Surgical Aspects of Pulmonary Tuberculosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
National Correct Coding Initiative Policy Manual for Medicare Services Revision Date: 1/1/2019
National Correct Coding Initiative Policy Manual for Medicare Services Revision Date: 1/1/2019 Current Procedural Terminology (CPT) codes, descriptions and other data only are copyright 2018 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association. Applicable FARS\DFARS Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors, prospective payment systems, and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for the data contained or not contained herein. TABLE OF CONTENTS FOR NATIONAL CORRECT CODING INITIATIVE POLICY MANUAL FOR MEDICARE SERVICES Introduction Introduction Intro-3 Purpose Intro-3 Policy Manual Background Intro-6 Edit Development and Review Process Intro-7 Sources of Information about NCCI and MUE Intro-9 Correspondence to CMS about NCCI and its Contents Intro-10 Chapter I - General Correct Coding Policies List of Acronyms I-3 A. Introduction I-5 B. Coding Based on Standards of Medical/Surgical I-9 Practice C. Medical/Surgical Package I-12 D. Evaluation and Management (E&M) Services I-17 E. Modifiers and Modifier Indicators I-19 F. Standard Preparation/Monitoring Services for I-27 Anesthesia G. Anesthesia Service Included in the Surgical Procedure I-27 H. HCPCS/CPT Procedure Code Definition I-28 I. CPT Manual and CMS Coding Manual Instructions I-29 J. CPT “Separate Procedure” Definition I-30 K. Family of Codes I-30 L. -
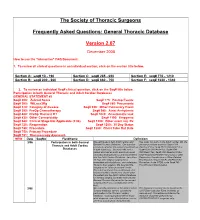
FAQ Document
The Society of Thoracic Surgeons Frequently Asked Questions: General Thoracic Database Version 2.07 December 2008 How to use the “interactive” FAQ Document: 1. To review all clinical questions in an individual section, click on the section title below. Section A: seq# 10 - 190 Section C: seq# 285 - 650 Section E: seq# 770 - 1210 Section B: seq# 200 - 260 Section D: seq# 660 - 750 Section F: seq# 1220 - 1340 2. To review an individual Seq# clinical question, click on the Seq# title below. Participation in both General Thoracic and Adult Cardiac Databases GENERAL STATEMENT #2 Seq# 200: Zubrod Score Seq# 775: Postop Events Seq# 300: WtLoss3Kg Seq# 860: Pneumonia Seq# 310: Category of disease Seq# 930: Other Pulmonary Event Seq# 390: PreOp Chemotherapy Seq# 940: Atrial Arrhythmia Seq# 400: PreOp Thoracic RT Seq# 1020: Anastomotic leak Seq# 430: Other Cormorbidity Seq# 1190: Empyema Seq# 540: Clinical Stage Not Applicable (2.06) Seq# 1200: Other event req. Rx Seq# 725: Reoperation Seq# 1250: 30 Day Status Seq# 740: Procedure Seq# 1280: Chest Tube Out Date Seq# 750: Primary Procedure Seq# 751: Thoracoscopy Approach NEW Date SeqNo FieldName Definition 3/06 Participation in both General We participate in both Adult Cardiac and Yes, enter into both. In the Adult Cardiac DB, the Thoracic and Adult Cardiac General Thoracic Database. Our question primary procedure would be Seq# 1310 pertains to whether the patient should end up OpOCard=Yes; Seq# 2510 ONCAoAn=Yes; Databases in both databases. Scenario--We had a Seq# 2530 ONCArch=Yes; Seq# 2540 patient who had an aortic aneurysm repair ONCDesc=Yes; Seq# 3220 Readm30=Yes; (arch/descending thoracic) and was entered Seq# ReadmRsn=either Pneumonia or other into the Adult Cardiac Database. -
Toman's Tuberculosis Case Detection, Treatment, and Monitoring
TOMAN’S TUBERCULOSIS TOMAN’S TUBERCULOSIS CASE DETECTION, TREATMENT, AND MONITORING The second edition of this practical, authoritative reference book provides a rational basis for the diagnosis and management of tuberculosis. Written by a number of experts in the field, it remains faithful to Kurt Toman’s original question-and-answer format, with subject matter grouped under the three headings Case detection, Treatment, and Monitoring. It is a testament to the enduring nature of the first edition that so much CASE DETECTION, TREA material has been retained unchanged. At the same time, the new edition has had not only to address the huge resurgence of