Seborrheic Dermatitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Where Does Psoriasis Fit
Dr Shan Edwards Dermatologist Dermatology Clinic, Christchurch 11:00 - 11:55 WS #86: Differential Diagnosis Based on Classic Location - Where Does Psoriasis Fit In? 12:05 - 13:00 WS #97: Differential Diagnosis Based on Classic Location - Where Does Psoriasis Fit In? (Repeated) Differential diagnosis based on classic location Where does psoriasis fit in? Dr Shan Edwards , dermatologist Christchurch 2016 2 Conflict statement . This talk sponsored by LEO Pharma Pty Ltd . I have no other association financial or otherwise with LEO Pharma Pty Ltd 3 Acknowedgement I wish to thank and acknowledge and thank A/Prof Amanda Oakley for providing a lot of the material and allowing me to use it in this talk I would also like to acknowledge Dermnet NZ as a source for most of my clinical slides 4 How do you diagnose red scaly skin ? Take a history (90% diagnosis made on history) . When did scaly rash first appear? . What do you think caused it? . What treatments used and their effects? . Personal history of skin problems ? . Family history of similar disorders? . Occupation, hobbies, other life events? . Symptoms: itch? Other eg fever, weightloss unwell Other medical problems?(co-morbidities) . Current medicines : how long, any new ? 7 When did scaly rash first appear? . Infancy: seborrhoeic dermatitis/eczema . Toddler: atopic dermatitis/eczema . Pre-schooler/primary school: tinea capitis/corporis . Primary school: head lice . Teenage/adult: seborrhoeic dermatitis/eczema, psoriasis . Adult/elderly: drug rash, lymphoma, other less common skin conditions(PRP,Lupus) . All age groups:scabies 8 Dear Shan Re: Miss EM age 7yrs I am completely puzzled by EM’s rash and particularly so since there now appear to be other areas of her body being affected by it. -
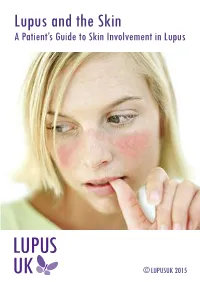
Lupus and the Skin a Patient’S Guide to Skin Involvement in Lupus
Lupus and the Skin A Patient’s Guide to Skin Involvement in Lupus © LUPUSUK 2015 LUPUS and the Skin LUPUS UK acknowledges with gratitude the assistance of Sue Brown, Consultant Nurse in Rheumatology (Connective Tissue Diseases), Royal National Hospital for Rheumatic Diseases NHS Foundation Trust, Bath and Dr Chris Lovell, Consultant Dermatologist, Royal United Hospital and Royal National Hospital for Rheumatic Diseases NHS Foundation Trust, Bath in the provision of clinical information towards the production of this booklet. ACKNOWLEDGEMENT The authors would like to thank Professor Peter Maddison, Consultant Rheumatologist and Dr Andrew Macfarlane, Consultant Dermatologist at Ysbyty Gwynedd, Bangor, Wales, who wrote the first edition of this booklet and have kindly agreed to its revision. LUPUS UK is the national charity caring for those with systemic lupus erythematosus (SLE) and discoid lupus erythematosus (DLE), supporting people as they develop the symptoms prior to diagnosis and those already diagnosed. You can help by taking up membership For more information contact: LUPUS UK, St James House, Eastern Road, Romford, Essex RM1 3NH Tel: 01708 731251 www.lupusuk.org.uk Reg. charity nos 1051610, SC039682 © LUPUS UK 2012 All rights reserved. No part of this book may be reproduced in any form without written permission from LUPUS UK. Index Section Page No 1 Introduction 1 2 Types of rashes 2 3 Mechanism of photosensitivity 5 4 Treatment of the skin in lupus 7 5 Sun protection 10 6 Quality of life 11 7 Fatigue 12 8 Self help 12 9 Research 14 10 Further reading 14 1. Introduction Many people with lupus may have skin problems, and a rash may be the first sign of the condition. -

