Genetic and Epigenetic Modulation of Cell Functions by Physical Exercise
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HOLOHAN-DISSERTATION-2015.Pdf (6.419Mb)
IDENTIFYING, CHARACTERIZING AND INHIBITING THE TELOMERASE REGULATORY NETWORK APPROVED BY SUPERVISORY COMMITTEE Jerry Shay, PhD Woodring Wright, MD, PhD David Corey, PhD Rolf Brekken, PhD Melanie Cobb, PhD DEDICATION Dedicated to my parents, Mark and Tracy Holohan, as well as my siblings, Kelly Nudleman and Kyle Holohan for their support and encouragement. IDENTIFYING, CHARACTERIZING AND INHIBITING THE TELOMERASE REGULATORY NETWORK by BRODY CHRISTOPHER HOLOHAN DISSERTATION / THESIS Presented to the Faculty of the Graduate School of Biomedical Sciences The University of Texas Southwestern Medical Center at Dallas In Partial Fulfillment of the Requirements For the Degree of DOCTOR OF PHILOSOPHY The University of Texas Southwestern Medical Center at Dallas Dallas, Texas May, 2015 Copyright by Brody Christopher Holohan, 2015 All Rights Reserved ACKNOWLEDGEMENTS I would like the thank my mentors, Jerry Shay and Woodring Wright for their continuous support, advice and encouragement, as well as allowing me time and resources to pursue my ideas. They are a fantastic team, and I could not have asked for better mentors. I would also like to thank my lab-mates, particularly Dr. Andrew Ludlow, Dr. Yong Zhou, Dr. Tsung-Po Lai, Dr. Oliver Delgado, Dr. Wanil Kim, Dr. Guido Stadler, Kimberly Batten, Ryan Laranger and Neal Jones. I would also like to thank Kevin Kennon for administrative support. Without my collaborators much of this would have been impossible, so I would like to thank Dr. Tim De Meyer, Dr. Abraham Aviv, Dr. Fowzan Aklayura, Dr. Steve Hunt, Dr. Tim Spector, Dr. Massimo Mangino, Dr. Daphne Friedman and Dr. Daniel Eisenberg for their help, intellectual discussions and willingness to pursue challenenging ideas. -

