and Ureters Urinary Bladder Urethra Genital Organs Male Genital Organs Female KIDNEY and URETHERS The kidneys lie in the retroperitoneal space lateral to the aorta and the caudal vena cava. They have a fibrous capsule and are held in position by subperitoneal connective tissue. The renal pelvis is the funnel shaped structure that receives urine and directs it into the ureter. Generally, five or six diverticula curve outward from the renal pelvis. The renal artery normally bifurcates into dorsal and ventral branches; however, variations in the renal arteries and veins are common. The ureter begins at the renal pelvis and enters the dorsal surface of the bladder obliquely by means of two slit like orifices. The blood supply to the ureter is provided from the cranial ureteral artery (from the renal artery) and the caudal ureteral artery (from the prostatic or vaginal artery). Urinary bladder and urethra The bladder is divided into the trigone, which connects it to the urethra, and the body. The urethra in male dogs and cats is divided into prostatic, membranous (pelvic), and penile portions. Surgery of Kidney and Urethers Nephrectomy is excision of the kidney; nephrotomy is a surgical incision into the kidney. Pyelolithotomy is an incision into the renal pelvis and proximal ureter; a ureterotomy is an incision into the ureter; both are generally used to remove calculi. Neoureterostomy is a surgical procedure performed to correct intramural ectopic ureters; ureteroneocystostomy involves implantation of a resected ureter into the bladder. Nephrotomy to obtain tissue samples or to gain access to the renal pelvis for removal of nephroliths or other obstructive lesions. -
Methods of Urolith Removal
3 CE CE Article CREDITS Methods of Urolith Removal Cathy Langston, DVM, DACVIM (Small Animal Internal Medicine) Kelly Gisselman, DVM Douglas Palma, DVM John McCue, DVM Animal Medical Center New York, New York Abstract: Multiple techniques exist to remove uroliths from each section of the urinary tract. Minimally invasive methods for removing lower urinary tract stones include voiding urohydropropulsion, retrograde urohydropropulsion followed by dissolution or removal, catheter retrieval, cystoscopic removal, and cystoscopy-assisted laser lithotripsy and surgery. Laparoscopic cysto- tomy is less invasive than surgical cystotomy. Extracorporeal shock wave lithotripsy can be used for nephroliths and ureteroliths. Nephrotomy, pyelotomy, or urethrotomy may be recommended in certain situations. This article discusses each technique and gives guidance for selecting the most appropriate technique for an individual patient. ew, minimally invasive techniques for removing preventive measures.7 Surgical removal of partial or com- uroliths have been developed or have become more pletely obstructing ureteroliths that do not pass within 24 Nreadily available in veterinary medicine. TABLE hours may be prudent.8 A staged approach to surgery can be 1 summarizes the advantages and disadvantages of each considered if uroliths are found at multiple sites in the upper method, the number and type of uroliths for which each is urinary tract. The reversibility of renal dysfunction depends appropriate, and necessary equipment for each. on completeness and duration -

Approaches to Pyelolithotomy
Vet Times The website for the veterinary profession https://www.vettimes.co.uk APPROACHES TO PYELOLITHOTOMY Author : Nitzan Kroter Categories : Vets Date : February 14, 2011 Nitzan Kroter discusses this procedure in reference to a case involving the removal of calcium phosphate renoliths in a cat with only one functional kidney Summary A 12-year-old cat was presented for chronic weight loss. Clinical evaluation and investigation revealed an atrophied left kidney with nephroliths and an enlarged right kidney containing multiple renal calculi. Bilateral calcium phosphate renal calculi were diagnosed. This report describes pyelolithotomy in a cat. Pyelolithotomy was performed to avoid damage to the renal parenchyma, which could occur during a nephrotomy, and, therefore, minimise further damage to an already compromised kidney. Before performing surgery, consideration of the patient’s renal function is important to obtain optimal results. Maintaining normal urine production in the pre-operative and postoperative period is