Australia's Response to HIV/AIDS 1982-2005
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
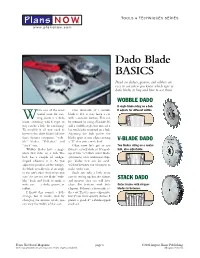
Dado Blade BASICS Dead-On Dadoes, Grooves, and Rabbets Are Easy to Cut When You Know Which Type of Dado Blades to Buy and How to Use Them
TOOLS & TECHNIQUES SERIES Plans NOW® www.plansnow.com Dado Blade BASICS Dead-on dadoes, grooves, and rabbets are easy to cut when you know which type of dado blades to buy and how to use them. WOBBLE DADO A single blade riding on a hub. hile one of the most One downside of a wobble It adjusts for different widths. useful tools for cut- blade is that it may leave a cut Wting joints is a dado with a concave bottom. This can blade, selecting which type to be reduced by using a V-blade. It’s buy can be a little bit confusing. still a wobble-style, but instead it To simplify it, all you need to has two blades mounted on a hub. know is that dado blades fall into Adjusting the hub pushes the three distinct categories: “wob- blades apart at one edge, creating V-BLADE DADO ble” blades, “V-blades,” and a “V” that cuts a wide kerf. “stack” sets. Okay, now let’s get to my Two blades riding on a center Wobble blades have a single favorite:a stack dado set.It’s made hub, also adjustable. 1 blade that rides on a hub. The up of two /8"-thick outer blades hub has a couple of wedge- (trimmers) with additional chip- shaped adjusters in it. As you per blades that can be sand- adjust the position of the wedges, wiched between the trimmers to the blade actually tilts at an angle make wider cuts. to the saw’s arbor.And, when you Stack sets take a little more turn the saw on, the blade “wob- care in setting up, but the dadoes STACK DADO bles” back and forth to make a and grooves they cut will have wide cut — a dado, groove, or clean, flat bottoms with little Outer blades with chipper rabbet. -

Dado & Accessories
20-73 pages 8-28-06 8/30/06 11:21 AM Page 63 Dado Sets & Saw Blade Accessories Dado Sets 63 Whether you’re a skilled professional or a weekend hobbiest, Freud has a dado for you. The SD608, Freud’s Dial-A-Width Dado, has a patented dial system for easy and precise adjustments while offering extremely accurate cuts. The SD300 Series adds a level of safety not found in other manufacturers’ dadoes, while the SD200 Series provides the quality of cuts you expect from Freud, at an attractive price. 20-73 pages 8-28-06 8/30/06 11:21 AM Page 64 Dial-A-Width Stacked Dado Sets NOT A 1 Loosen SD600 WOBBLE Series DADO! 2 Turn The Dial 3 Tighten Features TiCo™ High Dado Cutter Heads Density Carbide Crosscutting Blend For Maximum Performance Chip Free Dadoes In Veneered Plywoods and Laminates The Dial-A-Width Dado set performs like a stacked dado, but Recommended Use & Cut Quality we have replaced the shims with a patented dial system and HARDWOOD: with our exclusive Dial hub, ensures accurate adjustments. SOFTWOOD: Each “click” of the dial adjusts the blade by .004". The Dial- A-Width dado set is easy to use, and very precise. For the CHIP BOARD: serious woodworker, there’s nothing better. PLYWOOD: • Adjusts in .004" increments. 64 LAMINATE: • Maximum 29/32" cut width. NON-FERROUS: • Adjusts easily to right or left operating machines. • Set includes 2 outside blades, 5 chippers, wrench and Application CUT QUALITY: carrying case. (Not recommended for ferrous metals or masonry) • Does not need shims. -

