Morphometry of the Foramen Ovale of Sphenoid Bone in Human Dry Skulls in Kerala
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Morfofunctional Structure of the Skull
N.L. Svintsytska V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 Ministry of Public Health of Ukraine Public Institution «Central Methodological Office for Higher Medical Education of MPH of Ukraine» Higher State Educational Establishment of Ukraine «Ukranian Medical Stomatological Academy» N.L. Svintsytska, V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 2 LBC 28.706 UDC 611.714/716 S 24 «Recommended by the Ministry of Health of Ukraine as textbook for English- speaking students of higher educational institutions of the MPH of Ukraine» (minutes of the meeting of the Commission for the organization of training and methodical literature for the persons enrolled in higher medical (pharmaceutical) educational establishments of postgraduate education MPH of Ukraine, from 02.06.2016 №2). Letter of the MPH of Ukraine of 11.07.2016 № 08.01-30/17321 Composed by: N.L. Svintsytska, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor V.H. Hryn, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor This textbook is intended for undergraduate, postgraduate students and continuing education of health care professionals in a variety of clinical disciplines (medicine, pediatrics, dentistry) as it includes the basic concepts of human anatomy of the skull in adults and newborns. Rewiewed by: O.M. Slobodian, Head of the Department of Anatomy, Topographic Anatomy and Operative Surgery of Higher State Educational Establishment of Ukraine «Bukovinian State Medical University», Doctor of Medical Sciences, Professor M.V. -

Results Description of the SKULLS. the Overall Size of Both Skulls Was Considered to Be Within Normal Limits for Their Ethnic
Ossification Defects and Craniofacial Morphology In Incomplete Forms of Mandibulofacial Dysostosis A Description of Two Dry Skulls ERIK DAHL, D.D.S., DR. ODONT. ARNE BJORK, D.D.S., ODONT. DR. Copenhagen, Denmark The morphology of two East Indian dry skulls exhibiting anomalies which were suggested to represent incomplete forms of mandibulofacial dysostosis is described. Obvious although minor ossification anomalies were found localized to the temporal, sphenoid, the zygomatic, the maxillary and the mandibular bones. The observations substantiate the concept of the regional and bilateral nature of this malformation syndrome. Bilateral orbital deviations, hypoplasia of the malar bones, and incomplete zygomatic arches appear to be hard tissue aberrations which may be helpful in exami- nation for subclinical carrier status. Changes in mandibular morphology seem to be less distinguishing features in incomplete or abortive types of mandibulofacial dysostosis. KEY WORDS craniofacial problems, mandible, mandibulofacial dysostosis, maxilla, sphenoid bone, temporal bone, zygomatic bone Mandibulofacial dysostosis (MFD) often roentgencephalometric examinations were results in the development of a characteristic made of the skulls, and tomograms were ob- facial disfigurement with considerable simi- tained of the internal and middle ear. Com- larity between affected individuals. However, parisons were made with normal adult skulls the symptoms may vary highly in respect to and with an adult skull exhibiting the char- type and degree, and both incomplete and acteristics of MFD. All of the skulls were from abortive forms of the syndrome have been the same ethnic group. ' reported in the literature (Franceschetti and Klein, 1949; Moss et al., 1964; Rogers, 1964). Results In previous papers, we have shown the DEsCRIPTION OF THE SKULLS. -

98796-Anatomy of the Orbit
Anatomy of the orbit Prof. Pia C Sundgren MD, PhD Department of Diagnostic Radiology, Clinical Sciences, Lund University, Sweden Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lay-out • brief overview of the basic anatomy of the orbit and its structures • the orbit is a complicated structure due to its embryological composition • high number of entities, and diseases due to its composition of ectoderm, surface ectoderm and mesoderm Recommend you to read for more details Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 3 x 3 Imaging technique 3 layers: - neuroectoderm (retina, iris, optic nerve) - surface ectoderm (lens) • CT and / or MR - mesoderm (vascular structures, sclera, choroid) •IOM plane 3 spaces: - pre-septal •thin slices extraconal - post-septal • axial and coronal projections intraconal • CT: soft tissue and bone windows 3 motor nerves: - occulomotor (III) • MR: T1 pre and post, T2, STIR, fat suppression, DWI (?) - trochlear (IV) - abducens (VI) Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Superior orbital fissure • cranial nerves (CN) III, IV, and VI • lacrimal nerve • frontal nerve • nasociliary nerve • orbital branch of middle meningeal artery • recurrent branch of lacrimal artery • superior orbital vein • superior ophthalmic vein Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. -

