Formaldehyde Crosses the Human Placenta and Affects Human Trophoblast Differentiation and Hormonal Functions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Paleovirology of 'Syncytins', Retroviral Env Genes Exapted for a Role in Placentation
Paleovirology of ‘syncytins’, retroviral env genes exapted for a role in placentation Christian Lavialle1,2, Guillaume Cornelis1,2, Anne Dupressoir1,2, Ce´cile Esnault1,2, Odile Heidmann1,2,Ce´cile Vernochet1,2 1,2 rstb.royalsocietypublishing.org and Thierry Heidmann 1UMR 8122, Unite´ des Re´trovirus Endoge`nes et E´le´ments Re´troı¨des des Eucaryotes Supe´rieurs, CNRS, Institut Gustave Roussy, 94805 Villejuif, France 2Universite´ Paris-Sud XI, 91405 Orsay, France Review The development of the emerging field of ‘paleovirology’ allows biologists to reconstruct the evolutionary history of fossil endogenous retroviral sequences Cite this article: Lavialle C, Cornelis G, integrated within the genome of living organisms and has led to the retrieval of conserved, ancient retroviral genes ‘exapted’ by ancestral hosts to fulfil Dupressoir A, Esnault C, Heidmann O, essential physiological roles, syncytin genes being undoubtedly among the Vernochet C, Heidmann T. 2013 Paleovirology most remarkable examples of such a phenomenon. Indeed, syncytins are of ‘syncytins’, retroviral env genes exapted for a ‘new’ genes encoding proteins derived from the envelope protein of endogen- role in placentation. Phil Trans R Soc B 368: ous retroviral elements that have been captured and domesticated on multiple 20120507. occasions and independently in diverse mammalian species, through a pro- http://dx.doi.org/10.1098/rstb.2012.0507 cess of convergent evolution. Knockout of syncytin genes in mice provided evidence for their absolute requirement for placenta development and embryo survival, via formation by cell–cell fusion of syncytial cell layers at One contribution of 13 to a Theme Issue the fetal–maternal interface. -

Polyclonal Antibody to MFSD2 (C-Term) - Aff - Purified
OriGene Technologies, Inc. OriGene Technologies GmbH 9620 Medical Center Drive, Ste 200 Schillerstr. 5 Rockville, MD 20850 32052 Herford UNITED STATES GERMANY Phone: +1-888-267-4436 Phone: +49-5221-34606-0 Fax: +1-301-340-8606 Fax: +49-5221-34606-11 [email protected] [email protected] AP26290PU-N Polyclonal Antibody to MFSD2 (C-term) - Aff - Purified Alternate names: HMFN0656, Major facilitator superfamily domain-containing protein 2, PP9177 Quantity: 0.1 mg Background: Multidrug transporters, such as MFSD2A, are membrane proteins that expel a wide spectrum of cytotoxic compounds from the cell and render cells resistant to multiple drugs. Major Facilitator Superfamily (MFS) members are capable of transporting various substrates such as sugars, polyols, drugs, neurotransmitters, amino acids, peptides, and inorganic anions, although most members are substrate-specific. MFSD2A is a novel lung cancer tumor suppressor gene that regulates cell cycle progression and matrix attachment and has recently been described as the human receptor for syncytin-2, a retrovirus-derived protein mediating fusion of placental trophoblasts. MFSD2A is expressed in many tissues and is highly induced in liver and brown adipose tissue (BAT) during fasting. The activation of the betaAR signaling pathway plays a major role in the induction of MFSD2A expression during adaptive thermogenesis. Uniprot ID: Q8NA29 NCBI: NP_001129965 GeneID: 84879 Host: Rabbit Immunogen: 18 amino acid peptide near the carboxy terminus of human MFSD2A Format: State: Liquid Ig fraction Purification: Affinity chromatography purified via peptide column Buffer System: PBS containing 0.02% sodium azide Applications: ELISA. Western blot: 1 - 2 µg/ml. Positive control: Lung Tissue Lysate. -