Happy Birthday, Monsieur Jaques! Bon Anniversaire, Monsieur Jaques ! Foreword Paul Hille, Vienna, Feb
2015 150 Happy birthday, Monsieur Jaques! Bon anniversaire, Monsieur Jaques ! Foreword Paul Hille, Vienna, Feb. 2016 2015 was a great year for the international field’s major event of scientific exchange and Eurhythmics community due to Émile Jaques-Dal- acknowledgment of the crucial impulses by croze’s 150th birthday. This volume of Le Rythme the founder of Eurhythmics, including his documents three mayor events. In March: method but also his philosophy and Wel- q The Remscheid Conference: Émile Jaques- tanschauung. Dalcroze 150 – Bonne anniversaire! Interna- All the three events and with them the articles tional Eurhythmics Festival with a special by authors from Germany, Australia, Austria, the artistic outcome by the foundation of the USA, Canada, Korea —for the first time! — and Remscheid Open Arts Rhythmics Reactor/ the UK show that our community is on its way to ROARR. q a more specific scientific discourse. Eckart In July: Altenmüller explains the multisensory-mo- q The Geneva Congrès International Jaques- tor integration, audiation and embodiment Dalcroze, which concerned the interactions of Eurhythmics. between pedagogy, art and science and their q expand historical research on the first and influence on learning music through music later generations of Dalcroze teachers. Ka- today and in future times. rin Greenhead describes personalities and q The 2nd International Conference of Dalcroze situations, which influenced Émile Jaques- Studies (ICDS) in Vienna. Thanks to John Dalcroze’s life and investigates why and how Habron, this conference has become our he created his method. She also gives an About Le Rythme est édité par la FIER (Fédération Internationale des Enseignants de Rythmique) Siège social : 44, Terrassière, CH-1207 Genève www.fier.com | [email protected] The views expressed in Le Rythme do not necessarily represent those of FIER. -

Joint Ex Vivo MRI and Histology Detect Iron-Rich Cortical Gliosis in Tau and TDP-43 Proteinopathies
bioRxiv preprint doi: https://doi.org/10.1101/2021.04.14.439064; this version posted April 14, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Iron-rich cortical pathology in FTLD 1 Joint ex vivo MRI and histology detect iron-rich cortical gliosis in Tau and TDP-43 proteinopathies M. Dylan Tisdall1, Daniel T. Ohm2, Rebecca Lobrovich2, Sandhitsu R. Das2, Gabor Mizsei1, Karthik Prabhakaran2, Ranjit Ittyerah1, Sydney Lim1, Corey T. McMillan2, David A. Wolk2, James Gee1, John Q. Trojanowski3, Edward B. Lee3, John A. Detre1,2, Paul Yushkevich1, Murray Grossman2, David J. Irwin2,3 1Radiology, Perelman School of Medicine, University of Pennsylvania 2Neurology, Perelman School of Medicine, University of Pennsylvania 3Pathology and Laboratory Medicine, Perelman School of Medicine, University of Pennsylvania Corresponding authors: David J. Irwin Frontotemporal Degeneration Center (FTDC) University of Pennsylvania Perelman School of Medicine Hospital of the University of Pennsylvania 3600 Spruce Street, Philadelphia, PA 19104 (215)-662-7682 [email protected] M. Dylan Tisdall Department of Radiology University of Pennsylvania Perelman School of Medicine D406 Richards Building 3700 Hamilton Walk, Philadelphia, PA 19104 bioRxiv preprint doi: https://doi.org/10.1101/2021.04.14.439064; this version posted April 14, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Iron-rich cortical pathology in FTLD 2 (215)- 573-4003 [email protected] bioRxiv preprint doi: https://doi.org/10.1101/2021.04.14.439064; this version posted April 14, 2021. -

Box-Jointed Craft Center
BOX-JOINTED CRAFT CENTER © 2016 Cruz Bay Publishing, Inc. Designer Project Box-Jointed Craft Center This unique storage project holds ample craft supplies in its five stacked trays. When it’s time to work, the trays cantilever out for easy access. More storage is always handy, par- to a comfortable working height when a little work at the band saw to com- ticularly for crafts that involve a lot you’re sitting in a chair. (Refer to page plete the final shaping. of small parts and pieces. That’s why 8 for more on this design option.) CANTILEVER ACTION. But the most inter- I built this handy craft center. In stor- SIMPLE, STURDY CONSTRUCTION. I opted to esting feature of this craft center is age and transport mode, it’s a compact use box joints to hold the five trays how the upper trays pivot out above package that’s easy to carry around together, as well as the handle. This the lower tray. As it turns out, this by its comfortable handle. And when joinery gives the cherry trays a great wasn’t really difficult to do. The secret you’re ready to work, the four ample look while also providing a rock-solid is a series of solid-wood pivot bars upper trays swing out above the large connection between the parts. The joined to the trays with brass binding lower tray to put all the contents within same technique is used to join the posts. I’ll show you the tips and tricks easy reach. An optional stand raises it parts of the handle before performing for installing them on page 5. -