tuber- culosis, the emergence of multidrug-resistant bacilli, and the special needs of HIV-infected individuals with tuberculosis, but also to encompass significant scientific advances. These changes in the profile of the disease and in approaches to management have inevitably prompted many new questions and answers and given a different complexion to others. Toman’s Tuberculosis remains essential reading for all who need to AND MONITORING TMENT, QUESTIONS learn more about every aspect of tuberculosis – case-finding, manage- ment, and effective control strategies. It provides invaluable support AND to anyone in the front line of the battle against this disease, from ANSWERS programme managers to policy-makers and from medical personnel to volunteer health workers. SECOND EDITION ISBN 92 4 154603 4 WORLD HEALTH ORGANIZATION WHO GENEVA Toman’s Tuberculosis Case detection, treatment, and monitoring – questions and answers SECOND EDITION Edited by T. Frieden WORLD HEALTH ORGANIZATION GENEVA 2004 WHO Library Cataloguing-in-Publication Data Toman’s tuberculosis case detection, treatment, and monitoring : questions and answers / edited by T. -

114.3 Cmr: Division of Health Care Finance and Policy Ambulatory Care
114.3 CMR: DIVISION OF HEALTH CARE FINANCE AND POLICY AMBULATORY CARE 114.3 CMR 40.00: RATES FOR SERVICES UNDER M.G.L. c. 152, WORKERS’ COMPENSATION ACT Section 40.01: General Provisions 40.02: General Definitions 40.03: Service and Rate Coverage Provisions 40.04: Provisions Affecting Eligible Providers 40.05: Policies for Individual Service Types 40.06: Fees 40.07: Appendices 40.08: Severability 40.01: General Provisions (1) Scope, Purpose and Effective Date. 114.3 CMR 40.00 governs the payment rates effective April 1, 2009 for purchasers of health care services under M.G.L. c. 152, the Workers’ Compensation Act. Payment rates for services provided by hospitals are set forth in 114.1 CMR 41.00. Program policies relating to medical necessity and clinical appropriateness are determined pursuant to M.G.L. c. 152 and 452 CMR 6.00. (2) Coverage. The payment rates set forth in 114.3 CMR 40.06 are full payment for services provided under M.G.L. c. 152, § 13, including any related administrative or overhead costs. The insurer, employer and health care service provider may agree upon a different payment rate for any service set forth in the fee schedule in 114.3 CMR 40.00. No employee may be held liable for the payment for health care services determined compensable under M.G.L. c. 152, § 13. (3) Administrative Bulletins. The Division may issue administrative bulletins to clarify substantive provisions of 114.3 CMR 40.00, or to publish procedure code updates and corrections. For coding updates and correction, the bulletin will list: (a) new code numbers for existing codes, with the corresponding cross references between existing and new codes numbers; (b) deleted codes for which there are no corresponding new codes; and (c) codes for entirely new services that require pricing. -

Emblemhealth's Pre-Authorization List
EmblemHealth's Pre-authorization List This is a complete list of all services requiring a Prior Approval for HIP members or a Pre-Certification for GHI members* (jointly referred to as "pre-authorization") subject to their benefit plan's coverage for all places of service, including Office (POS 11). The list accounts for EmblemHealth's medical policies, medical technology database, provider manual, and special utilization management programs. Pre-authorization is not a guarantee of payment. Payment is subject to a member's eligibility for benefits on the date of service. Emergency services do not require a pre-authorization. *GHI PPO City of New York employees and non-Medicare eligible retirees with GHI PPO benefits will be managed by Empire BCBS for inpatient and outpatient services. To see what needs authorization, use their look-up tool: https://www.empireblue.com/wps/portal/ehpprovider. CPT/ HCPCS Description Code 0008M Oncology (breast), mRNA analysis of 58 genes using hybrid capture, on formalin-fixed paraffin- embedded (FFPE) tissue, prognostic algorithm reported as a risk score 00640 Anesthesia for manipulation of the spine or for closed procedures on the cervical, thoracic or lumbar spine 0085T Breath test for heart transplant rejection 0100T Placement of a subconjunctival retinal prosthesis receiver and pulse generator, and implantation of intra-ocular retinal electrode array, with vitrectomy 0195T Arthrodesis, pre-sacral interbody technique, disc space preparation, discectomy, without instrumentation, with image guidance, includes -