Supplementary Data
Supplementary Fig. 1 A B Responder_Xenograft_ Responder_Xenograft_ NON- NON- Lu7336, Vehicle vs Lu7466, Vehicle vs Responder_Xenograft_ Responder_Xenograft_ Sagopilone, Welch- Sagopilone, Welch- Lu7187, Vehicle vs Lu7406, Vehicle vs Test: 638 Test: 600 Sagopilone, Welch- Sagopilone, Welch- Test: 468 Test: 482 Responder_Xenograft_ NON- Lu7860, Vehicle vs Responder_Xenograft_ Sagopilone, Welch - Lu7558, Vehicle vs Test: 605 Sagopilone, Welch- Test: 333 Supplementary Fig. 2 Supplementary Fig. 3 Supplementary Figure S1. Venn diagrams comparing probe sets regulated by Sagopilone treatment (10mg/kg for 24h) between individual models (Welsh Test ellipse p-value<0.001 or 5-fold change). A Sagopilone responder models, B Sagopilone non-responder models. Supplementary Figure S2. Pathway analysis of genes regulated by Sagopilone treatment in responder xenograft models 24h after Sagopilone treatment by GeneGo Metacore; the most significant pathway map representing cell cycle/spindle assembly and chromosome separation is shown, genes upregulated by Sagopilone treatment are marked with red thermometers. Supplementary Figure S3. GeneGo Metacore pathway analysis of genes differentially expressed between Sagopilone Responder and Non-Responder models displaying –log(p-Values) of most significant pathway maps. Supplementary Tables Supplementary Table 1. Response and activity in 22 non-small-cell lung cancer (NSCLC) xenograft models after treatment with Sagopilone and other cytotoxic agents commonly used in the management of NSCLC Tumor Model Response type -

Suppressyn Localization and Dynamic Expression Patterns in Primary Human Tissues Support a Physiologic Role in Human Placentation Jun Sugimoto1,4,5*, Danny J
www.nature.com/scientificreports OPEN Suppressyn localization and dynamic expression patterns in primary human tissues support a physiologic role in human placentation Jun Sugimoto1,4,5*, Danny J. Schust3,5, Tadatsugu Kinjo2, Yoichi Aoki2, Yoshihiro Jinno1 & Yoshiki Kudo4 We previously identifed suppressyn (SUPYN), a placental protein that negatively regulates the cell fusion essential for trophoblast syncytialization via binding to the trophoblast receptor for syncytin-1, ASCT2, and hypothesized that SUPYN may thereby regulate cell-cell fusion in the placenta. Here, we redefne in vivo SUPYN localization using specifc monoclonal antibodies in a rare early placental sample, showing SUPYN localization in villous and extravillous trophoblast subtypes, the decidua and even in placental debris in the maternal vasculature. In human trophoblast cell lines, we show SUPYN alters ASCT2 glycosylation within the secretory pathway and that this binding is associated with inhibition of cell fusion. Using newly-optimized trophoblast isolation protocols that allow tracking of ex vivo cell fusion, we present transcription and translation dynamics of fusion-related proteins over 96 hours in culture and the efects of changes in ambient oxygen levels on these processes. We report converse syncytin-1 and SUPYN transcriptional and translational responses to surrounding oxygen concentrations that suggest both are important in the efects of hypoxia and hyperoxia on placental syncytialization. Our results suggest that SUPYN’s anti-fusogenic properties may be exerted at several sites in the maternal body and its dysregulation may be associated with diseases of abnormal placentation. Tere are several types of human trophoblast cells, each with fairly well-characterized localization and function at the maternal-fetal interface. -