MBB: Head & Neck Anatomy
MBB: Head & Neck Anatomy Skull Osteology • This is a comprehensive guide of all the skull features you must know by the practical exam. • Many of these structures will be presented multiple times during upcoming labs. • This PowerPoint Handout is the resource you will use during lab when you have access to skulls. Mind, Brain & Behavior 2021 Osteology of the Skull Slide Title Slide Number Slide Title Slide Number Ethmoid Slide 3 Paranasal Sinuses Slide 19 Vomer, Nasal Bone, and Inferior Turbinate (Concha) Slide4 Paranasal Sinus Imaging Slide 20 Lacrimal and Palatine Bones Slide 5 Paranasal Sinus Imaging (Sagittal Section) Slide 21 Zygomatic Bone Slide 6 Skull Sutures Slide 22 Frontal Bone Slide 7 Foramen RevieW Slide 23 Mandible Slide 8 Skull Subdivisions Slide 24 Maxilla Slide 9 Sphenoid Bone Slide 10 Skull Subdivisions: Viscerocranium Slide 25 Temporal Bone Slide 11 Skull Subdivisions: Neurocranium Slide 26 Temporal Bone (Continued) Slide 12 Cranial Base: Cranial Fossae Slide 27 Temporal Bone (Middle Ear Cavity and Facial Canal) Slide 13 Skull Development: Intramembranous vs Endochondral Slide 28 Occipital Bone Slide 14 Ossification Structures/Spaces Formed by More Than One Bone Slide 15 Intramembranous Ossification: Fontanelles Slide 29 Structures/Apertures Formed by More Than One Bone Slide 16 Intramembranous Ossification: Craniosynostosis Slide 30 Nasal Septum Slide 17 Endochondral Ossification Slide 31 Infratemporal Fossa & Pterygopalatine Fossa Slide 18 Achondroplasia and Skull Growth Slide 32 Ethmoid • Cribriform plate/foramina -

Topographical Anatomy and Morphometry of the Temporal Bone of the Macaque
Folia Morphol. Vol. 68, No. 1, pp. 13–22 Copyright © 2009 Via Medica O R I G I N A L A R T I C L E ISSN 0015–5659 www.fm.viamedica.pl Topographical anatomy and morphometry of the temporal bone of the macaque J. Wysocki 1Clinic of Otolaryngology and Rehabilitation, II Medical Faculty, Warsaw Medical University, Poland, Kajetany, Nadarzyn, Poland 2Laboratory of Clinical Anatomy of the Head and Neck, Institute of Physiology and Pathology of Hearing, Poland, Kajetany, Nadarzyn, Poland [Received 7 July 2008; Accepted 10 October 2008] Based on the dissections of 24 bones of 12 macaques (Macaca mulatta), a systematic anatomical description was made and measurements of the cho- sen size parameters of the temporal bone as well as the skull were taken. Although there is a small mastoid process, the general arrangement of the macaque’s temporal bone structures is very close to that which is observed in humans. The main differences are a different model of pneumatisation and the presence of subarcuate fossa, which possesses considerable dimensions. The main air space in the middle ear is the mesotympanum, but there are also additional air cells: the epitympanic recess containing the head of malleus and body of incus, the mastoid cavity, and several air spaces on the floor of the tympanic cavity. The vicinity of the carotid canal is also very well pneuma- tised and the walls of the canal are very thin. The semicircular canals are relatively small, very regular in shape, and characterized by almost the same dimensions. The bony walls of the labyrinth are relatively thin. -

