Special Microbiology for Dummies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Culture Media Edition for Industrial Microbiology LABORATORIOS CONDA S.A
2nd Edition for Industrial Microbiology Culture Media LABORATORIOS CONDA S.A. Edited by: Laboratorios Conda S.A. © 2013. Conda S.A. All rights reserved. Printed in Spain C/ La Forja, 9 28850 - Torrejón de Ardoz, Madrid - SPAIN Tel. +34 91 761 02 00 Fax +34 91 656 82 28 C/ Berlín, 63 08029 Barcelona - SPAIN Tel. +34 93 363 72 64 / 65 Fax. +34 93 363 72 61 [email protected] [email protected] www.condalab.com Index 6 Meat & Fish Industry 20 Beer Industry 10 Water & Beverages 21 Waste Water 11 Dairy Products 23 Cosmetic Industry 15 Bakery 24 Pharmaceutical Industry 17 Processed Foods 25 Microbiology Dehydrated Culture Media Guide 19 Wines iv Media for Industrial Microbiology CULTURE MEDIA FOR INDUSTRIAL MICROBIOLOGY | 2ND EDITION Media for Industrial Microbiology 5 Culture Media for Industrial Microbiology Laboratorios CONDA, one of the world USP and AOAC standards. Strict quality leaders in the design and manufacturing of control procedures are adopted prior to, high quality culture media, currently offers during and after the manufacturing process more than 400 different products, among to ensure quality products and batch-to-batch which you will find chromogenic media, ISO- consistency. We also exert tight control over formulated media and custom-made media selection and treatment of all raw materials for many different industrial applications. and components (peptones, carbohydrates, minerals, chemicals, agar and other additives) From hygiene control, through food used in the manufacturing process. Physical- and beverage poisoning prevention, to chemical characteristics are tested, and microbiologial examination of cosmetic and media also undergo additional microbiological pharmaceutical products, CONDA supplies a tests that guarantee growth, differentiation, wide variety of different media for each field biochemical performance, recovery of small so that customers can find the most suitable inocula, selectivity, etc. -

PDF, Effect of Differences in Salt Concentration on the Quality Of
IOP Conference Series: Earth and Environmental Science PAPER • OPEN ACCESS Effect of Differences in Salt Concentration on the Quality of Rebon Shrimp Paste (Acetes Sp) in Tegal District To cite this article: S Mulyani et al 2021 IOP Conf. Ser.: Earth Environ. Sci. 755 012051 View the article online for updates and enhancements. This content was downloaded from IP address 170.106.33.19 on 26/09/2021 at 20:52 ACHOST 2020 IOP Publishing IOP Conf. Series: Earth and Environmental Science 755 (2021) 012051 doi:10.1088/1755-1315/755/1/012051 Effect of Differences in Salt Concentration on the Quality of Rebon Shrimp Paste (Acetes Sp) in Tegal District S Mulyani 1*, P M Vestiyati 1, Kusnandar 1, H K Alamsyah 1, and S W Simanjuntak 1 1Faculty of Fisheries and Marine Science, Pancasakti University of Tegal, Indonesia *[email protected] Abstract. Rebon Shrimp Paste (RSP) in Indonesia uses different percentages of salt addition, ranging from 2 to 20% or not at all. This study aims to determine the influence of different salt concentration (5%, 10%, 15% and without salt) on the quality of RSP organoleptic, microbiological and chemical. This research was conducted in Munjung Agung, Tegal and Cirebon Fisheries Product Quality Testing and Application Laboratory. The results showed that the addition of different salt concentration (5%, 10%,15% and without salt) affected the quality of organoleptics, microbiology, and chemistry. Organoleptic quality with salt concentration of 5% and 10% favored panelists with an average value of 6.8 (not yet meeting Indonesian National Standards). The highest water content value is found in RSP that are not added salt (40,19%-43,22%) and lowest at 15% salt concentration (31,12%-34,82%) in accordance with the SNI. -

Immune Effector Mechanisms and Designer Vaccines Stewart Sell Wadsworth Center, New York State Department of Health, Empire State Plaza, Albany, NY, USA
