Faqs in Ophthalmology Aravind Faqs in Ophthalmology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fundus Signs in Temporal Arteritis
Br J Ophthalmol: first published as 10.1136/bjo.62.9.591 on 1 September 1978. Downloaded from British Journal of Ophthalmology, 1978, 62, 591-594 Fundus signs in temporal arteritis D. McLEOD, E. 0. OJI, E. M. KOHNER, AND J. MARSHALL From Moorfields Eye Hospital and Institute of Ophthalmology, London SUMMARY A patient with temporal arteritis developed a variety of ischaemic lesions in the eyes. Infarction of the inner retina and optic nerve head was delineated on presentation by white swelling in the retinal nerve fibre layer. The role of interrupted axoplasmic transport in the production of this sign is discussed. Outer retinal infarction was also noted on presentation and subsequently gave rise to striking pigmented scars. Temporal arteritis often presents with visual loss, the central venous tributaries were of normal and necropsy examination in such cases shows wide- calibre and colour. No abnormality of the inner spread disease of the ophthalmic artery and the retina was noted in the territory of supply of the extraocular course of its ciliary and retinal branches central retinal artery. (Henkind et al., 1970). The medial and lateral At first sight the left eye showed a similar ophthal- posterior ciliary arteries supply the optic nerve head, moscopic picture, with pale swelling of the nasal the outer retina, and, in 20 to 50% of individuals, part of the optic disc and a row of fluffy white by copyright. a variable area of inner retina contiguous with the cotton-wool spots crossing the papillomacular optic disc (Hayreh, 1969); the central retinal artery bundle (Fig. 2). -
RETINAL DISORDERS Eye63 (1)
RETINAL DISORDERS Eye63 (1) Retinal Disorders Last updated: May 9, 2019 CENTRAL RETINAL ARTERY OCCLUSION (CRAO) ............................................................................... 1 Pathophysiology & Ophthalmoscopy ............................................................................................... 1 Etiology ............................................................................................................................................ 2 Clinical Features ............................................................................................................................... 2 Diagnosis .......................................................................................................................................... 2 Treatment ......................................................................................................................................... 2 BRANCH RETINAL ARTERY OCCLUSION ................................................................................................ 3 CENTRAL RETINAL VEIN OCCLUSION (CRVO) ..................................................................................... 3 Pathophysiology & Etiology ............................................................................................................ 3 Clinical Features ............................................................................................................................... 3 Diagnosis ......................................................................................................................................... -

Eleventh Edition
SUPPLEMENT TO April 15, 2009 A JOBSON PUBLICATION www.revoptom.com Eleventh Edition Joseph W. Sowka, O.D., FAAO, Dipl. Andrew S. Gurwood, O.D., FAAO, Dipl. Alan G. Kabat, O.D., FAAO Supported by an unrestricted grant from Alcon, Inc. 001_ro0409_handbook 4/2/09 9:42 AM Page 4 TABLE OF CONTENTS Eyelids & Adnexa Conjunctiva & Sclera Cornea Uvea & Glaucoma Viitreous & Retiina Neuro-Ophthalmic Disease Oculosystemic Disease EYELIDS & ADNEXA VITREOUS & RETINA Blow-Out Fracture................................................ 6 Asteroid Hyalosis ................................................33 Acquired Ptosis ................................................... 7 Retinal Arterial Macroaneurysm............................34 Acquired Entropion ............................................. 9 Retinal Emboli.....................................................36 Verruca & Papilloma............................................11 Hypertensive Retinopathy.....................................37 Idiopathic Juxtafoveal Retinal Telangiectasia...........39 CONJUNCTIVA & SCLERA Ocular Ischemic Syndrome...................................40 Scleral Melt ........................................................13 Retinal Artery Occlusion ......................................42 Giant Papillary Conjunctivitis................................14 Conjunctival Lymphoma .......................................15 NEURO-OPHTHALMIC DISEASE Blue Sclera .........................................................17 Dorsal Midbrain Syndrome ..................................45 -