Retrovirology Biomed Central
Retrovirology BioMed Central Research Open Access Identification of an endogenous retroviral envelope gene with fusogenic activity and placenta-specific expression in the rabbit: a new "syncytin" in a third order of mammals Odile Heidmann†, Cécile Vernochet†, Anne Dupressoir and Thierry Heidmann* Address: Unité des Rétrovirus Endogènes et Eléments Rétroïdes des Eucaryotes Supérieurs, CNRS UMR 8122, Institut Gustave Roussy, 39 rue Camille Desmoulins, F-94805 Villejuif, and Université Paris-Sud, Orsay, F-91405, France Email: Odile Heidmann - [email protected]; Cécile Vernochet - [email protected]; Anne Dupressoir - [email protected]; Thierry Heidmann* - [email protected] * Corresponding author †Equal contributors Published: 27 November 2009 Received: 22 October 2009 Accepted: 27 November 2009 Retrovirology 2009, 6:107 doi:10.1186/1742-4690-6-107 This article is available from: http://www.retrovirology.com/content/6/1/107 © 2009 Heidmann et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: Syncytins are envelope genes of retroviral origin that have been co-opted by the host to mediate a specialized function in placentation. Two of these genes have already been identified in primates, as well as two distinct, non orthologous genes in rodents. Results: Here we identified within the rabbit Oryctolagus cuniculus-which belongs to the lagomorpha order- an envelope (env) gene of retroviral origin with the characteristic features of a bona fide syncytin, that we named syncytin-Ory1. -
93-Ethnic Differences in Frequencies of Gene Lung Cancer.Pdf
This article was originally published in a journal published by Elsevier, and the attached copy is provided by Elsevier for the author’s benefit and for the benefit of the author’s institution, for non-commercial research and educational use including without limitation use in instruction at your institution, sending it to specific colleagues that you know, and providing a copy to your institution’s administrator. All other uses, reproduction and distribution, including without limitation commercial reprints, selling or licensing copies or access, or posting on open internet sites, your personal or institution’s website or repository, are prohibited. For exceptions, permission may be sought for such use through Elsevier’s permissions site at: http://www.elsevier.com/locate/permissionusematerial Lung Cancer (2007) 55, 271—277 available at www.sciencedirect.com journal homepage: www.elsevier.com/locate/lungcan Ethnic differences in frequencies of gene polymorphisms in the MYCL1 region and modulation of lung cancer patients’ survival Monica Spinola a, F. Stefania Falvella a, Antonella Galvan a, Carmen Pignatiello a, Vera P. Leoni a, Ugo Pastorino b, Rita Paroni c, Shuqing Chen d, Vidar Skaug e, Aage Haugen e, Tommaso A. Dragani a,∗ a Department of Experimental Oncology and Laboratories, Istituto Nazionale Tumori, Milan, Italy b Unit of Thoracic Surgery, Istituto Nazionale Tumori, Via G. Venezian 1, 20133 Milan, Italy c Department of Medicine, Surgery and Dental Science, University of Milan, San Paolo Hospital, Milan, Italy d College of Pharmaceutical Sciences, Zhejiang University, Zhejiang, China e Section for Toxicology, National Institute of Occupational Health, Oslo, Norway Received 2 October 2006; received in revised form 27 October 2006; accepted 30 October 2006 KEYWORDS Summary Linkage disequilibrium (LD) analysis to refine a region associated with lung cancer Genetic progression on chromosome 1p34 identified a 106 kb LD block that includes MYCL1, TRIT1 (tRNA susceptibility; isopentenyltransferase 1) and MFSD2 (major facilitator superfamily domain-containing 2). -

UNIVERSITY of CALIFORNIA, SAN DIEGO the Proteome of Mouse
UNIVERSITY OF CALIFORNIA, SAN DIEGO The Proteome of Mouse Brain Microvessel Membranes and Basal Lamina A thesis submitted in partial satisfaction of the requirements for the degree Master of Science in Biology by Hyun Bae Chun Committee in charge: Professor Brian P. Eliceiri, Chair Professor Andrew D. Chisholm, Co-chair Professor Steven P. Briggs 2011 The Thesis of Hyun Bae Chun is approved and it is accepted in quality and form for publication on microfilm and electronically: ___________________________________________________________________ ___________________________________________________________________ Co-Chair ___________________________________________________________________ Chair University of California, San Diego 2011 iii TABLE OF CONTENTS Signature Page ………………………………….………………………………..….. iii Table of Contents …............................................................................................. iv List of Abbreviations …………………………….…………………………………… v List of Figures ………………………………………………………………………... vi List of Tables …………………………………………………………………………. vii List of Supplementary Tables ………………………………………………………. viii Acknowledgements ………………………………………………………………….. ix Abstract ……………………………………………………………………………….. x Introduction ……………………………………………………………………………. 1 Materials and Methods ……………………………………………………………….. 6 Results …………………………………………………………………………...…….. 10 Discussion ……………………………………………………………………………… 18 Figures ……………………………………………………………………………...….. 26 Tables…………………………………………………………………………………... 30 Supplementary Tables………………………………………………………………… 39 References……………………………………………………………….……………. -

Global Patterns of Changes in the Gene Expression Associated with Genesis of Cancer a Dissertation Submitted in Partial Fulfillm
Global Patterns Of Changes In The Gene Expression Associated With Genesis Of Cancer A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy at George Mason University By Ganiraju Manyam Master of Science IIIT-Hyderabad, 2004 Bachelor of Engineering Bharatiar University, 2002 Director: Dr. Ancha Baranova, Associate Professor Department of Molecular & Microbiology Fall Semester 2009 George Mason University Fairfax, VA Copyright: 2009 Ganiraju Manyam All Rights Reserved ii DEDICATION To my parents Pattabhi Ramanna and Veera Venkata Satyavathi who introduced me to the joy of learning. To friends, family and colleagues who have contributed in work, thought, and support to this project. iii ACKNOWLEDGEMENTS I would like to thank my advisor, Dr. Ancha Baranova, whose tolerance, patience, guidance and encouragement helped me throughout the study. This dissertation would not have been possible without her ever ending support. She is very sincere and generous with her knowledge, availability, compassion, wisdom and feedback. I would also like to thank Dr. Vikas Chandhoke for funding my research generously during my doctoral study at George Mason University. Special thanks go to Dr. Patrick Gillevet, Dr. Alessandro Giuliani, Dr. Maria Stepanova who devoted their time to provide me with their valuable contributions and guidance to formulate this project. Thanks to the faculty of Molecular and Micro Biology (MMB) department, Dr. Jim Willett and Dr. Monique Vanhoek in embedding valuable thoughts to this dissertation by being in my dissertation committee. I would also like to thank the present and previous doctoral program directors, Dr. Daniel Cox and Dr. Geraldine Grant, for facilitating, allowing, and encouraging me to work in this project. -