EXPERT REVIEW OF VACCINES https://doi.org/10.1080/14760584.2019.1674144 REVIEW How vaccines work: immune effector mechanisms and designer vaccines Stewart Sell Wadsworth Center, New York State Department of Health, Empire State Plaza, Albany, NY, USA ABSTRACT ARTICLE HISTORY Introduction: Three major advances have led to increase in length and quality of human life: Received 6 June 2019 increased food production, improved sanitation and induction of specific adaptive immune Accepted 25 September 2019 responses to infectious agents (vaccination). Which has had the most impact is subject to debate. KEYWORDS The number and variety of infections agents and the mechanisms that they have evolved to allow Vaccines; immune effector them to colonize humans remained mysterious and confusing until the last 50 years. Since then mechanisms; toxin science has developed complex and largely successful ways to immunize against many of these neutralization; receptor infections. blockade; anaphylactic Areas covered: Six specific immune defense mechanisms have been identified. neutralization, cytolytic, reactions; antibody- immune complex, anaphylactic, T-cytotoxicity, and delayed hypersensitivity. The role of each of these mediated cytolysis; immune immune effector mechanisms in immune responses induced by vaccination against specific infectious complex reactions; T-cell- mediated cytotoxicity; agents is the subject of this review. delayed hypersensitivity Expertopinion: In the past development of specific vaccines for infections agents was largely by trial and error. With an understanding of the natural history of an infection and the effective immune response to it, one can select the method of vaccination that will elicit the appropriate immune effector mechanisms (designer vaccines). These may act to prevent infection (prevention) or eliminate an established on ongoing infection (therapeutic). -

Medical Bacteriology
LECTURE NOTES Degree and Diploma Programs For Environmental Health Students Medical Bacteriology Abilo Tadesse, Meseret Alem University of Gondar In collaboration with the Ethiopia Public Health Training Initiative, The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education September 2006 Funded under USAID Cooperative Agreement No. 663-A-00-00-0358-00. Produced in collaboration with the Ethiopia Public Health Training Initiative, The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education. Important Guidelines for Printing and Photocopying Limited permission is granted free of charge to print or photocopy all pages of this publication for educational, not-for-profit use by health care workers, students or faculty. All copies must retain all author credits and copyright notices included in the original document. Under no circumstances is it permissible to sell or distribute on a commercial basis, or to claim authorship of, copies of material reproduced from this publication. ©2006 by Abilo Tadesse, Meseret Alem All rights reserved. Except as expressly provided above, no part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without written permission of the author or authors. This material is intended for educational use only by practicing health care workers or students and faculty in a health care field. PREFACE Text book on Medical Bacteriology for Medical Laboratory Technology students are not available as need, so this lecture note will alleviate the acute shortage of text books and reference materials on medical bacteriology. -

Food Microbiology
Food Microbiology Food Water Dairy Beverage Online Ordering Available Food, Water, Dairy, & Beverage Microbiology Table of Contents 1 Environmental Monitoring Contact Plates 3 Petri Plates 3 Culture Media for Air Sampling 4 Environmental Sampling Boot Swabs 6 Environmental Testing Swabs 8 Surface Sanitizers 8 Hand Sanitation 9 Sample Preparation - Dilution Vials 10 Compact Dry™ 12 HardyCHROM™ Chromogenic Culture Media 15 Prepared Media 24 Agar Plates for Membrane Filtration 26 CRITERION™ Dehydrated Culture Media 28 Pathogen Detection Environmental With Monitoring Contact Plates Baird Parker Agar Friction Lid For the selective isolation and enumeration of coagulase-positive staphylococci (Staphylococcus aureus) on environmental surfaces. HardyCHROM™ ECC 15x60mm contact plate, A chromogenic medium for the detection, 10/pk ................................................................................ 89407-364 differentiation, and enumeration of Escherichia coli and other coliforms from environmental surfaces (E. coli D/E Neutralizing Agar turns blue, coliforms turn red). For the enumeration of environmental organisms. 15x60mm plate contact plate, The media is able to neutralize most antiseptics 10/pk ................................................................................ 89407-354 and disinfectants that may inhibit the growth of environmental organisms. Malt Extract 15x60mm contact plate, Malt Extract is recommended for the cultivation and 10/pk ................................................................................89407-482 -