Compact Bone Spongy Bone
Spongy bone Compact bone © 2018 Pearson Education, Inc. 1 (b) Flat bone (sternum) (a) Long bone (humerus) (d) Irregular bone (vertebra), right lateral view (c) Short bone (talus) © 2018 Pearson Education, Inc. 2 Articular cartilage Proximal epiphysis Spongy bone Epiphyseal line Periosteum Compact bone Medullary cavity (lined by endosteum) Diaphysis Distal epiphysis (a) © 2018 Pearson Education, Inc. 3 Trabeculae of spongy bone Osteon (Haversian Perforating system) (Volkmann’s) canal Blood vessel continues into medullary cavity containing marrow Blood vessel Lamellae Compact bone Central (Haversian) canal Perforating (Sharpey’s) fibers Periosteum Periosteal blood vessel (a) © 2018 Pearson Education, Inc. 4 Lamella Osteocyte Canaliculus Lacuna Central Bone matrix (Haversian) canal (b) © 2018 Pearson Education, Inc. 5 Osteon Interstitial lamellae Lacuna Central (Haversian) canal (c) © 2018 Pearson Education, Inc. 6 Articular cartilage Hyaline Spongy cartilage bone New center of bone growth New bone Epiphyseal forming plate cartilage Growth Medullary in bone cavity width Bone starting Invading to replace Growth blood cartilage in bone vessels length New bone Bone collar forming Hyaline Epiphyseal cartilage plate cartilage model In an embryo In a fetus In a child © 2018 Pearson Education, Inc. 7 Bone growth Bone grows in length because: Articular cartilage 1 Cartilage grows here. Epiphyseal plate 2 Cartilage is replaced by bone here. 3 Cartilage grows here. © 2018 Pearson Education, Inc. 8 Bone remodeling Growing shaft is remodeled as: Articular cartilage Epiphyseal plate 1 Bone is resorbed by osteoclasts here. 2 Bone is added (appositional growth) by osteoblasts here. 3 Bone is resorbed by osteoclasts here. © 2018 Pearson Education, Inc. 9 Hematoma External Bony callus callus of spongy bone New Internal blood callus vessels Healed (fibrous fracture tissue and Spongy cartilage) bone trabecula 1 Hematoma 2 Fibrocartilage 3 Bony callus 4 Bone remodeling forms. -

Metrical and Non-Metrical Study of Anterior Clinoid Proces in Adult Indian Skulls Swetha.S Saveetha Dental College and Hospital
Swetha.S /J. Pharm. Sci. & Res. Vol. 7(9), 2015, 708-710 Metrical and Non-Metrical Study of Anterior Clinoid Proces in Adult Indian Skulls Swetha.S Saveetha dental college and hospital Abstract:- Background:-The complex architecture of the anterior clinoid process (ACP), which is usually removed during the surgical elimination of tumors or aneurysms of sellar region, has surgical importance. For effective clinoidectomy, a neurosurgeon must have the prior knowledge of anatmoical variations of ACP. Aim And Objective:- The purpose of this study was to investigate the dimensions and variation in the shape of ACP in dry adult skulls of Indian origin. Methods:- 30 dry adult Indian skulls will be observed .Basal width, length and thickness of ACP will be measured on both the sides using Vernier caliper. Non-metrical parameters such as shape, direction of ACP will be recorded. Reason:- Special attention should be paid to the anatomic landmarks indicating the relationship between the anterior clinoid process and adjacent structures. Beside that, pneumatization of the anterior clinoid process should be evaluated preoperatively with computed tomography to avoid complications. Keywords:- Anterior clinoid process, anatomical variations , sphenoid bone, anterior clinoidectomy INTRODUCTION:- A. Basal width- measured from lateral margin of optic The Sphenoid bone, an unpaired pneumatic bone form parts foramen to lateral margin of anterior clinoid process, on of anterior and middle cranial fossae of skull.It consists of a both right and left side.(AB line) central body,greater and lesser wings and two pterygoid B. Length of anterior clinoid process - perpendicular length processes.The lesser wings end medially to form eminences taken between apex and base.(CD line) termed as anterior clinoid processes(ACP) which are attached to the free margin of tentorium-cerebelli.(1) The anatomical relationships of the ACP, ON, chiasm, internal carotid artery (ICA), ophthalmic artery (OA) and falciform ligament (FL) are complex and represent important variations. -