Scabies in Healthcare Facilities
Scabies in Healthcare Facilities Tammra L. Morrison, RN BSN Healthcare Associated Infections Coordinator Communicable Disease Branch, Epidemiology Section December 9, 2016 Symptoms • In a person who has never had scabies: • May take 4-6 weeks for symptom onset • In a person who has had scabies in the past: • Symptoms may start in 1-4 days • May be spread PRIOR to symptom onset What to Look for • Intense itching • Especially at night • Pimple-like itchy rash • May affect entire body OR Dermatologie.md common sites: • Wrist, elbow, armpit, webbing between the fingers, nipple, penis, waist, belt-line, and buttocks • Burrows (tunnels) may be seen on the skin • Tiny raised and crooked grayish-white or skin- colored lines Transmission • Direct, prolonged, skin-to-skin contact with an infested person • Sexual partners • Household members • Quick handshake/hug will usually not spread scabies How Long Do Mites Live? • 1-2 months on a person • 48-72 hours off a person • Scabies mites will die at 122 degrees for 10 minutes Webmd.com 5 Diagnosis • Customary appearance and distribution of the rash and presence of burrows. • Confirm diagnosis: • Obtain a skin scraping to examine under a microscope for mites, eggs, or mite fecal matter • Person can still be infested even if mites, eggs, or fecal matter cannot be found • Typically fewer than 10-15 mites present on the entire body • **Crusted scabies may be thousands of mites and should be considered highly contagious** How Do You Treat Scabies? 7 Treatment • Available only by prescription • No "over-the-counter“ -

Scalp Eczema Factsheet the Scalp Is an Area of the Body That Can Be Affected by Several Types of Eczema
12 Scalp eczema factsheet The scalp is an area of the body that can be affected by several types of eczema. The scalp may be dry, itchy and scaly in a chronic phase and inflamed (red), weepy and painful in an acute (eczema flare) phase. Aside from eczema, there are a number of reasons why the scalp can become dry and itchy (e.g. psoriasis, fungal infection, ringworm, head lice etc.), so it is wise to get a firm diagnosis if there is uncertainty. Types of eczema • Hair clips and headgear – especially those containing that affect the scalp rubber or nickel. Seborrhoeic eczema (dermatitis) is one of the most See the NES booklet on Contact Dermatitis for more common types of eczema seen on the scalp and hairline. details. It can affect babies (cradle cap), children and adults. The Irritant contact dermatitis is a type of eczema that skin appears red and scaly and there is often dandruff as occurs when the skin’s surface is irritated by a substance well, which can vary in severity. There may also be a rash that causes the skin to become dry, red and itchy. on other parts of the face, such as around the eyebrows, For example, shampoos, mousses, hair gels, hair spray, eyelids and sides of the nose. Seborrhoeic eczema can perm solution and fragrance can all cause irritant contact become infected. See the NES factsheets on Adult dermatitis. See the NES booklet on Contact Dermatitis for Seborrhoeic Dermatitis and Infantile Seborrhoeic more details. Dermatitis and Cradle Cap for more details. -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

Classification of Medicinal Drugs and Driving: Co-Ordination and Synthesis Report
Project No. TREN-05-FP6TR-S07.61320-518404-DRUID DRUID Driving under the Influence of Drugs, Alcohol and Medicines Integrated Project 1.6. Sustainable Development, Global Change and Ecosystem 1.6.2: Sustainable Surface Transport 6th Framework Programme Deliverable 4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Due date of deliverable: 21.07.2011 Actual submission date: 21.07.2011 Revision date: 21.07.2011 Start date of project: 15.10.2006 Duration: 48 months Organisation name of lead contractor for this deliverable: UVA Revision 0.0 Project co-funded by the European Commission within the Sixth Framework Programme (2002-2006) Dissemination Level PU Public PP Restricted to other programme participants (including the Commission x Services) RE Restricted to a group specified by the consortium (including the Commission Services) CO Confidential, only for members of the consortium (including the Commission Services) DRUID 6th Framework Programme Deliverable D.4.4.1 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Page 1 of 243 Classification of medicinal drugs and driving: Co-ordination and synthesis report. Authors Trinidad Gómez-Talegón, Inmaculada Fierro, M. Carmen Del Río, F. Javier Álvarez (UVa, University of Valladolid, Spain) Partners - Silvia Ravera, Susana Monteiro, Han de Gier (RUGPha, University of Groningen, the Netherlands) - Gertrude Van der Linden, Sara-Ann Legrand, Kristof Pil, Alain Verstraete (UGent, Ghent University, Belgium) - Michel Mallaret, Charles Mercier-Guyon, Isabelle Mercier-Guyon (UGren, University of Grenoble, Centre Regional de Pharmacovigilance, France) - Katerina Touliou (CERT-HIT, Centre for Research and Technology Hellas, Greece) - Michael Hei βing (BASt, Bundesanstalt für Straßenwesen, Germany). -