Endoscopy Matrix
Endoscopy Matrix CPT Description of Endoscopy Diagnostic Therapeutic Code (Surgical) 31231 Nasal endoscopy, diagnostic, unilateral or bilateral (separate procedure) X 31233 Nasal/sinus endoscopy, diagnostic with maxillary sinusoscopy (via X inferior meatus or canine fossa puncture) 31235 Nasal/sinus endoscopy, diagnostic with sphenoid sinusoscopy (via X puncture of sphenoidal face or cannulation of ostium) 31237 Nasal/sinus endoscopy, surgical; with biopsy, polypectomy or X debridement (separate procedure) 31238 Nasal/sinus endoscopy, surgical; with control of hemorrhage X 31239 Nasal/sinus endoscopy, surgical; with dacryocystorhinostomy X 31240 Nasal/sinus endoscopy, surgical; with concha bullosa resection X 31241 Nasal/sinus endoscopy, surgical; with ligation of sphenopalatine artery X 31253 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including frontal sinus exploration, with removal of tissue from frontal sinus, when performed 31254 Nasal/sinus endoscopy, surgical; with ethmoidectomy, partial (anterior) X 31255 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior 31256 Nasal/sinus endoscopy, surgical; with maxillary antrostomy X 31257 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy 31259 Nasal/sinus endoscopy, surgical; with ethmoidectomy, total (anterior X and posterior), including sphenoidotomy, with removal of tissue from the sphenoid sinus 31267 Nasal/sinus endoscopy, surgical; with removal of -

Supplement 1
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open Supplement 1 Embase ('chronic pain'/exp OR (((chronic* OR constant* OR continu* OR persist* OR longterm OR long-term OR longstanding OR long-standing OR longlasting OR long-lasting OR phantom) NEAR/6 (pain* OR discomfort* OR complaint*)):ti,ab,kw)) AND ('postoperative pain'/exp OR (((postoperative OR posttreatment OR postsurg*) NEAR/6 (pain* OR analgesi*)) OR ((post OR after OR follow*) NEAR/3 (surg* OR operat* OR treat* OR resect* OR transplant*) NEAR/6 (pain* OR analgesi*)) OR ((post* NEAR/1 pain*)) OR pain-relief-after OR ((post-extraction OR postextraction OR amputat* OR mediastinoscopy OR sternotomy OR thoracoplasty OR thoracoscopy OR thoracostomy OR thoracotomy OR thoracocentesis OR thymectomy OR tracheostomy OR tracheotomy OR Bronchoscopy OR pneumonolysis OR pneumonectomy OR esophagectomy OR oesophagectomy OR postmediastinoscop* OR poststernotom* OR postthoracoplast* OR postthoracoscop* OR postthoracostom* OR postthoracotom* OR postthoracocentesis OR postthymectom* OR posttracheostom* OR posttracheotom* OR postbronchoscop* OR postpneumonolysis OR postpneumonectom* OR postesophagectom* OR postoesophagectom* OR postlobectom*) NEAR/6 (pain* OR discomfort OR analgesi*))):ti,ab,kw) AND (('thorax surgery'/exp NOT 'heart surgery'/exp) OR 'lung tumor'/exp/dm_su OR (((thora* OR lung OR pulmonary OR esophag* OR oesophag* OR trachea* -

Prognostic Factors for Chronic Post-Surgical Pain After Lung Or Pleural Surgery: a Protocol for a Systematic Review and Meta- Analysis