Replace This with the Actual Title Using All Caps
UNDERSTANDING THE GENETICS UNDERLYING MASTITIS USING A MULTI-PRONGED APPROACH A Dissertation Presented to the Faculty of the Graduate School of Cornell University In Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy by Asha Marie Miles December 2019 © 2019 Asha Marie Miles UNDERSTANDING THE GENETICS UNDERLYING MASTITIS USING A MULTI-PRONGED APPROACH Asha Marie Miles, Ph. D. Cornell University 2019 This dissertation addresses deficiencies in the existing genetic characterization of mastitis due to granddaughter study designs and selection strategies based primarily on lactation average somatic cell score (SCS). Composite milk samples were collected across 6 sampling periods representing key lactation stages: 0-1 day in milk (DIM), 3- 5 DIM, 10-14 DIM, 50-60 DIM, 90-110 DIM, and 210-230 DIM. Cows were scored for front and rear teat length, width, end shape, and placement, fore udder attachment, udder cleft, udder depth, rear udder height, and rear udder width. Independent multivariable logistic regression models were used to generate odds ratios for elevated SCC (≥ 200,000 cells/ml) and farm-diagnosed clinical mastitis. Within our study cohort, loose fore udder attachment, flat teat ends, low rear udder height, and wide rear teats were associated with increased odds of mastitis. Principal component analysis was performed on these traits to create a single new phenotype describing mastitis susceptibility based on these high-risk phenotypes. Cows (N = 471) were genotyped on the Illumina BovineHD 777K SNP chip and considering all 14 traits of interest, a total of 56 genome-wide associations (GWA) were performed and 28 significantly associated quantitative trait loci (QTL) were identified. -
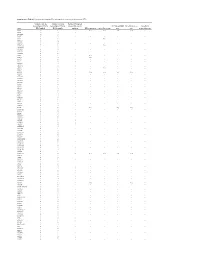
Supplementary Table S1. Prioritization of Candidate FPC Susceptibility Genes by Private Heterozygous Ptvs
Supplementary Table S1. Prioritization of candidate FPC susceptibility genes by private heterozygous PTVs Number of private Number of private Number FPC patient heterozygous PTVs in heterozygous PTVs in tumors with somatic FPC susceptibility Hereditary cancer Hereditary Gene FPC kindred BCCS samples mutation DNA repair gene Cancer driver gene gene gene pancreatitis gene ATM 19 1 - Yes Yes Yes Yes - SSPO 12 8 1 - - - - - DNAH14 10 3 - - - - - - CD36 9 3 - - - - - - TET2 9 1 - - Yes - - - MUC16 8 14 - - - - - - DNHD1 7 4 1 - - - - - DNMT3A 7 1 - - Yes - - - PKHD1L1 7 9 - - - - - - DNAH3 6 5 - - - - - - MYH7B 6 1 - - - - - - PKD1L2 6 6 - - - - - - POLN 6 2 - Yes - - - - POLQ 6 7 - Yes - - - - RP1L1 6 6 - - - - - - TTN 6 5 4 - - - - - WDR87 6 7 - - - - - - ABCA13 5 3 1 - - - - - ASXL1 5 1 - - Yes - - - BBS10 5 0 - - - - - - BRCA2 5 6 1 Yes Yes Yes Yes - CENPJ 5 1 - - - - - - CEP290 5 5 - - - - - - CYP3A5 5 2 - - - - - - DNAH12 5 6 - - - - - - DNAH6 5 1 1 - - - - - EPPK1 5 4 - - - - - - ESYT3 5 1 - - - - - - FRAS1 5 4 - - - - - - HGC6.3 5 0 - - - - - - IGFN1 5 5 - - - - - - KCP 5 4 - - - - - - LRRC43 5 0 - - - - - - MCTP2 5 1 - - - - - - MPO 5 1 - - - - - - MUC4 5 5 - - - - - - OBSCN 5 8 2 - - - - - PALB2 5 0 - Yes - Yes Yes - SLCO1B3 5 2 - - - - - - SYT15 5 3 - - - - - - XIRP2 5 3 1 - - - - - ZNF266 5 2 - - - - - - ZNF530 5 1 - - - - - - ACACB 4 1 1 - - - - - ALS2CL 4 2 - - - - - - AMER3 4 0 2 - - - - - ANKRD35 4 4 - - - - - - ATP10B 4 1 - - - - - - ATP8B3 4 6 - - - - - - C10orf95 4 0 - - - - - - C2orf88 4 0 - - - - - - C5orf42 4 2 - - - - -

Telomeres, Aging and Exercise: Guilty by Association?
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Federation ResearchOnline COPYRIGHT NOTICE FedUni ResearchOnline https://researchonline.federation.edu.au This is the published version of: Chilton, W., et.al. (2017) Telomeres, aging and exercise: Guilty by association. International Journal of Molecular Sciences, 18(12), p.1-32. Available online at https://doi.org/10.3390/ijms18122573 Copyright © 2017 Chilton, W., et.al. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0) (http://creativecommons.org/licenses/by/4.0/). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. International Journal of Molecular Sciences Review Telomeres, Aging and Exercise: Guilty by Association? Warrick Chilton 1,*, Brendan O’Brien 1 and Fadi Charchar 1,2,3,* ID 1 Faculty of Health Sciences and Faculty of Science and Technology, Federation University Australia, Ballarat, VIC 3350, Australia; [email protected] 2 Department of Physiology, University of Melbourne, Melbourne, VIC 3010, Australia 3 Department of Cardiovascular Sciences, University of Leicester, Leicester LE1 7RH, UK * Correspondence: [email protected] (W.C.); [email protected] (F.C.); Tel.: +61-3-5327-6254 (W.C.); +61-3-5327-6098 (F.C.) Received: 7 September 2017; Accepted: 25 November 2017; Published: 29 November 2017 Abstract: Telomeres are repetitive tandem DNA sequences that cap chromosomal ends protecting genomic DNA from enzymatic degradation. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