Woodworking Joints.Key
Woodworking making joints Using Joints Basic Butt Joint The butt joint is the most basic woodworking joint. Commonly used when framing walls in conventional, stick-framed homes, this joint relies on mechanical fasteners to hold the two pieces of stock in place. Learn how to build a proper butt joint, and when to use it on your woodworking projects. Basic Butt Joint The simplest of joints is a butt joint - so called because one piece of stock is butted up against another, then fixed in place, most commonly with nails or screws. The addition of glue will add some strength, but the joint relies primarily upon its mechanical fixings. ! These joints can be used in making simple boxes or frames, providing that there will not be too much stress on the joint, or that the materials used will take nails or screws reliably. Butt joints are probably strongest when fixed using glued dowels. Mitered Butt Joint ! A mitered butt joint is basically the same as a basic butt joint, except that the two boards are joined at an angle (instead of square to one another). The advantage is that the mitered butt joint will not show any end grain, and as such is a bit more aesthetically pleasing. Learn how to create a clean mitered butt joint. Mitered Butt Joint The simplest joint that requires any form of cutting is a miter joint - in effect this is an angled butt joint, usually relying on glue alone to construct it. It requires accurate 45° cutting, however, if the perfect 90° corner is to result. -

5.10 Joinery
5.10.1 5.10 Joinery a. the context b. sash windows c. reversible sashes d. sash balances e. casement windows f. transom lights g. room dividers h. H D Annear i modernist joinery j. built-in furniture a. the context The details of joinery concern us here only upon a rather selective basis. Joinery was overwhelmingly traditional and British, inculcated not only by the training of the joiner himself, but by a number of standard texts which were available in the colonies. In a few cases, however, the author of such a text actually emigrated and practised in Australia. In a sense this was true of Samuel Brees, who was the author of the Glossary which will be mentioned below, and who spent time in Victoria and New Zealand. Joshua Jeays, who reached Moreton Bay in 1852, had been responsible for The Geometrical Construction of the Hipped Roof1 and The Orthogonal System of Hand- Railing, with Practical Illustrations of the Construction of Stairs.2 But the most striking example is that of Robert Riddell, who was not British but American. Robert Riddell of Philadephia was an expert carpenter, a specialist in staircases, and the author of The Carpenter and Joiner, Stair Builder and Hand-Railer,3 of 1860. It was published by Thomas C. Jack of Edinburgh in1860" in an edition of five hundred copies. Whether he thought the book sufficient to propel him to international fame, or whether he merely wanted to escape the Civil War, we cannot know, but he and his daughters went to London in about 1861. -

Fine Woodworking 2007 No
192 Build an Fine Woodworking TAUN TON’S Adirondack chair, p. 54 ADIRONDACK CHAIR GLUE TEST FINISHING REPAIRS DRILL-PRESS TEST FIGURED WOOD CABINET BACKS How strong is your glue? 6 types tested with surprising results How to: Fix finishing mistakes Buy a benchtop drill press Choose and use figured woods Design a cabinet back Use chisels precisely Build a door frame July/August 2007 August 2007 No. 192 U.S. $7.99/Canada $8.99 W192FCf.indd 1 5/10/07 11:29:19 AM FW192ADp2.indd 5/11/07 11:11:09 AM pg 2 - (Cyan)(Magenta)(Yellow)(BlacK) FLUSH SANDING VERTICAL SANDING SCRIBING EDGE SANDING FW192ADp3.indd 5/11/07 11:10:14 AM pg 3 - (Cyan)(Magenta)(Yellow)(BlacK) THE BIG IDEA. SMALLER. (Actual Size) Now sanding in tight spaces or unusual orientations is easier than ever. Introducing the most compact belt sander you can buy, the PORTER-CABLE® 371K. It’s the only 21/2˝X14˝ belt sander available. Besides being compact, it has a fl ush side for sanding up to perpendicular surfaces. It also features a low center of gravity for balance, a rubber grip for comfort, and metal components for durability. Find out more about our small wonder at www.porter-cable.com/sanders. READER SERVICE NO. 135 contentsJULY/AUGUST2007 ISSUE192 features 36 How Strong Is COVER STORY Your Glue? We take six types to the breaking point, shattering some common wisdom in the process B Y MARK SCHOFIELD 41 10 Best Fixes for Finishing Mistakes Cures for common problems, and how to prevent them in the first place B Y TERI MASASCHI 48 A Back for Every Cabinet The right choices balance strength, appearance, and efficiency B Y S T E V E L A T T A CENTER-GUIDED 72 DRAWERS Cover photo: Mark Schofield w192CT.indd 4 5/10/07 11:52:09 AM UNDERSTANDING up front 92 WOOD FIGURE 6 On the Web 8 Contributors 10 Letters 14 Methods of Work N Shopmade stand holds carving gouges N Carry sheet goods with ease ADIRONDACK CHAIR 54 20 Tools & Materials N Bosch shop vacuum N Blue Spruce dovetail chisels N Pinnacle honing guide NEW 26 What’s the Difference? Natural vs. -