Research Journal of Pharmaceutical, Biological and Chemical Sciences
ISSN: 0975-8585 Research Journal of Pharmaceutical, Biological and Chemical Sciences Florula of Larval and Imaginal Phases of the Volfartova Fly (Wohlfarthia magnifica) In the Conditions of the Steppe Zone of The Pavlodar Region. A A Bitkeyeva1* and L T Bulekbayeva2. 1Senior teacher, Master of Ecology, Pavlodar State University named after S. Toraygyrov, The Republic of Kazakhstan. 2Associate professor, Candidate of Biological Sciences, Pavlodar State Pedagogical Institute, Republic of Kazakhstan. ABSTRACT Groups of bacteria were found during research in a steppe zone of the Pavlodar region, belonging to 3 families: Baccilaceae, Micrococcaceae, Enterobacteriacea. 13 species of pathogenic and opportunistic bacteria are obtained and identified, which cause diseases. Reception of agents from flies of Wohlfartia magnifica family in region farms forces to pay attention to quite real possibility and contagion of various infections. It creates the menacing epidemiological and epizootiology situation on the adjacent to farms of populated places, as flies with excrements can infect forages and migrate on considerable distances. Keywords: bacteria, diseases, infections, larvaes, microorganisms, flies, sheep, pathogenic microorganisms, carriers. *Corresponding author July– August 2015 RJPBCS 6(4) Page No. 2069 ISSN: 0975-8585 INTRODUCTION Flies are known as carriers of causative agents of dangerous infectious and invasive diseases. Therefore, in the populated places and on the pastures, studying of microbal and helminthosis impurity of flies represents scientific and practical interest. Epidemiological value of flies was opened by E.N. Pavlovskiy and V.P. Derbeneva-Ukhova, they participate in distribution about 70 pathogenic microflora, and including agents of a tularemia, anthrax, diphtheria, cholera, plague, a crab hand, etc. [2; 8; 12]. -
Module 2: Diphtheria
The Immunological Basis for Immunization Series Module 2: Diphtheria DEPARTMENT OF VACCINES AND BIOLOGICALS ~-) World Health Organization ~ ~ fJ! Geneva ----~ WHO/EPI/GEN/93.12 ORIGINAL: ENGLISH DISTR.: GENERAL The Immunological Basis for Immunization Series Module 2: Diphtheria Dr Artur M. Galazka Medical Officer Expanded Programme on Immunization DEPARTMENT OF VACCINES AND BIOLOGICALS .) World Health Organization ~ , ~ ~ Geneva ~ I iJff 2001 ~~ The Department of Vaccines and Biologicals thanks the donors whose unspecified financial support has made the production of this document possible. United Nations Development Fund (UNDP) The Rockefeller Foundation The Government of Sweden The Immunological Basis for Immunization series is available in English and French (from the address below). It has also been translated by national health authorities into a number of other languages for local use: Chinese, Italian, Persian, Russian, Turkish, Ukranian and Vietnamese. The series comprises eight independent modules: Module 1: General immunology Module 2: Diphtheria Module 3: Tetanus Module 4: Pertussis Module 5: Tuberculosis Module 6: Poliomyelitis Module 7: Measles Module 8: Yellow fever Produced in 1993 Reprinted (with new covers but no changes to content) in 2001 Ordering code: WHO/EPI/GEN/93.12 This document is available on the Internet at: www.who.int/vaccines-documents/ Copies may be requested from: World Health Organization Department of Vaccines and Biologicals CH-1211 Geneva 27, Switzerland • Fax: + 41 22 791 4227 • £-mail: [email protected] • ©World Health Organization 2001 This document is not a formal publication of the World Health Organization (WHO), and all rights are reserved by the Organization. The document may, however, be freely reviewed, abstracted, reproduced and translated, in part or in whole, but not for sale nor for use in conjunction with commercial purposes. -

Clinical Microbiology 12Th Edition