The Management of Common Skin Conditions in General Practice
Management of Common Skin Conditions In General Practice including the “red rash made easy” © Arroll, Fishman & Oakley, Department of General Practice and Primary Health Care University of Auckland, Tamaki Campus Reviewed by Hon A/Prof Amanda Oakley - 2019 http://www.dermnetnz.org Management of Common Skin Conditions In General Practice Contents Page Derm Map 3 Classic location: infants & children 4 Classic location: adults 5 Dermatology terminology 6 Common red rashes 7 Other common skin conditions 12 Common viral infections 14 Common bacterial infections 16 Common fungal infections 17 Arthropods 19 Eczema/dermatitis 20 Benign skin lesions 23 Skin cancers 26 Emergency dermatology 28 Clinical diagnosis of melanoma 31 Principles of diagnosis and treatment 32 Principles of treatment of eczema 33 Treatment sequence for psoriasis 34 Topical corticosteroids 35 Combination topical steroid + antimicrobial 36 Safety with topical corticosteroids 36 Emollients 37 Antipruritics 38 For further information, refer to: http://www.dermnetnz.org And http://www.derm-master.com 2 © Arroll, Fishman & Oakley, Department of General Practice and Primary Health Care, University of Auckland, Tamaki Campus. Management of Common Skin Conditions In General Practice DERM MAP Start Is the patient sick ? Yes Rash could be an infection or a drug eruption? No Insect Bites – Crop of grouped papules with a central blister or scab. Is the patient in pain or the rash Yes Infection: cellulitis / erysipelas, impetigo, boil is swelling, oozing or crusting? / folliculitis, herpes simplex / zoster. Urticaria – Smooth skin surface with weals that evolve in minutes to hours. No Is the rash in a classic location? Yes See our classic location chart . -

Eczema of Infancy and Childhood
International Journal of Medicine Research International Journal of Medicine Research ISSN: 2455-7404; Impact Factor: RJIF 5.42 Received: 23-02-2020; Accepted: 21-03-2020; Published: 11-04-2020 www.medicinesjournal.com Volume 5; Issue 2; 2020; Page No. 21-23 Eczema of infancy and childhood Dr. Magida Kathm1, Dr. Baraa W Taha2, Dr. Nassema Lazim3 1, 2, 3 Centeral Teaching Hospital of Peadiatrics, Baghdad, Iraq Abstract Background: Eczema of infancy and childhood is one of the commom dermatological diseases in Iraqi patients for this reason this study was arranged. Objective: To assessment of an epidemiological study aimed at characterization of different clinical aspects of eczema in children and in infants in Iraqi population. Patient and Methods: A total number of tow hundred and fifty patients was seen and studied in the department of dermatology / Medical City Baghdad, FROM December 2013 to April 2014. They were 131 males and 119 female. Their ages ranged from 2 weeks to 12 years, mean age 4.43 years with mean age of onset was 3.65 years. A detailed history was taken from each patient with emphasis on the following relivant points: age, age of onset, sex, family history of atopy, personal history of atopy, history of food allergy, any associated diseases and any seasonal variations. All patients were fully examined regarding the type, morphology and distribution of the lesions in each type of eczema including: Atopic dermatitis, discoid eczema, pityriasis Alba and seborrhoeic dermatitis. The type of feeding whether breast, bottle or mixed feeding was assessed in all types of eczema. -

Health Economics and Dermatology
Extracts from the Lectures of the 32nd Nordic Congress of Dermato-Venereology, Tampere, Finland Hyperpigmentation is a common symptom but will not pro- vide much valuable information to help diagnosing the skin condition. Almost all skin diseases in dark skin can give hyper- pigmentation at some point, especially if they have a chronic or protracted course. A non-specific hyperchromia can darken the elementary lesions of the underlying dermatosis, which could mislead the physician when examining the patient. Hyperpigmentation is the main cause of consultation of dark- skinned patients but the list of causes of hyperpigmentation is countless, thus topography and additional signs should help the physician. Three conditions are of particular exception, namely acne, lichen planus and prurigo lesions in HIV patients. Hypopigmentation on the other hand is an important sign for diagnosis and hypopigmentation also severely impairs the quality of life of the patients. Causes of permanent achromia Fig. 2. Prurigo nodularis in include mainly vitiligo, post-traumatic achromia, idiopathic an HIV patients. Typical Fig. 3. Heterogenous depigmentation hypomelanosis, chronic lupus of the discoid type, and burns. annular pigmented itchy induced by skin bleaching agents. lesions with central depig- Causes of mottled hypopigmentation include vitiligo, systemic mentation. scleroderma and lichenification. Lastly, frequent causes of hypopigmentation include eczema, seborrhoeic dermatitis, pityriasis versicolor, vitiligo minor, injection or local treat- systemic complications. As users tend to hide the use of such ment of corticosteroids, achromic hamartoma, lichen striatus agents to the physician it is important to treat any underlying or verruca plana. Rare causes of hypopigmentation include skin dermatoses, disrupt bleaching agents, avoid any judge- mycosis fungoides, sarcoidosis and leprosy. -