Retinal Expression of Wnt-Pathway Mediated Genes in Low- Density Lipoprotein Receptor-Related Protein 5 (Lrp5) Knockout Mice
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Harvard University - DASH Retinal Expression of Wnt-Pathway Mediated Genes in Low- Density Lipoprotein Receptor-Related Protein 5 (Lrp5) Knockout Mice The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters. Citation Chen, Jing, Andreas Stahl, Nathan M. Krah, Molly R. Seaward, Jean-Sebastian Joyal, Aimee M. Juan, Colman J. Hatton, et al. 2012. Retinal expression of Wnt-pathway mediated genes in low- density lipoprotein receptor-related protein 5 (Lrp5) knockout mice. PLoS ONE 7(1): e30203. Published Version doi:10.1371/journal.pone.0030203 Accessed February 19, 2015 9:51:39 AM EST Citable Link http://nrs.harvard.edu/urn-3:HUL.InstRepos:10021423 Terms of Use This article was downloaded from Harvard University's DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http://nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA (Article begins on next page) Retinal Expression of Wnt-Pathway Mediated Genes in Low-Density Lipoprotein Receptor-Related Protein 5 (Lrp5) Knockout Mice Jing Chen1, Andreas Stahl1,2, Nathan M. Krah1, Molly R. Seaward1, Jean-Sebastian Joyal1, Aimee M. Juan1, Colman J. Hatton1, Christopher M. Aderman1, Roberta J. Dennison1, Keirnan L. Willett1, Przemyslaw Sapieha1,3, Lois E. H. Smith1* 1 Department of Ophthalmology, Harvard Medical School, Children’s Hospital Boston, Boston, Massachusetts, United States of America, 2 University Eye Hospital Freiburg, Freiburg, Germany, 3 Department of Ophthalmology, Maisonneuve-Rosemont Hospital Research Centre, University of Montreal, Montreal, Canada Abstract Mutations in low-density lipoprotein receptor-related protein 5 (Lrp5) impair retinal angiogenesis in patients with familial exudative vitreoretinopathy (FEVR), a rare type of blinding vascular eye disease. -

Membrane Transport Across Polarized Epithelia
Downloaded from http://cshperspectives.cshlp.org/ on September 29, 2021 - Published by Cold Spring Harbor Laboratory Press Membrane Transport across Polarized Epithelia Maria Daniela Garcia-Castillo,1 Daniel J.-F. Chinnapen,1,2,3 and Wayne I. Lencer1,2,3 1Division of Gastroenterology, Boston Children’s Hospital, Boston, Massachusetts 02155 2Department of Pediatrics, Harvard Medical School, Boston, Massachusetts 02155 3Department of Pediatrics, Harvard Digestive Diseases Center, Boston, Massachusetts 02155 Correspondence: [email protected] Polarized epithelial cells line diverse surfaces throughout the body forming selective barriers between the external environment and the internal milieu. To cross these epithelial barriers, large solutes and other cargoes must undergo transcytosis, an endocytic pathway unique to polarized cell types, and significant for the development of cell polarity, uptake of viral and bacterial pathogens, transepithelial signaling, and immunoglobulin transport. Here, we review recent advances in our knowledge of the transcytotic pathway for proteins and lipids. We also discuss briefly the promise of harnessing the molecules that undergo trans- cytosis as vehicles for clinical applications in drug delivery. pithelial cells form delicate but highly effec- transcellular endocytic process termed transcy- Etive single-cell-thick barriers that define the tosis (Rojas and Apodaca 2002; Rath et al. 2014; lumen of many tissues, including all secretory Azizi et al. 2015; Tanigaki et al. 2016). Here, we organs and mucosal surfaces. Endothelial cells address new developments in our understand- form analogous single-cell-thick barriers that ing of transcytosis, the process of endosome define blood vessels and capillaries. Both cell trafficking unique to polarized cell types that types function to separate and affect vastly dif- connects one cell surface with the other. -