Washington University School of Medicine Digital Commons@Becker Open Access Publications 6-15-2021 Prognostic factors for chronic post-surgical pain after lung or pleural surgery: A protocol for a systematic review and meta- analysis Pascal Richard David Clephas Sanne Elisabeth Hoeks Marialena Trivella Christian S Guay Preet Mohinder Singh See next page for additional authors Follow this and additional works at: https://digitalcommons.wustl.edu/open_access_pubs Authors Pascal Richard David Clephas, Sanne Elisabeth Hoeks, Marialena Trivella, Christian S Guay, Preet Mohinder Singh, Markus Klimek, and Michael Heesen Open access Protocol BMJ Open: first published as 10.1136/bmjopen-2021-051554 on 15 June 2021. Downloaded from Prognostic factors for chronic post- surgical pain after lung or pleural surgery: a protocol for a systematic review and meta- analysis Pascal Richard David Clephas ,1 Sanne Elisabeth Hoeks ,1 Marialena Trivella ,2 Christian S Guay ,3 Preet Mohinder Singh ,3 Markus Klimek ,1 Michael Heesen4 To cite: Clephas PRD, ABSTRACT Strengths and limitations of this study Hoeks SE, Trivella M, et al. Introduction Chronic post- surgical pain (CPSP) after Prognostic factors for chronic lung or pleural surgery is a common complication and ► This systematic review and meta- analysis will be post- surgical pain after lung associated with a decrease in quality of life, long- term use or pleural surgery: a protocol the first to systematically identify all prognostic fac- of pain medication and substantial economic costs. An for a systematic review and tors for chronic post- surgical pain after lung or pleu- abundant number of primary prognostic factor studies are meta- analysis. -
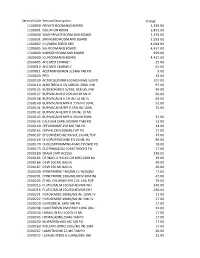
Copy of 2019 Price List for Website.Xlsx
Service Code Service Description Charge 1100000 PRIVATE ROOM AND BOARD 3,339.00 1100001 ISOLATION ROOM 3,892.00 1200000 SEMI-PRIVATE ROOM AND BOARD 3,339.00 1200001 SWINGBED ROOM AND BOARD 2,593.00 1200002 ICU/MONITORED BED 4,048.00 1200005 SIU-ROOM AND BOARD 4,457.00 1700000 NURSERY ROOM AND BOARD 959.00 2000000 ICU ROOM AND BOARD 4,457.00 2500005 AHC MED CHARGE I 25.00 2500010 AHC MED CHARGE II 65.00 2500011 ACETAMINOPHEN 325MG TAB PO 9.00 2500020 PPD 33.00 2500100 ACTIDOSE/SORB 50GM/240ML SUSPO 107.00 2500110 ALBUTEROL 0.5% NEBSOL 20ML INH 97.00 2500135 BUDESONIDE 0.5/2ML NEB SOL INH 40.00 2500137 BUPIVACAINE 0.25% INJ 10 ML IV 66.00 2500138 BUPIVACAINE 0.5% INJ 10 ML IV 69.00 2500140 BUPIVACAINE MPF 0.75% INJ 10ML 52.00 2500141 BUPIVACAINE/EPI 0.25% INJ 10ML 75.00 2500142 BUPIVACAINE/EPI 0.5% INJ 10 ML - 2500143 BUPIVACAINE MPF 0.5% INJ 30ML 47.00 2500145 CALCIUM CARB 1000MG TABS PO 13.00 2500160 CEFUROXIME 250 MG TAB PO 34.00 2500165 CEPHALEXIN 500MG CAP PO 17.00 2500167 CHLORHEXIDINE 4% SOL 240ML TOP 47.00 2500169 CHLOROPROCAINE 3% 20 ML INJ 90.00 2500170 CHOLESTRYRAMINE 4GM LT POWD PO 18.00 2500173 CLOTRIMAZOLE 10MG TROCHE PO 17.00 2500180 CRASH CART ACCESS 330.00 2500185 D5/NACL 0.9% KCL20 MEQ 1000 ML 39.00 2500186 D5W 100 ML BAG IV 40.00 2500187 D5W 250 ML BAG IV 40.00 2500200 EPINEPHRINE 1MG/ML (1:1000)INJ 17.00 2500201 EPINEPHRINE 1MG/ML MDV 30M INJ 42.00 2500205 ETHYL CHLORIDE SPR 103.1ML TOP 79.00 2500215 FLUTIC/SALM 100/50 ADVAIR INH 340.00 2500216 FLUTIC/SALM 250/50 ADVAIR INH 430.00 2500221 FUROSEMIDE 10MG/ML INJ 10ML IV -
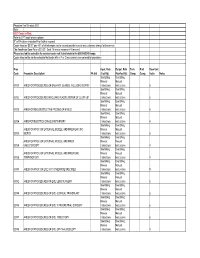
Procedure Codes Section 5
NEW YORK STATE MEDICAID PROGRAM PHYSICIAN – PROCEDURE CODES SECTION 5 - SURGERY Physician – Procedure Codes, Section 5 - Surgery _____________________________________________________________________________ Table of Contents ANESTHESIA SECTION------------------------------------------------------------------------2 GENERAL INFORMATION AND RULES------------------------------------------------2 CALCULATION OF TOTAL ANESTHESIA VALUES --------------------------------4 SURGERY SECTION ----------------------------------------------------------------------------5 GENERAL INFORMATION AND RULES------------------------------------------------5 SURGERY SERVICES ------------------------------------------------------------------------ 11 GENERAL -------------------------------------------------------------------------------------- 11 INTERGUMENTARY SYSTEM ----------------------------------------------------------- 11 MUSCULOSKELETAL SYSTEM--------------------------------------------------------- 38 RESPIRATORY SYSTEM ---------------------------------------------------------------- 108 CARDIOVASCULAR SYSTEM --------------------------------------------------------- 123 HEMIC AND LYMPHATIC SYSTEMS ------------------------------------------------ 167 MEDIASTINUM AND DIAPHRAGM --------------------------------------------------- 170 DIGESTIVE SYSTEM---------------------------------------------------------------------- 171 URINARY SYSTEM ------------------------------------------------------------------------ 214 MALE GENITAL SYSTEM --------------------------------------------------------------- -