Localization of Glucokinase Gene Expression in the Rat Brain Ronald M
Localization of Glucokinase Gene Expression in the Rat Brain Ronald M. Lynch, Linda S. Tompkins, Heddwen L. Brooks, Ambrose A. Dunn-Meynell, and Barry E. Levin The brain contains a subpopulation of glucosensing neu- rons that alter their firing rate in response to elevated glucose concentrations. In pancreatic -cells, gluco- ammalian feeding behavior and general energy kinase (GK), the rate-limiting enzyme in glycolysis, medi- homeostasis appear to be regulated by circu- ates glucose-induced insulin release by regulating intra- lating levels of nutrients (glucose) and pep- cellular ATP production. A similar role for GK is pro- tides (e.g., leptin, insulin). Sensors to detect lev- posed to underlie neuronal glucosensing. Via in situ M els of these factors have been found to reside within specific hybridization, GK mRNA was localized to hypothalamic areas that are thought to contain relatively large popu- nuclei of the hypothalamus (1–8), where central regulation of lations of glucosensing neurons (the arcuate, ventrome- energy homeostasis is believed to be coordinated. For exam- dial, dorsomedial, and paraventricular nuclei and the lat- ple, large changes in blood glucose are correlated with cen- eral area). GK also was found in brain areas without trally mediated responses such as thermogenesis through known glucosensing neurons (the lateral habenula, the activation of the sympathetic nervous system. These changes bed nucleus stria terminalis, the inferior olive, the are monitored by the brain (9–11), and such responses are retrochiasmatic and medial preoptic areas, and the thal- altered in obesity-prone animals (11–13). Moreover, lesions amic posterior paraventricular, interpeduncular, oculo- of the ventromedial hypothalamus (VMH) prevent the hypo- motor, and anterior olfactory nuclei). -

A Specific N-Terminal Extension of the 8 Kda Domain Is Required for DNA End-Bridging by Human Polk and Polj
Published online 8 August 2013 Nucleic Acids Research, 2013, Vol. 41, No. 19 9105–9116 doi:10.1093/nar/gkt681 A specific N-terminal extension of the 8 kDa domain is required for DNA end-bridging by human Polk and Polj Maria Jose Martin*, Maria Victoria Garcia-Ortiz, Ana Gomez-Bedoya, Veronica Esteban, Susana Guerra and Luis Blanco* Centro de Biologia Molecular Severo Ochoa (CSIC-UAM), 28049 Madrid, Spain Received February 27, 2013; Revised July 12, 2013; Accepted July 14, 2013 ABSTRACT state [see Supplementary Figure S1A for an example with Polß; reviewed in (1)]. One role of this conformational Human DNA polymerases mu (Polk) and lambda change is to allow the rapid binding of substrates (and (Polj) are X family members involved in the repair release of products) in the open state, while inducing of double-strand breaks in DNA during non-homolo- optimal alignment of catalytic residues surrounding the gous end joining. Crucial abilities of these enzymes substrates in the closed state. The shape of the base pair include bridging of the two 30 single-stranded over- formed determines the fate of the weakly bound nucleotide hangs and trans-polymerization using one 30 end as during the conformational change step: only a correct base primer and the other as template, to minimize pair induces closing of the enzyme to form a tight catalytic sequence loss. In this context, we have studied complex; conversely, if a mismatched nucleotide is bound, the importance of a previously uncharacterised the enzyme does not close, but rather proceeds to release sequence (‘brooch’), located at the N-terminal the nucleotide while reducing the rate of catalysis. -

Rats and Axolotls Share a Common Molecular Signature After Spinal Cord Injury Enriched in Collagen-1
Rats and axolotls share a common molecular signature after spinal cord injury enriched in collagen-1 Athanasios Didangelos1, Katalin Bartus1, Jure Tica1, Bernd Roschitzki2, Elizabeth J. Bradbury1 1Wolfson CARD King’s College London, United Kingdom. 2Centre for functional Genomics, ETH Zurich, Switzerland. Running title: spinal cord injury in rats and axolotls Correspondence: A Didangelos: [email protected] SUPPLEMENTAL FIGURES AND LEGENDS Supplemental Fig. 1: Rat 7 days microarray differentially regulated transcripts. A-B: Protein-protein interaction networks of upregulated (A) and downregulated (B) transcripts identified by microarray gene expression profiling of rat SCI (4 sham versus 4 injured spinal cord samples) 7 days post-injury. Microarray expression data and experimental information is publicly available online (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE45006) and is also summarised in Supplemental Table 1. Protein-protein interaction networks were performed in StringDB using the full range of protein interaction scores (0.15 – 0.99) to capture maximum evidence of proteins’ interactions. Networks were then further analysed for betweeness centrality and gene ontology (GO) annotations (BinGO) in Cytoscape. Node colour indicates betweeness centrality while edge colour and thickness indicate interaction score based on predicted functional links between nodes (green: low values; red: high values). C-D: The top 10 upregulated (C) or downregulated (D) transcripts sorted by betweeness centrality score in protein-protein interaction networks shown in A & B. E-F: Biological process GO analysis was performed on networks of upregulated and downregulated genes using BinGO in Cytoscape. Graphs indicate the 20 most significant GO categories and the number of genes in each category. -