(Frontal Sinus, Coronal Suture) Parietal Bone
Axial Skeleton Skull (cranium) Frontal Bone (frontal sinus, coronal suture) Parietal Bone (sagittal suture) Sphenoid Bone (sella turcica, sphenoid sinus) Temporal Bone (mastoid process, styloid process, external auditory meatus) malleus incus stapes Occipital Bone (occipital condyles, foramen magnum) Ethmoid Bone (nasal conchae, cribriform plate, crista galli, ethmoid sinus, perpendicular plate) Lacrimal Bone Zygomatic Bone Maxilla Bone (hard palate, palatine process, maxillary sinus) Palatine Bone Nasal Bone Vomer Bone Mandible Hyoid Bone Vertebral Column (general markings: body, vertebral foramen, transverse process, spinous process, superior and inferior articular processes) Cervical Vertebrae (transverse foramina) Atlas (absence of body, "yes" movement) Axis (dens, "no" movement) Thoracic Vertebrae (facets on body and transverse processes) Lumbar Vertebrae (largest) Sacral Vertebrae 5 fused vertebrae) Coccyx (3 to 5 vestigial vertebrae, body only on most) Bony Thorax Ribs (costal cartilage, true ribs, false ribs, floating ribs, facets) Sternum Manubrium Body Xiphoid Process Appendicular Skeleton Upper Limb Pectoral Girdle Scapula (acromion, coracoid process, glenoid cavity, spine) Clavicle Upper Arm Humerus (head, greater tubercle, lesser tubercle, olecranon fossa) Forearm Radius Ulna (olecranon process) Hand Carpals Metacarpals Phalanges Lower Limb Pelvic Girdle Os Coxae (sacroiliac joint, acetabulum, obturator foramen, false pelvis, difference between male and female pelvis) Ilium (iliac crest) Ischium (ischial tuberosity) Pubis (pubic symphysis) Thigh Femur (head, neck) Patella Lower Leg Tibia Fibula Foot Tarsals Metatarsals Phalanges. -
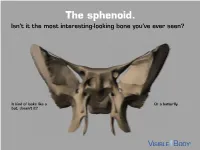
The Sphenoid. Isn’T It the Most Interesting-Looking Bone You’Ve Ever Seen?
The sphenoid. Isn’t it the most interesting-looking bone you’ve ever seen? It kind of looks like a Or a butterfly. bat, doesn’t it? The sphenoid articulates with 12 bones, both in the neurocranium and facial skeleton. The sphenoid is not just present in human skeletons, but also in mammalian ones. : A human has 1 Factoid sphenoid bone, but a dog has 8 bones that make up its sphenoid. The sphenoid is one of the 8 bones of the neurocranium (bones that protect the brain). It is the keystone* bone at the base of the skull. *In architecture, a keystone is the piece at the apex of an arch, locking all the other pieces together and bearing the weight of it all. The body of the sphenoid is the central part of the bone. It is a hollowed-out, cubical portion of the bone that forms the sphenoidal sinuses. The body is home to a deep depression known as the Sella turcica, which houses the pituitary gland. Factoid: sella turcica is Latin for “Turkish saddle” because of its resemblance to the saddles used by Turks, which had supports in the front and back. The greater wings of the sphenoid articulate with several bones, including the frontal, temporal, parietal, and zygomatic. They also serve as the attachment site for the temporalis muscles. The lesser wings are thin, triangular plates located above the greater wings. They, along with the body, form the optic canal. The optic nerve (II) passes through the optic canal to the eyes. The lateral and medial pterygoid plates project downward from the sphenoid body to give shape to the nasal cavity. -

Key Anatomical Landmarks for Middle Fossa Surgery: a Surgical Anatomy Study
LABORATORY INVESTIGATION J Neurosurg 131:1561–1570, 2019 Key anatomical landmarks for middle fossa surgery: a surgical anatomy study Maria Peris-Celda, MD, PhD,1 Avital Perry, MD,1 Lucas P. Carlstrom, MD, PhD,1 Christopher S. Graffeo, MD,1 Colin L. W. Driscoll, MD,1,2 and Michael J. Link, MD1,2 Departments of 1Neurologic Surgery and 2Otolaryngology–Head and Neck Surgery, Mayo Clinic, Rochester, Minnesota OBJECTIVE Middle fossa surgery is challenging, and reliable surgical landmarks are essential to perform accurate and safe surgery. Although many descriptions of the middle fossa components have been published, a clinically practical description of this very complex anatomical region is lacking. Small structure arrangements in this area are often not well visualized or accurately demarcated with neuronavigation systems. The objective is to describe a “roadmap” of key surgi- cal reference points and landmarks during middle fossa surgery to help the surgeon predict where critical structures will be located. METHODS The authors studied 40 dry skulls (80 sides) obtained from the anatomical board at their institution. Mea- surements of anatomical structures in the middle fossa were made with a digital caliper and a protractor, taking as refer- ence the middle point of the external auditory canal (MEAC). The results were statistically analyzed. RESULTS The petrous part of the temporal bone was found at a mean of 16 mm anterior and 24 mm posterior to the MEAC. In 87% and 99% of the sides, the foramen ovale and foramen spinosum, respectively, were encountered deep to the zygomatic root. The posterior aspect of the greater superficial petrosal nerve (GSPN) groove was a mean of 6 mm anterior and 25 mm medial to the MEAC, nearly parallel to the petrous ridge. -