Volume 1 Manual of Clinical Microbiology 12th Edition Downloaded from www.asmscience.org by IP: 94.66.220.5 MCM12_FM.indd 1 On: Thu, 18 Apr 2019 08:17:55 2/12/19 6:48 PM Volume 1 Manual of Clinical Microbiology 12th Edition EDITORS-IN-CHIEF Karen C. Carroll Michael A. Pfaller Division of Medical Microbiology, Departments of Pathology and Epidemiology Department of Pathology, The Johns Hopkins (Emeritus), University of Iowa, University School of Medicine, Iowa City, and JMI Laboratories, Baltimore, Maryland North Liberty, Iowa VOLUME EDITORS Marie Louise Landry Robin Patel Laboratory Medicine and Internal Medicine, Infectious Diseases Research Laboratory, Yale University, New Haven, Connecticut Mayo Clinic, Rochester, Minnesota Alexander J. McAdam Sandra S. Richter Department of Laboratory Medicine, Boston Department of Laboratory Medicine, Children’s Hospital, Boston, Massachusetts Cleveland Clinic, Cleveland, Ohio David W. Warnock Atlanta, Georgia Washington, DC Downloaded from www.asmscience.org by IP: 94.66.220.5 MCM12_FM.indd 2 On: Thu, 18 Apr 2019 08:17:55 2/12/19 6:48 PM Volume 1 Manual of Clinical Microbiology 12th Edition EDITORS-IN-CHIEF Karen C. Carroll Michael A. Pfaller Division of Medical Microbiology, Departments of Pathology and Epidemiology Department of Pathology, The Johns Hopkins (Emeritus), University of Iowa, University School of Medicine, Iowa City, and JMI Laboratories, Baltimore, Maryland North Liberty, Iowa VOLUME EDITORS Marie Louise Landry Robin Patel Laboratory Medicine and Internal Medicine, Infectious Diseases Research Laboratory, Yale University, New Haven, Connecticut Mayo Clinic, Rochester, Minnesota Alexander J. McAdam Sandra S. Richter Department of Laboratory Medicine, Boston Department of Laboratory Medicine, Children’s Hospital, Boston, Massachusetts Cleveland Clinic, Cleveland, Ohio David W. -

BD Industry Catalog
PRODUCT CATALOG INDUSTRIAL MICROBIOLOGY BD Diagnostics Diagnostic Systems Table of Contents Table of Contents 1. Dehydrated Culture Media and Ingredients 5. Stains & Reagents 1.1 Dehydrated Culture Media and Ingredients .................................................................3 5.1 Gram Stains (Kits) ......................................................................................................75 1.1.1 Dehydrated Culture Media ......................................................................................... 3 5.2 Stains and Indicators ..................................................................................................75 5 1.1.2 Additives ...................................................................................................................31 5.3. Reagents and Enzymes ..............................................................................................75 1.2 Media and Ingredients ...............................................................................................34 1 6. Identification and Quality Control Products 1.2.1 Enrichments and Enzymes .........................................................................................34 6.1 BBL™ Crystal™ Identification Systems ..........................................................................79 1.2.2 Meat Peptones and Media ........................................................................................35 6.2 BBL™ Dryslide™ ..........................................................................................................80 -

Bismuth Sulfite Agar
Bismuth Sulfite Agar Intended Use mended for use in testing clinical specimens.15,16 In addition, Bismuth Sulfite Agar is a highly selective medium used for Bismuth Sulfite Agar is valuable when investigating outbreaks of isolating Salmonella spp., particularly Salmonella Typhi, from Salmonella spp., especially S. Typhi.17-19 food and clinical specimens. Bismuth Sulfite Agar is used for the isolation of S. Typhi and other Salmonella from food, feces, urine, sewage and other Summary and Explanation infectious materials. The typhoid organism grows luxuriantly Salmonellosis continues to be an important public health on the medium, forming characteristic black colonies, while problem worldwide, despite efforts to control the prevalence of gram-positive bacteria and members of the coliform group Salmonella in domesticated animals. Infection with nontyphi are inhibited. This inhibitory action of Bismuth Sulfite Agar Salmonella often causes mild, self-limiting illness.1 Typhoid toward gram-positive and coliform organisms permits the use