Erounds on Wednesday Mornings, the West LA VA Optometry Residents & Student Participate in Erounds
West Los Angeles VA Health Care Center, Los Angeles, CA eRounds On Wednesday mornings, the West LA VA Optometry residents & student participate in eRounds. An eRounds typically includes presentation of one or more illustrative cases of the condition under consideration. During the case presentations, trainees are asked to identify normal and abnormal findings, list ocular differential diagnoses, list systemic differential diagnoses when applicable, and state options for ocular (and systemic) management. This is usually followed by a presentation of information on the topic, which may include epidemiology, presenting signs and symptoms of the condition, clinical diagnostic testing, ancillary testing, ocular and systemic management, etc. Topics include: Acne rosacea Conjunctival actinic keratosis Conjunctivochalasis Entropion and ectropion Floppy eyelid syndrome Fat prolapse Herpetic eye disease Hyphema Neovascular glaucoma Corneal degenerations Squamous cell carcinoma of the eyelid Basal cell carcinoma of the eyelid Sebaceous carcinoma Pemphigoid Phthisis bulbi Ocular manifestations of Valsalva maneuver Xanthelasma Branch retinal artery occlusion Central retinal artery occlusion Giant cell arteritis Fibrinoplatelet retinal embolus Ophthalmic artery occlusion Multiple Hollenhorst plaques Solitary Hollenhorst plaque Best dystrophy Retinitis pigmentosa Cone-rod dystrophies Optic disc drusen Tilted disc syndrome Stargardt’s disease Diabetic retinopathy Diabetes mellitus and ocular media disorders Diabetes mellitus and neuro-ophthalmic disease -

PG Series Ophthalmology Buster
PG Series Ophthalmology Buster PG Series Ophthalmology Buster E Ahmed Formerly Head, Department of Ophthalmology Calcutta National Medical College Consultant, Eye Care and Research Centre Kolkata JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD New Delhi Published by Jitendar P Vij Jaypee Brothers Medical Publishers (P) Ltd B-3, EMCA House, 23/23B Ansari Road, Daryaganj New Delhi 110 002, India Phones: +91-11-23272143, +91-11-23272703, +91-11-23282021, +91-11-23245672, Rel: 32558559 Fax: +91-11-23276490, +91-11-23245683 e-mail: [email protected] Visit our website: www.jaypeebrothers.com Branches • 2/B, Akruti Society, Jodhpur Gam Road Satellite, Ahmedabad 380 015 Phones: +91-079-26926233, Rel: +91-079-32988717, Fax: +91-079-26927094 e-mail: [email protected] • 202 Batavia Chambers, 8 Kumara Krupa Road, Kumara Park East, Bangalore 560 001 Phones: +91-80-22285971, +91-80-22382956, Rel: +91-80-32714073, Fax: +91-80-22281761 e-mail: [email protected] • 282 IIIrd Floor, Khaleel Shirazi Estate, Fountain Plaza, Pantheon Road, Chennai 600 008 Phones: +91-44-28193265, +91-44-28194897, Rel: +91-44-32972089 Fax: +91-44-28193231 e-mail: [email protected] • 4-2-1067/1-3, 1st Floor, Balaji Building, Ramkote Cross Road, Hyderabad 500 095 Phones: +91-40-66610020, +91-40-24758498, Rel:+91-40-32940929 Fax:+91-40-24758499, e-mail: [email protected] • No. 41/3098, B & B1, Kuruvi Building, St. Vincent Road, Kochi 682 018, Kerala Phones: +91-0484-4036109, +91-0484-2395739, +91-0484-2395740 e-mail: [email protected] • 1-A Indian Mirror Street, Wellington Square, Kolkata 700 013 Phones: +91-33-22451926, +91-33-22276404, +91-33-22276415, Rel: +91-33-32901926 Fax: +91-33-22456075, e-mail: [email protected] • 106 Amit Industrial Estate, 61 Dr SS Rao Road, Near MGM Hospital, Parel, Mumbai 400 012 Phones: +91-22-24124863, +91-22-24104532, Rel: +91-22-32926896 Fax: +91-22-24160828, e-mail: [email protected] • “KAMALPUSHPA” 38, Reshimbag, Opp. -