The Temporal Bone: Trouble Maker in the Head Temporal Bone
The temporal bone: Trouble maker in the head Temporal bone HAROLD I. MAGOUN, SR., D.O., FAAO Belen, New Mexico function, produce tension in nerves or fascia, and generally upset homeostasis in this area. Physicians knowledgeable about osteopathic Likewise, many of the problems in the area of theory and procedures in the cranial field the eye, ear, nose, and throat have roots in have found it possible to relieve many structural abnormalities that affect the tem- conditions that result from abnormalities poral bone. Temporal bone syndromes, how- in the position and motion of temporal bones. ever, go far beyond these areas of practice. Structural deviations of these bones may be This may seem to be a questionable concept responsible for migraine headaches, vertigo, to physicians who were led to believe that the strabismus, and malocclusion of the teeth, skull is a solid ivory tower. This misconception as well as bruxism and nystagmus. has arisen because textbook writers started Correction of these deviations is not a with a false premise. Their descriptions were cure-all, but often long-standing conditions written from study of dry, defatted laboratory erroneously attributed to other causes may specimens, not of living, resilient bone. To be relieved by manipulative measures. It contemplate flexibility in a structure that does not require a great deal of training to through the ages has been considered im- perceive movement or to detect slight mobile calls for flexibility in the thinking distortions or lack of motion. process. Basic anatomy Before the position and/or motion of the tem- poral bone are considered in relation to the disorders possibly connected with abnormal- Pursuant to his observation that the spheno- ities thereof, it would be well to review the squamous suture is "beveled like the gills of a general anatomy and the physiologic move- fish and indicating articular mobility," Suther- ment involved. -

The Natural History and Pathogenesis of the Cranial Coronal Ring
The Natural History and Pathogenesis of the Cranial Coronal Ring Articulations: Implications in Understanding the Pathogenesis of the Crouzon Craniostenotic Defects ALpHonsE R. BURDI, PH.D. ADA B. KUSNETZ JoAn L. VENES, M.D. STEPHEN S. GEBARsKI, M.D. The craniostenotic birth defects seen in patients with Crouzon syn- drome have prompted this developmental study on the system of ar- ticulations between the human frontal, sphenoid, and ethmoid bones. The Crouzon facies, including midfacial hypoplasia and exorbitism, have been linked to the premature synostosis of calvarial sutures. However, considerable evidence shows that midfacial positioning is linked to increasing length of the midline cranial base. Thirty-seven typical-for-age (8 to 29 weeks) embryos were histologically prepared, read serially, and three-dimensionally reconstructed to map the so- called coronal ring articulations that continuously join the frontal, sphe- noid, and ethmoid bones. A morphologic staging plan was used to show the progressive development of bones and intervening joints. Data show that a coronal ring exists beginning at 8 weeks. Those portions of the ring separating the frontal and sphenoid bones (within the orbit and laterally along the coronal suture) show the typical structure of a five-layered suture. This sutural component of the ring is C-shaped with a cartilaginous bridge between the optic foramina completing the ring. This is the sphenoethmoidal (S-E) synchondrosis of the midline cranial base. It is suggested that this deeply located cartilage joint is the primary site of pathogenesis in the craniostenotic facies and not the coronal sutures which are operated upon. Even though the S-E cartilage would be difficult and potentially morbid to approach surgi- cally, this study would suggest that preoperative computed tomogra- phy (CT) of the skull base with special emphasis on the S-E region may provide a better prognosis regarding midface growth effects after sur- gery.