important in all cases. Pyelolithotomy in the dog is covered and described in the literature; the author is unaware of a detailed description of pyelolithotomy in a cat. Key words kidney, pyelolithotomy, urine 1 / 7 A NEUTERED domestic shorthaired male feline presented with a complaint of marked weight loss over the preceding few months. It weighed 2.6kg. When recorded two-and-ahalf years previously, its weight had been 5.5kg. The owner reported recent increased activity, the cat was more talkative and attention seeking, and had a normal appetite. There was no history of polydipsia or polyuria, and there had been no vomiting or diarrhoea. Clinical examination and investigation The patient had a body condition score of 2/4 and an unkempt coat, but it was responsive and alert. -
New Alternatives for Minimally Invasive Management of Uroliths: Nephroliths
3 CE Credits New Alternatives for Minimally Invasive Management of Uroliths: Nephroliths Alice Defarges, DVM, DACVIM University of Guelph Allyson Berent, DVM, DACVIM The Animal Medical Center New York, New York Marilyn Dunn, DMV, DACVIM Université de Montreal Abstract: Urolithiasis is a common clinical problem in small animal veterinary patients. Management of upper urinary tract calculi can be particularly challenging in small animals, as traditional surgical removal can be associated with significant morbidity. In humans, minimally invasive treatment options have replaced traditional surgical removal in many cases. This article reviews the current literature on the various types of lithotripsy and some of the newer minimally invasive options available for management of nephrolithiasis in small animal veterinary patients. An article in the January 2013 issue addressed management of lower urinary tract uroliths; a future article will discuss current management strategies for ureteroliths. For more information, please see the companion article: Nephrolithiasis “New Alternatives for Minimally Invasive Management of Uroliths: Many canine and feline nephroliths remain static in size and Lower Urinary Tract Uroliths” (January 2013). clinically silent for years. Some controversy still exists as to whether nonobstructive kidney stones worsen underlying kidney disease.5 rolithiasis is a common clinical problem in small animal Removal of these stones is typically recommended if the stones veterinary patients. In the past, nephroliths were treated -

Public Use Data File Documentation
Public Use Data File Documentation Part III - Medical Coding Manual and Short Index National Health Interview Survey, 1995 From the CENTERSFOR DISEASECONTROL AND PREVENTION/NationalCenter for Health Statistics U.S. DEPARTMENTOF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics CDCCENTERS FOR DlSEASE CONTROL AND PREVENTlON Public Use Data File Documentation Part Ill - Medical Coding Manual and Short Index National Health Interview Survey, 1995 U.S. DEPARTMENT OF HEALTHAND HUMAN SERVICES Centers for Disease Control and Prevention National Center for Health Statistics Hyattsville, Maryland October 1997 TABLE OF CONTENTS Page SECTION I. INTRODUCTION AND ORIENTATION GUIDES A. Brief Description of the Health Interview Survey ............. .............. 1 B. Importance of the Medical Coding ...................... .............. 1 C. Codes Used (described briefly) ......................... .............. 2 D. Appendix III ...................................... .............. 2 E, The Short Index .................................... .............. 2 F. Abbreviations and References ......................... .............. 3 G. Training Preliminary to Coding ......................... .............. 4 SECTION II. CLASSES OF CHRONIC AND ACUTE CONDITIONS A. General Rules ................................................... 6 B. When to Assign “1” (Chronic) ........................................ 6 C. Selected Conditions Coded ” 1” Regardless of Onset ......................... 7 D. When to Assign -

Ureteroscopic Treatment of Larger Renal Calculi (>2 Cm)