A De Novo 1P34.2 Microdeletion Identifies the Synaptic Vesicle Gene
Original article A de novo 1p34.2 microdeletion identifies the J Med Genet: first published as 10.1136/jmg.2008.065821 on 21 June 2009. Downloaded from synaptic vesicle gene RIMS3 as a novel candidate for autism Ravinesh A Kumar,1 Jyotsna Sudi,1 Timothy D Babatz,1 Camille W Brune,2 Donald Oswald,3 Mayon Yen,4 Norma J Nowak,5 Edwin H Cook,2 Susan L Christian,1 William B Dobyns1,6,7 < Supplementary figures and ABSTRACT including recurrent microdeletions and duplications tables are published online only Background A child with autism and mild microcephaly of 16p11.2 that have been reported in w1% of at http://jmg.bmj.com/content/ was found to have a de novo 3.3 Mb microdeletion on autism patients.81112Importantly, the discovery vol47/issue2 chromosome 1p34.2p34.3. The hypothesis is tested that of chromosomal abnormalities and CNVs has led 1 Department of Human this microdeletion contains one or more genes that to the identification of rare intragenic mutat- Genetics, University of Chicago, Chicago, Illinois, USA 2Institute underlie the autism phenotype in this child and in other ions through deep resequencing of autism candi- 13 for Juvenile Research, children with autism spectrum disorders. date genes, including NLGN3 and NLGN4, e e Department of Psychiatry, Methods To search for submicroscopic chromosomal NRXN1,10 14 15 SHANK316 18 and CNTNAP2.19 21 University of Illinois at Chicago, rearrangements in the child, array comparative genomic Although mutations in these genes account for only Chicago, Illinois, USA hybridisation (aCGH) was performed using a 19 K whole 3Department of Psychology, a small proportion of individuals with autism, they Virginia Commonwealth genome human bacterial artificial chromosome (BAC) nonetheless provide insight into potential biological University, Richmond, Virginia, array and the Illumina 610-Quad BeadChip microarray. -
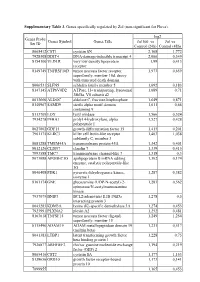
Supplementary Table 3. Genes Specifically Regulated by Zol (Non-Significant for Fluva)
Supplementary Table 3. Genes specifically regulated by Zol (non-significant for Fluva). log2 Genes Probe Genes Symbol Genes Title Zol100 vs Zol vs Set ID Control (24h) Control (48h) 8065412 CST1 cystatin SN 2,168 1,772 7928308 DDIT4 DNA-damage-inducible transcript 4 2,066 0,349 8154100 VLDLR very low density lipoprotein 1,99 0,413 receptor 8149749 TNFRSF10D tumor necrosis factor receptor 1,973 0,659 superfamily, member 10d, decoy with truncated death domain 8006531 SLFN5 schlafen family member 5 1,692 0,183 8147145 ATP6V0D2 ATPase, H+ transporting, lysosomal 1,689 0,71 38kDa, V0 subunit d2 8013660 ALDOC aldolase C, fructose-bisphosphate 1,649 0,871 8140967 SAMD9 sterile alpha motif domain 1,611 0,66 containing 9 8113709 LOX lysyl oxidase 1,566 0,524 7934278 P4HA1 prolyl 4-hydroxylase, alpha 1,527 0,428 polypeptide I 8027002 GDF15 growth differentiation factor 15 1,415 0,201 7961175 KLRC3 killer cell lectin-like receptor 1,403 1,038 subfamily C, member 3 8081288 TMEM45A transmembrane protein 45A 1,342 0,401 8012126 CLDN7 claudin 7 1,339 0,415 7993588 TMC7 transmembrane channel-like 7 1,318 0,3 8073088 APOBEC3G apolipoprotein B mRNA editing 1,302 0,174 enzyme, catalytic polypeptide-like 3G 8046408 PDK1 pyruvate dehydrogenase kinase, 1,287 0,382 isozyme 1 8161174 GNE glucosamine (UDP-N-acetyl)-2- 1,283 0,562 epimerase/N-acetylmannosamine kinase 7937079 BNIP3 BCL2/adenovirus E1B 19kDa 1,278 0,5 interacting protein 3 8043283 KDM3A lysine (K)-specific demethylase 3A 1,274 0,453 7923991 PLXNA2 plexin A2 1,252 0,481 8163618 TNFSF15 tumor necrosis