Lack of Rybp in Mouse Embryonic Stem Cells Impairs Cardiac Differentiation O
Page 1 of 43 1 Lack of Rybp in Mouse Embryonic Stem Cells Impairs Cardiac Differentiation O. Ujhelly1, V. Szabo2, G. Kovacs2, F. Vajda2, S. Mallok4, J. Prorok5, K. Acsai6, Z. Hegedus3, S. Krebs4, A. Dinnyes1,7 and M. K. Pirity2 * 1 BioTalentum Ltd, H-2100 Gödöllö, Hungary 2 Institute of Genetics, Biological Research Centre, Hungarian Academy of Sciences, H-6726 Szeged, Hungary 3 Institute of Biophysics, Biological Research Centre, Hungarian Academy of Sciences, H-6726 Szeged, Hungary 4 Laboratory for Functional Genome Analysis (LAFUGA), Gene Center, LMU Munich, Munich, Germany 5 Department of Pharmacology and Pharmacotherapy, University of Szeged, Szeged, Hungary 6 MTA-SZTE Research Group of Cardiovascular Pharmacology, Szeged, Hungary 7 Molecular Animal Biotechnology Laboratory, Szent Istvan University, Gödöllö, Hungary * Author for correspondence at Institute of Genetics, Biological Research Centre, Hungarian Academy of Sciences, H-6726 Szeged, Hungary Stem Cells and Development Ring1 and Yy1 Binding Protein (Rybp) has been implicated in transcriptional regulation, apoptotic signaling and as a member of the polycomb repressive complex 1 has important function in regulating pluripotency and differentiation of embryonic stem cells. Earlier, we have proven that Rybp plays essential role in mouse embryonic and central nervous system development. This work identifies Rybp, as a critical regulator of heart development. Rybp is readily detectable in the developing mouse heart from day 8.5 of embryonic development. Prominent Rybp expression persists during all embryonic stages and Rybp marks differentiated cell types of the heart. By utilizing rybp null embryonic stem cells (ESCs) in an in vitro cardiac Lack of Rybp in Mouse Embryonic Stem Cells Impairs Cardiac Differentiation (doi: 10.1089/scd.2014.0569) differentiation assay we found that rybp null ESCs do not form rhythmically beating cardiomyocytes. -

Table SII. Significantly Differentially Expressed Mrnas of GSE23558 Data Series with the Criteria of Adjusted P<0.05 And
Table SII. Significantly differentially expressed mRNAs of GSE23558 data series with the criteria of adjusted P<0.05 and logFC>1.5. Probe ID Adjusted P-value logFC Gene symbol Gene title A_23_P157793 1.52x10-5 6.91 CA9 carbonic anhydrase 9 A_23_P161698 1.14x10-4 5.86 MMP3 matrix metallopeptidase 3 A_23_P25150 1.49x10-9 5.67 HOXC9 homeobox C9 A_23_P13094 3.26x10-4 5.56 MMP10 matrix metallopeptidase 10 A_23_P48570 2.36x10-5 5.48 DHRS2 dehydrogenase A_23_P125278 3.03x10-3 5.40 CXCL11 C-X-C motif chemokine ligand 11 A_23_P321501 1.63x10-5 5.38 DHRS2 dehydrogenase A_23_P431388 2.27x10-6 5.33 SPOCD1 SPOC domain containing 1 A_24_P20607 5.13x10-4 5.32 CXCL11 C-X-C motif chemokine ligand 11 A_24_P11061 3.70x10-3 5.30 CSAG1 chondrosarcoma associated gene 1 A_23_P87700 1.03x10-4 5.25 MFAP5 microfibrillar associated protein 5 A_23_P150979 1.81x10-2 5.25 MUCL1 mucin like 1 A_23_P1691 2.71x10-8 5.12 MMP1 matrix metallopeptidase 1 A_23_P350005 2.53x10-4 5.12 TRIML2 tripartite motif family like 2 A_24_P303091 1.23x10-3 4.99 CXCL10 C-X-C motif chemokine ligand 10 A_24_P923612 1.60x10-5 4.95 PTHLH parathyroid hormone like hormone A_23_P7313 6.03x10-5 4.94 SPP1 secreted phosphoprotein 1 A_23_P122924 2.45x10-8 4.93 INHBA inhibin A subunit A_32_P155460 6.56x10-3 4.91 PICSAR P38 inhibited cutaneous squamous cell carcinoma associated lincRNA A_24_P686965 8.75x10-7 4.82 SH2D5 SH2 domain containing 5 A_23_P105475 7.74x10-3 4.70 SLCO1B3 solute carrier organic anion transporter family member 1B3 A_24_P85099 4.82x10-5 4.67 HMGA2 high mobility group AT-hook 2 A_24_P101651 -