fever, caused by S. Typhi, is characterized by fever, headache, of a much larger inoculum than possible with other media diarrhea and abdominal pain, and can produce fatal respi- employed for similar purposes in the past. The use of larger ratory, hepatic, splenic and/or neurological damage. These inocula greatly increases the possibility of recovering the illnesses result from consumption of raw, undercooked or pathogens, especially when they are present in relatively small improperly processed foods contaminated with Salmonella. numbers. Small numbers of organisms may be encountered in Many cases of Salmonella-related gastroenteritis are due to the early course of the disease or in the checking of carriers improper handling of poultry products. -
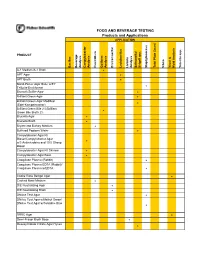
DONE Food and Beverage Testing
FOOD AND BEVERAGE TESTING Products and Applications APPLICATION PRODUCT Bacillus Beverage Analysis Campylobacter Analysis Clostridium Coliform Analysis Environmental Lactobacillus Listeria Analysis Salmonella/ Shigell spp. Staphylococcus Total Plate Count Vibrio Yeast & Mold Analysis Yersinia spp. A-1 Medium/A-1 Broth ! APT Agar ! APT Broth ! Baird-Parker Agar Base w/EY Tellurite Enrichment ! Bismuth Sulfite Agar ! Brilliant Green Agar ! Brilliant Green Agar Modified (Edel-Kampelmacher) ! Brilliant Green Bile 2%/Brilliant Green Bile Broth 2% ! Brucella Agar ! Brucella Broth ! Bryant and Burkey Medium ! Buffered Peptone Water ! Campylobacter Agar Kit Blaser/Campylobacter Agar w/5 Antimicrobics and 10% Sheep ! Blood Campylobacter Agar Kit Skirrow ! Campylobacter Agar Base ! Coagulase Plasma (Rabbit) ! Coagulase Plasma EDTA (Rabbit)/ Coagulase Plasma w/EDTA ! Cooke Rose Bengal Agar ! Cooked Meat Medium ! D/E Neutralizing Agar ! D/E Neutralizing Broth ! DNAse Test Agar ! DNAse Test Agar w/Methyl Green/ DNAse Test Agar w/Toluidine Blue ! DRBC Agar ! Demi-Fraser Broth Base ! Desoxycholate Citrate Agar Hynes ! FOOD AND BEVERAGE TESTING Products and Applications APPLICATION PRODUCT Bacillus Beverage Analysis Campylobacter Analysis Clostridium Coliform Analysis Environmental Lactobacillus Listeria Analysis Salmonella/ Shigell spp. Staphylococcus Total Plate Count Vibrio Yeast & Mold Analysis Yersinia spp. Differential Reinforced Clostridial Agar ! EC Medium/EC Broth ! EC Medium with MUG/EC Broth w/MUG ! Elliker Broth ! m Endo Agar LES ! m Endo -
Cultivation of Bacteria
CULTIVATION OF BACTERIA RAKESH SHARDA Department of Veterinary Microbiology NDVSU College of Veterinary Science & A.H., MHOW CULTIVATION OF AEROBIC BACTERIA For bacteria of veterinary importance, aerobic incubation is uniformly done at 37ºC. Depending upon the workload a laboratory may have a tabletop incubator or a walk-in incubator. For prolonged incubations, as required for the growth of Mycobacterium tuberculosis, screw-capped bottles should be used instead of Petri dishes or tubes to prevent the drying of medium. CULTIVATION OF ANAEROBIC BACTERIA Incorporation of reducing agents into the liquid medium Freshly steamed liquid media are at least temporarily anaerobic, but soon become aerobic unless a reducing agent is added.. Reducing agents include glucose 0.5-1%, ascorbic acid 0.1%, cysteine 0.1%, sodium mercaptoacetate or thioglycollate 0.1%, or the particles of meat in cooked meat broth. Examples - Thioglycollate broth, Robertson's cooked meat medium Addition of 0.05-0.1% agar can further increase the effectiveness of reducing agents Liquid media should be `pre-reduced' by holding in a boiling water bath for 10 min, to drive off dissolved oxygen Incorporation of reducing agents in Petri dish lids (Brewer’s method) a simple and safe method of obtaining anaerobiasis when using solid medium sodium dithionite (reducing agent), together with sodium bicarbonate and sodium carbonate (to supply CO2), is added in the lid of a Petri dish sodium dithionite removes the oxygen to give anaerobic conditions Displacement of oxygen by inert gases Anaerobic jar using hydrogen Most of the air from the anaerobic jar is removed and replaced with hydrogen or preferably hydrogen mixed with nitrogen in the presence of a catalyst The hydrogen reacts with the remaining oxygen to form water A common catalyst used is palladium, which should be completely dried Anaerobiasis is checked by a chemical indicator and also a bacterial indicator Metal anaerobic jar (McIntosh and Filde’s jar) 1.