Measuring & Marking Tools
Measuring & Marking Tools Dividers & Callipers • Dividers are instruments that can be used to transfer measurements directly from a rule, to measure distances on a map, or to scribe an arc or a circle. • Wing dividers feature a curved steel bar to separate the legs, while the distance is set with a lock nut. • Callipers (inside or outside) work in the same way, but are designed for measurement, rather than marking. 3170 3170-SS 3175-SS STRAIGHT EDGE STAINLESS STEEL STRAIGHT EDGE S/STEEL STRAIGHT EDGE IN WOODEN CASE • Manufactured from carbon steel • Stainless steel • Stainless steel • Made with one squared edge and one bevelled edge • Finely polished • Finely polished • Comes in graduated (mm) or plain without graduation • Made with one squared edge and one bevelled edge • Square on both edges • Sizes up to 2000 mm are chromated, 3000 mm lengths • Comes in graduated (mm) or plain with no graduation • Permanently etched graduations are finely polished • Removable positioning/carrying knob/s • Includes calibration certificate • Comes in wooden case • In accordance to DIN 866/1 standards (tolerance - 0.04 mm/m) Hang Display (t((tolerancetoololeolerllelereerraancanceanncennccece --0 00.04.04.0.0404 mm/mmmmm/mmm/m)m/mmm//m/m) Removable positioning/carrying knob/s NOTE: Supplied with cat.-no. length (mm) section (mm) knobs Calibration certificate. (Tolerance - 0.04 mm/m) Graduated (mm) 3170-M-SS-500 500 40 x 3 1 cat.-no. length (mm) section (mm) 3170-M-SS-1000 1000 50 x 4 2 3175-SS-A-500 500 30 x 6 3170-M-SS-1500 1500 50 x 4 2 3175-SS-A-1000 1000 40 x 8 3170-M-SS-2000 2000 50 x 4 2 Plain, no graduation 1511 3170-P-SS-500 500 40 x 3 1 3170-P-SS-1000 1000 50 x 4 2 WING DIVIDER 3170-P-SS-1500 1500 50 x 4 2 • High quality forged steel • Heavy rivet and box joint mechanism Hang 3170-P-SS-2000 2000 50 x 4 2 • All polished Display cat.-no. -

Cromwelliana
Cromwelliana The Journal of The Cromwell Association 2017 The Cromwell Association President: Professor PETER GAUNT, PhD, FRHistS Vice Presidents: PAT BARNES Rt Hon FRANK DOBSON, PC Rt Hon STEPHEN DORRELL, PC Dr PATRICK LITTLE, PhD, FRHistS Professor JOHN MORRILL, DPhil, FBA, FRHistS Rt Hon the LORD NASEBY, PC Dr STEPHEN K. ROBERTS, PhD, FSA, FRHistS Professor BLAIR WORDEN, FBA Chairman: JOHN GOLDSMITH Honorary Secretary: JOHN NEWLAND Honorary Treasurer: GEOFFREY BUSH Membership Officer PAUL ROBBINS The Cromwell Association was formed in 1937 and is a registered charity (reg no. 1132954). The purpose of the Association is to advance the education of the public in both the life and legacy of Oliver Cromwell (1599-1658), politician, soldier and statesman, and the wider history of the seventeenth century. The Association seeks to progress its aims in the following ways: campaigns for the preservation and conservation of buildings and sites relevant to Cromwell commissions, on behalf of the Association, or in collaboration with others, plaques, panels and monuments at sites associated with Cromwell supports the Cromwell Museum and the Cromwell Collection in Huntingdon provides, within the competence of the Association, advice to the media on all matters relating to the period encourages interest in the period in all phases of formal education by the publication of reading lists, information and teachers’ guidance publishes news and information about the period, including an annual journal and regular newsletters organises an annual service, day schools, conferences, lectures, exhibitions and other educational events provides a web-based resource for researchers in the period including school students, genealogists and interested parties offers, from time to time grants, awards and prizes to individuals and organisations working towards the objectives stated above. -