20-OPHTHALMOLOGY Cataract-Ds Brushfield-Down Synd Christmas
20-OPHTHALMOLOGY cataract-ds BrushfielD-Down synd christmas tree-myotonic dystrophy coronaRY-pubeRtY cuneiform-cortical(polyopia) cupuliform-post subcapsular(max vision loss) Elschnig pearl, ring of Soemmering-after(post capsule) experimenTal-Tyr def glassworker-infrared radiation grey(soft), yellow, amber, red(cataracta rubra), brown(cataracta brunescence), black(cat nigrans)(GYARBB)-nuclear(hard) heat-ionising radiation Membranous-HallerMan Streiff synd morgagnian-hypermature senile oildrop(revers)-galactossemia(G1PUT def) post cortical/bread crumb/polychromatic lustre/rainbow-complicated post polar-PHPV(persistent hyperplastic prim vitreous) radiational-post subcapsular riders-zonular/lamellar(vitD def, hypoparathy) roseTTe(ant cortex)-Trauma, concussion shield-atopic dermatitis snowstorm/flake-juvenile DM(aldose reductase def, T1>T2, sorbitol accumulat) star-electrocution sunflower/flower of petal-Wilson ds, chalcosis, penetrating trauma syndermatotic-atopic ds total-cong rubella zonular-galactossemia(galactokinase def) stage of cataract lamellar separation incipient/intumescence(freq change of glass) immature mature hypermature Aim4aiims.inmorgagnian sclerotic lens layer ant capsule ant epithelium lens fibre[66%H2O, 34%prot-aLp(Largest), Bet(most aBundant), γ(crystalline, soluble)] nucleus embryonic(0-3mthIUL) fetal(3-8mthIUL)-Y shape(suture) infantile(8mthIUL-puberty) adult(>puberty) cortex post capsule thinnest-post pole>ant pole thickest, most active cell-equator vitA absent in lens vitC tpt in lens by myoinositol H2O tpt in lens -

Amaurosis Fugax (Transient Monocular Or Binocular Vision Loss)
Amaurosis fugax (transient monocular or binocular vision loss) Syndee Givre, MD, PhD Gregory P Van Stavern, MD The next version of UpToDate (15.3) will be released in October 2007. INTRODUCTION AND DEFINITIONS — Amaurosis fugax (from the Greek "amaurosis," meaning dark, and the Latin "fugax," meaning fleeting) refers to a transient loss of vision in one or both eyes. Varied use of common terminology may cause some confusion when reading the literature. Some suggest that "amaurosis fugax" implies a vascular cause for the visual loss, but the term continues to be used when describing visual loss from any origin and involving one or both eyes. The term "transient monocular blindness" is also often used but is not ideal, since most patients do not experience complete loss of vision with the episode. "Transient monocular visual loss" (TMVL) and "transient binocular visual loss" (TBVL) are preferred to describe abrupt and temporary loss of vision in one or both eyes, since they carry no connotation regarding etiology. Transient visual loss, either monocular or binocular, reflects a heterogeneous group of disorders, some relatively benign and others with grave neurologic or ophthalmologic implications. The task of the clinician is to use the history and examination to localize the problem to a region in the visual pathways, identify potential etiologies, and, when indicated, perform a focused battery of laboratory tests to confirm or exclude certain causes. Therapeutic interventions and prognostic implications are specific to the underlying cause. This topic discusses transient visual loss. Other ocular and cerebral ischemic syndromes are discussed separately. APPROACH TO TRANSIENT VISUAL LOSS — By definition, patients with transient visual loss almost always present after the episode has resolved; hence, the neurologic and ophthalmologic examination is usually normal. -