Physician Fee Schedule 2021 Note
Physician Fee Schedule 2021 Note: 2021 Codes in Red; Refer to CPT book for descriptions R" in PA column indicates Prior Auth is required Codes listed as '$0.00" pay 45% of billed amount not to exceed provider’s usual and customary charge for the service The Anesthesia Base Rate is $15.20. Each 15 minute increment=1 time unit. Please use lab fee schedule for covered codes not listed below in the 80000-89249 range. Codes listed on the lab fee schedule that begin with a P or Q are currently non-covered for physicians Proc Inpat. Rate Outpat. Rate Tech. Prof. Base Unit Code Procedure Description PA Ind (Facility) (NonFacility) Comp. Comp. Value Notes See Billing See Billing Manual Manual 00100 ANES FOR PROCEDURES ON SALIVARY GLANDS, INCLUDING BIOPSY Instructions Instructions 5 See Billing See Billing Manual Manual 00102 ANES FOR PROCEDURES INVOLVING PLASTIC REPAIR OF CLEFT LIP Instructions Instructions 6 See Billing See Billing Manual Manual 00103 ANES FOR RECONSTRUCTIVE PROCED OF EYELID Instructions Instructions 5 See Billing See Billing Manual Manual 00104 ANES FOR ELECTROCONVULSIVE THERAPY Instructions Instructions 4 See Billing See Billing ANES FOR PROC ON EXTERNAL, MIDDLE, AND INNER EAR ,INC Manual Manual 00120 BIOPSY Instructions Instructions 5 See Billing See Billing ANES FOR PROC ON EXTERNAL, MIDDLE, AND INNER Manual Manual 00124 EAR,OTOSCOPY Instructions Instructions 4 See Billing See Billing ANES FOR PROC ON EXTERNAL, MIDDLE, AND INNER EAR, Manual Manual 00126 TYMPANOTOMY Instructions Instructions 4 See Billing See Billing Manual -

General Rate Provisions 16.04: Maximum Allowable Fees - Anesthesia Services 16.05: Maximum Allowable Fees - Surgical Services 16.06 Severability
Adopted Regulation August 31, 2012 114.3 CMR: DIVISION OF HEALTH CARE FINANCE AND POLICY AMBULATORY CARE 114.3 CMR 16.00: SURGERY AND ANESTHESIA SERVICES Section 16.01: General Provisions 16.02: General Definitions 16.03: General Rate Provisions 16.04: Maximum Allowable Fees - Anesthesia Services 16.05: Maximum Allowable Fees - Surgical Services 16.06 Severability 16.01: General Provisions (1) Scope, Purpose and Effective Date. (a) 114.3 CMR 16.00 governs the payment rates used by all governmental units for surgery and anesthesia services provided to publicly aided patients. 114.3 CMR 16.00 is effective July 1, 2012. Rates for services provided to individuals covered by M.G.L. c. 152 (the Workers' Compensation Act) are set forth at 114.3 CMR 40.00. (b) The following laboratory services have a professional and technical component. These are codes: 83020, 83912, 84165, 84166, 84181, 84182, 85390, 85576, 86255, 86256, 86320, 86325, 86327, 86334, 86335, 87164, 87207, 88371, 88372 and 89060. The professional component is contained herein. The technical component for these codes is contained in 114.3 CMR 20.00 Clinical Laboratory Services. (2) Coverage. The payment rates in 114.3 CMR 16.00 are used to pay for: (a) Surgical and anesthesia services rendered to registered bed patients in a licensed health care facility by an eligible provider who is not under contractual arrangement with the licensed health care facility for medical services and who bills separately and apart from the health care facility for medical services rendered. (b) Surgical and anesthesia services rendered to ambulatory patients in a private medical office, freestanding ambulatory surgical center, licensed clinic facility, hospital outpatient department, independent diagnostic testing facility, or other appropriate setting by an eligible provider who bills for the medical services rendered and receives no other compensation for medical services rendered.