Översättning Av Slöjd Och Snickeriord, Svenska-Engelska
Översättning av Slöjd och Snickeriord, Svenska-Engelska SVENSKA ENGELSKA (US, UK) 1 Al (Alnus) Alder 2 Alm (Ulmus glabra) Elm 3 Aln (593,8 mm) Ell (23,4”) 4 Andningsskydd Face mask 5 Arbetsbänk Workbench 6 Arbetshandskar Working gloves 7 Ask (Fraxinus excelsior) Ash 8 Asp (Populus tremula ) European Aspen 9 Avbitare Cutting nipper/plier 10 Avenbok (Carpinus betulus) Hornbeam, -beech 11 Bandkniv Drawknife 12 Bandslipmaskin Beltsander 13 Bandsåg Band-saw 14 Bark Bark 15 Barksida Bark side 16 Barrträd Coniferous tree 17 Basa Steam bending 18 Baslåda Steambox 19 Benlim Bone glue 20 Bets Analine dye 21 Bildhuggarjärn Gauge 22 Bildhuggarklubba Mallet 23 Bildhuggarskölp Carving chisel 24 Bits Bits 25 Björk (Betula-) Birch Av Morgan Nilsson 2021 1 av 40 Översättning av Slöjd och Snickeriord, Svenska-Engelska 26 Björknäver Birch bark 27 Björksav Birch syrup 28 Björkvril Birch burl 29 Blad (på kniv) Blade (on knife) 30 Blyertspenna Pencil 31 Bock (stöd) Stand 32 Bock (stöd) Trestle 33 Bok (Fagus silvatica) Beech 34 Bordcirkelsåg Table saw 35 Borr Drill 36 Borra Boring/Bore 37 Borrmaskin Drilling machine 38 Borrstativ Drill stand 39 Borrsväng Brace 40 Borste/pensel Brush 41 Bricka (till skruv/bult) Washer 42 Brotsch (konisk borr) Reamer 43 Bryna Sharpen 44 Brynolja Honing oil 45 Brynsten Sharpening stone 46 Brynsten (knivformigt) Slipstones 47 Brytbladskniv Snap-off-blade-knife 48 Bräda (mindre än 45x70 mm) Board 49 Brädgård Lumber yard (US) 50 Brädgård Timber yard (UK) 51 Bubinga (Guibourtia demeusei) Bubinga Av Morgan Nilsson 2021 2 av 40 Översättning -

PWM Style Book Jan 2014.Pdf
Style Book Revised: January 2014 PW Style Book Revised: Jan 2014 Numbers, Measurements • #400-grit (adj) • 30 years adze (n): a primitive tool for surfacing lumber and Callouts • #400 grit (n) • #0000 steel wool • #1,000 grit stone • 1-pound cut, 2-pound cut etc. aftermarket (n): the market for parts, accessories and repairs • 40-tooth (adj) (for shellac) • thickness x width x length of a product; also, a secondary • On anything dimensional, • $2,800 (not $2800) • 1 horsepower; 1 hp (1-hp market for a product after the use numerals and birds’ feet, router); spell out ‘horsepower’ primary market; an aftermarket • 2" scale even if it’s an approximation on first reference, then can use fence for a table saw, for example • 32" x 48" ‘hp’ abbreviation (this departs from AP style) AIA (abbreviation): American • 4' x 7' 1/4"-20 (machine screw thread; • 4/4 lumber (reads as “four- Institute of Architects • 2x4; 2x4s (Name for quarter lumber”; refers to rough- 1/4" is diameter, 20 is threads per air-conditioner (n); construction-grade lumber, cut lumber measured by quarters inch) air-conditioning (A/C) (n); usually pine, generally used for or an inch; do not set as stacked • 70°F (no space; don’t spell out air-conditioned (adj) wall studs; is not really 2" by 4", fractions) on first ref.) air-dry (v); air-dried (adj): a but an estimate of the size used • mid-1800s • 3D (departure from AP) commonly; do not include inch method of seasoning lumber •30mm, 25 cm marks) which permits the sawn wood, • model 41293 which is usually protected from • 90°