Involvement of DNA Polymerase K in the Repair of a Specific Subset of DNA Double-Strand Breaks in Mammalian Cells
Published online 5 May 2007 Nucleic Acids Research, 2007, Vol. 35, No. 11 3551–3560 doi:10.1093/nar/gkm243 Involvement of DNA polymerase k in the repair of a specific subset of DNA double-strand breaks in mammalian cells Jean-Pascal Capp1, Franc¸ ois Boudsocq1, Anne-Gaelle Besnard1, Bernard S. Lopez2, Christophe Cazaux1, Jean-Se´ bastien Hoffmann1 and Yvan Canitrot1,* 1Genetic instability and Cancer group, Institute of Pharmacology and Structural Biology, University Paul Sabatier, UMR CNRS 5089, 205 route de Narbonne, 31077 Toulouse cedex and 2De´ partement de Radiobiologie et Radiopathologie, 60-68 av. Ge´ ne´ ral Leclerc, UMR 217 CNRS-CEA, 92265 Fontenay aux Roses cedex, France Received February 27, 2007; Revised April 2, 2007; Accepted April 3, 2007 ABSTRACT the recently discovered DNA polymerase l (poll) (2,3). Polm and poll share some homology and both have been The repair of DNA double-strand breaks (DSB) described as participating in vitro in the repair of DNA requires processing of the broken ends to complete double-strand breaks (DSB) by non-homologous end the ligation process. Recently, it has been shown joining (NHEJ) (4,5). The hallmark of animals or cells that DNA polymerase k (polk) and DNA polymerase j defective in one of the components of the NHEJ pathway (polj) are both involved in such processing during is an increased sensitivity to ionizing radiation (IR) (6–8). non-homologous end joining in vitro. However, no However, cells isolated from animals knocked out for poll phenotype was observed in animal models defective or polm do not present differences in sensitivity to any for either polk and/or polj. -

Spermatozoa Protein Alterations in Infertile Men with Bilateral Varicocele
Asian Journal of Andrology (2016) 18, 43–53 © 2016 AJA, SIMM & SJTU. All rights reserved 1008-682X www.asiaandro.com; www.ajandrology.com Open Access ORIGINAL ARTICLE Spermatozoa protein alterations in infertile men with bilateral varicocele Male Infertility Ashok Agarwal1,*, Rakesh Sharma1,*, Damayanthi Durairajanayagam1,2, Zhihong Cui1, Ahmet Ayaz1, Sajal Gupta1, Belinda Willard3, Banu Gopalan3, Edmund Sabanegh1 Among infertile men, a diagnosis of unilateral varicocele is made in 90% of varicocele cases and bilateral in the remaining varicocele cases. However, there are reports of under‑diagnosis of bilateral varicocele among infertile men and that its prevalence is greater than 10%. In this prospective study, we aimed to examine the differentially expressed proteins (DEP) extracted from spermatozoa cells of patients with bilateral varicocele and fertile donors. Subjects consisted of 17 men diagnosed with bilateral varicocele and 10 proven fertile men as healthy controls. Using the LTQ‑orbitrap elite hybrid mass spectrometry system, proteomic analysis was done on pooled samples from 3 patients with bilateral varicocele and 5 fertile men. From these samples, 73 DEP were identified of which 58 proteins were differentially expressed, with 7 proteins unique to the bilateral varicocele group and 8 proteins to the fertile control group. Majority of the DEPs were observed to be associated with metabolic processes, stress responses, oxidoreductase activity, enzyme regulation, and immune system processes. Seven DEP were involved in sperm function such as capacitation, motility, and sperm‑zona binding. Proteins TEKT3 and TCP11 were validated by Western blot analysis and may serve as potential biomarkers for bilateral varicocele. In this study, we have demonstrated for the first time the presence of DEP and identified proteins with distinct reproductive functions which are altered in infertile men with bilateral varicocele.