Thomas Jefferson University Jefferson Digital Commons Department of Urology Faculty Papers Department of Urology 9-1-2012 Ureteroscopic treatment of larger renal calculi (>2 cm). Demetrius H. Bagley Thomas Jefferson University Kelly A. Healy Thomas Jefferson University Nir Kleinmann Thomas Jefferson University Follow this and additional works at: https://jdc.jefferson.edu/urologyfp Part of the Urology Commons Let us know how access to this document benefits ouy Recommended Citation Bagley, Demetrius H.; Healy, Kelly A.; and Kleinmann, Nir, "Ureteroscopic treatment of larger renal calculi (>2 cm)." (2012). Department of Urology Faculty Papers. Paper 45. https://jdc.jefferson.edu/urologyfp/45 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in Department of Urology Faculty Papers by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. Arab Journal of Urology (2012) 10, 296–300 Arab Journal of Urology (Official Journal of the Arab -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Urolithiasis
Guidelines on Urolithiasis C. Türk (chairman), T. Knoll (vice-chairman), A. Petrik, K. Sarica, M. Straub, C. Seitz © European Association of Urology 2012 TABLE OF CONTENTS PAGE 1. METHODOLOGY 7 1.1 Introduction 7 1.2 Data identification 7 1.3 Evidence sources 7 1.4 Level of evidence and grade of recommendation 7 1.5 Publication history 8 1.5.1 Summary of changes 8 1.6 References 9 2. CLASSIFICATION OF STONES 10 2.1 Stone size 10 2.2 Stone location 10 2.3 X-ray characteristics 10 2.4 Aetiology of stone formation 10 2.5 Stone composition 10 2.6 Risk groups for stone formation 11 2.7 References 12 3. DIAGNOSIS 12 3.1 Diagnostic imaging 12 3.1.1 Evaluation of patients with acute flank pain 13 3.1.2 Evaluation of patients for whom further treatment of renal stones is planned 14 3.1.3 References 14 3.2 Diagnostics - metabolism-related 15 3.2.1 Basic analysis - non-emergency stone patients 16 3.2.2 Analysis of stone composition 16 3.3 References 17 4. TREATMENT OF PATIENTS WITH RENAL COLIC 17 4.1 Renal colic 17 4.1.1 Pain relief 17 4.1.2 Prevention of recurrent renal colic 18 4.1.3 Recommendations for analgesia during renal colic 18 4.1.4 References 18 4.2 Management of sepsis in obstructed kidney 19 4.2.1 Decompression 19 4.2.2 Further measures 20 4.2.3 References 20 5. STONE RELIEF 21 5.1 Observation of ureteral stones 21 5.1.1 Stone-passage rates 21 5.2 Observation of kidney stones 21 5.3 Medical expulsive therapy (MET) 21 5.3.1 Choice of medical agent 22 5.3.1.1 Alpha-blockers 22 5.3.1.2 Calcium-channel blockers 22 5.3.1.2.1 Tamsulosin versus -

Surgical Management of Urolithiasis in Patients After Urinary Diversion
Surgical Management of Urolithiasis in Patients after Urinary Diversion Wen Zhong1, Bicheng Yang1, Fang He2, Liang Wang3, Sunil Swami4, Guohua Zeng1* 1 Department of Urology, the First Affiliated Hospital of Guangzhou Medical University, Guangdong Key Laboratory of Urology, Guangzhou, China, 2 Department of Gynecology and Obstetrics, the Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, China, 3 Department of Biostatistics and Epidemiology, College of Public Health, East Tennessee State University, Johnson, Tennessee, United States of America, 4 Department of Epidemiology, College of Public Health and Health Professions, University of Florida, Gainesville, Florida, United States of America Abstract Objective: To present our experience in surgical management of urolithiasis in patients after urinary diversion. Patients and Methods: Twenty patients with urolithiasis after urinary diversion received intervention. Percutaneous nephrolithotomy, percutaneous based antegrade ureteroscopy with semi-rigid or flexible ureteroscope, transurethral reservoir lithotripsy, percutaneous pouch lithotripsy and open operation were performed in 8, 3, 2, 6, and 1 patients, respectively. The operative finding and complications were retrospectively collected and analyzed. Results: The mean stone size was 4.563.1 (range 1.5–11.2) cm. The mean operation time was 82.0611.5 (range 55–120) min. Eighteen patients were rendered stone free with a clearance of 90%. Complications occurred in 3 patients (15%). Two patients (10%) had postoperative fever greater than 38.5uC, and one patient (5%) suffered urine extravasations from percutaneous tract. Conclusions: The percutaneous based procedures, including percutaneous nephrolithotomy, antegrade ureteroscopy with semi-rigid ureteroscope or flexible ureteroscope from percutaneous tract, and percutaneous pouch lithotripsy, provides a direct and safe access to the target stones in patients after urinary diversion, and with high stone free rate and minor complications.