Systemic Disease with a Twist of Neuro
6/14/2021 Systemic Disease Straight Up…. AOA’s definition of Optometry approved Sept 2012 with a Twist of Neuro! Doctors of optometry (ODs) are the independent primary health care Beth A. Steele, OD, FAAO professionals for the eye. Optometrists examine, diagnose, treat, and [email protected] manage diseases, injuries, and disorders of the visual system, the eye, and associated structures as well as identify related systemic conditions affecting the eye. PREVENTION Not just this… TREATING THE WHOLE PATIENT But also this… MEDICAL OPTOMETRY …..where do we fit in? 1 6/14/2021 29 AA F Hx ESRD, on dialysis Blood Pressure Classifications and Referral Guidelines (adapted from the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure –JNC 7, no symptoms, visual or systemic 2003) Hypotension normal Pre‐ HTN Stage 1Stage 2 Critical High Point Systolic < 90 < 120 120‐139 140‐ 159 ≥160 >180 Diastolic < 60 < 80 80 ‐ 89 90‐99 ≥100 >110 Refer Refer Evaluate or refer From: 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report From the Panel Members within 2 within 1 immediately or BP 159/116 Appointed to the Eighth Joint National Committee (JNC 8) months month within 1 week JNC vs. ACC/AHA Guidelines All values ~10mmHg lower than JNC • 2017 ACC/AHA Clinical Practice Guidelines lowered thresholds by 10mmHg for diagnosis and treatment goals! • 26% increase in US prevalence HTN • Very controversial 2 6/14/2021 Atherosclerotic cardiovascular disease (ASCVD) risk calculator • 10‐year risk of CVD • http://tools.acc.org/ASCVD‐Risk‐Estimator/ • age >65 • atherosclerosis or risk of developing it (e.g. -
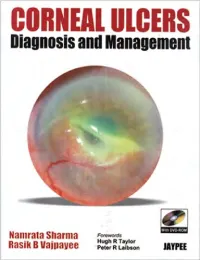
CORNEAL ULCERS Diagnosis and Management
CORNEAL ULCERS Diagnosis and Management System requirement: • Windows XP or above • Power DVD player (Software) • Windows Media Player 10.0 version or above • Quick time player version 6.5 or above Accompanying DVD ROM is playable only in Computer and not in DVD player. Kindly wait for few seconds for DVD to autorun. If it does not autorun then please do the following: • Click on my computer • Click the drive labelled JAYPEE and after opening the drive, kindly double click the file Jaypee CORNEAL ULCERS Diagnosis and Management Namrata Sharma MD DNB MNAMS Associate Professor of Ophthalmology Cornea, Cataract and Refractive Surgery Services Dr. Rajendra Prasad Centre for Ophthalmic Sciences All India Institute of Medical Sciences, New Delhi India Rasik B Vajpayee MS FRCSEd FRANZCO Head, Corneal and Cataract Surgery Centre for Eye Research Australia Royal Victorian Eye and Ear Hospital University of Melbourne Australia Forewords Hugh R Taylor Peter R Laibson ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD New Delhi • Ahmedabad • Bengaluru • Chennai • Hyderabad • Kochi • Kolkata • Lucknow • Mumbai • Nagpur Published by Jitendar P Vij Jaypee Brothers Medical Publishers (P) Ltd B-3 EMCA House, 23/23B Ansari Road, Daryaganj New Delhi 110 002, India Phones: +91-11-23272143, +91-11-23272703, +91-11-23282021, +91-11-23245672 Rel: +91-11-32558559, Fax: +91-11-23276490, +91-11-23245683 e-mail: [email protected] Visit our website: www.jaypeebrothers.com Branches • 2/B, Akruti Society, Jodhpur Gam Road Satellite Ahmedabad 380 015, Phones: +91-79-26926233, -

Retina/Vitreous 2017-2019
Academy MOC Essentials® Practicing Ophthalmologists Curriculum 2017–2019 Retina/Vitreous *** Retina/Vitreous 2 © AAO 2017-2019 Practicing Ophthalmologists Curriculum Disclaimer and Limitation of Liability As a service to its members and American Board of Ophthalmology (ABO) diplomates, the American Academy of Ophthalmology has developed the Practicing Ophthalmologists Curriculum (POC) as a tool for members to prepare for the Maintenance of Certification (MOC) -related examinations. The Academy provides this material for educational purposes only. The POC should not be deemed inclusive of all proper methods of care or exclusive of other methods of care reasonably directed at obtaining the best results. The physician must make the ultimate judgment about the propriety of the care of a particular patient in light of all the circumstances presented by that patient. The Academy specifically disclaims any and all liability for injury or other damages of any kind, from negligence or otherwise, for any and all claims that may arise out of the use of any information contained herein. References to certain drugs, instruments, and other products in the POC are made for illustrative purposes only and are not intended to constitute an endorsement of such. Such material may include information on applications that are not considered community standard, that reflect indications not included in approved FDA labeling, or that are approved for use only in restricted research settings. The FDA has stated that it is the responsibility of the physician to determine the FDA status of each drug or device he or she wishes to use, and to use them with appropriate patient consent in compliance with applicable law. -

Book XIV Art and Psychology
8 88 88 88ycology 8888on.com 8888 Basic Photography in 180 Days Book XIV - Art and Psychology Editor: Ramon F. aeroramon.com Contents 1 Day 1 1 1.1 Visual perception ........................................... 1 1.1.1 Visual system ......................................... 1 1.1.2 Study ............................................. 1 1.1.3 The cognitive and computational approaches ......................... 3 1.1.4 Transduction ......................................... 4 1.1.5 Opponent process ....................................... 4 1.1.6 Artificial visual perception .................................. 4 1.1.7 See also ............................................ 4 1.1.8 Further reading ........................................ 4 1.1.9 References .......................................... 4 1.1.10 External links ......................................... 5 1.2 Depth perception ........................................... 6 1.2.1 Monocular cues ........................................ 6 1.2.2 Binocular cues ........................................ 7 1.2.3 Theories of evolution ..................................... 8 1.2.4 In art ............................................. 8 1.2.5 Disorders affecting depth perception ............................. 9 1.2.6 See also ............................................ 9 1.2.7 References .......................................... 9 1.2.8 Bibliography ......................................... 10 1.2.9 External links ......................................... 10 2 Day 2 11 2.1 Human eye ............................................. -

Non-Diabetic Retinal Vascular Disease”
“Non-Diabetic Retinal Vascular Disease” Brad Sutton, O.D., F.A.A.O. Clinical Professor IU School of Optometry Indianapolis Eye Care Center Retinal Vascular Disease No financial disclosures Hypoperfusion Syndrome Occurs when the eye lacks blood perfusion secondary to carotid artery blockage or ophthalmic artery blockage. Terminology debate: venous stasis retinopathy vs. hypoperfusion syndrome Why is venous stasis retinopathy a poor term for this condition? Hypoperfusion Syndrome Patient may complain of dull, chronic ache in the affected eye Photostress issues / dazzle TIA symptoms may or may not be present (amaurosis fugax) Possible bruit / decreased pulse strength in carotid Hypoperfusion Syndrome Bruit at 30-85% blockage; swishing sound Bell vs. diaphragm Definitive diagnosis requires carotid imaging Hypoperfusion Syndrome Peripheral dot / blot hemorrhages Dilated veins Relatively spares the posterior pole Ocular Ischemic Syndrome With ocular NVD / NVE / NVI ischemic Iritis syndrome same Sluggish pupil findings plus……….. Conjunctival congestion Corneal Edema 80% unilateral / 20% bilateral Ocular Ischemic Syndrome Rare! Only 10% of eyes with 70+% blocked carotids 60% CF or worse VA by one year: 82% if NVI is present Teichopsia: colored afterimages after viewing lights More likely in patients with increased homocysteine and CRP Ocular Ischemic Syndrome When presented with Question about TIA these ocular findings……. Check carotids Arrange for carotid testing (Doppler has limits) ESR C-reactive protein CBC Ocular Ischemic Syndrome Treatment: Systemic management (diet, drugs, surgery) PRP / cryotherapy? Avastin / Lucentis / Eyelea? Five year mortality rate of 40% Sickle Cell Retinopathy Hemoglobinopathy affecting mostly AA (8% in US carry trait, .15% have SS dis.) 60,000 in US: 250,000 born yearly w-wide Malaria and natural selection (sickle trait carriers and sickle cell patients are resistant to malaria) AC, SA, SS, Sthal, SC.