CCA Senior Care Options Formulary
Commonwealth Care Alliance Senior Care Option HMO SNP 2021 List of Covered Drugs Formulary 30 Winter Street • Boston, MA 02108 PLEASE READ: THIS DOCUMENT CONTAINS INFORMATION ABOUT THE DRUGS WE COVER IN THIS PLAN This formulary was updated on 08/01/2021. For more recent information or other questions, please contact Senior Care Options Program (HMO SNP) Member Services, at 1-866-610-2273 or, for TTY users, 711, 8 a.m. – 8 p.m., 7 days a week, or visit www.commonwealthcaresco.org. HPMS Approved Formulary File Submission ID 00021589, Version Number 13 Senior Care Options Program (HMO SNP) 2021 Formulary (List of Covered Drugs) PLEASE READ: THIS DO CUMENT CONTAINS INFORMATION ABOUT THE DRUGS WE COVER IN THIS PLAN HPMS Approved Formulary File Submission ID 00021589, Version Number 13 Note to existing members: This formulary has changed since last year. Please review this document to make sure that it still contains the drugs you take. When this drug list (formulary) refers to “we,” “us”, or “our,” it means Commonwealth Care Alliance. When it refers to “plan” or “our plan,” it means 2021 Senior Care Options Program. This document includes list of the drugs (formulary) for our plan which is current as of 08/01/2021. This formulary document applies to all SCO members. For an updated formulary, please contact us. Our contact information, along with the date we last updated the formulary, appears on the front and back cover pages. You must generally use network pharmacies to use your prescription drug benefit. Benefits, formulary, pharmacy n etwork, and/or copayments/coinsurance may change on January 1, 2022, and from time to time during the year. -

Salicylic Acid
Treatment Guide to Common Skin Conditions Prepared by Loren Regier, BSP, BA, Sharon Downey -www.RxFiles.ca Revised: Jan 2004 Dermatitis, Atopic Dry Skin Psoriasis Step 1 - General Treatment Measures Step 1 - General Treatment Measures Step 1 • Avoid contact with irritants or trigger factors • Use cool air humidifiers • Non-pharmacologic measures (general health issues) • Avoid wool or nylon clothing. • Lower house temperature (minimize perspiration) • Moisturizers (will not clear skin, but will ↓ itching) • Wash clothing in soap vs detergent; double rinse/vinegar • Limit use of soap to axillae, feet, and groin • Avoid frequent or prolonged bathing; twice weekly • Topical Steroids Step 2 recommended but daily bathing permitted with • Coal Tar • Colloidal oatmeal bath products adequate skin hydration therapy (apply moisturizer • Anthralin • Lanolin-free water miscible bath oil immediately afterwards) • Vitamin D3 • Intensive skin hydration therapy • Limit use of soap to axillae, feet, and groin • Topical Retinoid Therapy • “Soapless” cleansers for sensitive skin • Apply lubricating emollients such as petrolatum to • Sunshine Step 3 damp skin (e.g. after bathing) • Oral antihistamines (1st generation)for sedation & relief of • Salicylic acid itching give at bedtime +/- a daytime regimen as required Step 2 • Bath additives (tar solns, oils, oatmeal, Epsom salts) • Topical hydrocortisone (0.5%) for inflammation • Colloidal oatmeal bath products Step 2 apply od-tid; ointments more effective than creams • Water miscible bath oil • Phototherapy (UVB) may use cream during day & ointment at night • Humectants: urea, lactic acid, phospholipid • Photochemotherapy (Psoralen + UVA) Step 4 Step 3 • Combination Therapies (from Step 1 & 2 treatments) • Prescription topical corticosteroids: use lowest potency • Oral antihistamines for sedation & relief of itching steroid that is effective and wean to twice weekly. -

Dermatological Effects of Different Keratolytic Agents on Acne Vulgaris
Clin l of ica a l T n r r i u a l o s J Alodeani, J Clin Trials 2016, 6:2 Journal of Clinical Trials DOI: 10.4172/2167-0870.1000262 ISSN: 2167-0870 Research Article Open Access Dermatological Effects of Different Keratolytic Agents on Acne Vulgaris Essa Ajmi Alodeani* College of Medicine at AD-Dwadmi, Shaqra University, Saudi Arabia *Corresponding author: Essa Ajmi Alodeani, College of Medicine at AD-Dwadmi, Shaqra University, Saudi Arabia, Tel: +966 55 075 9042; E-mail: [email protected] Received date: March 24, 2016; Accepted date: April 18, 2016; Published date: April 25, 2016 Copyright: © 2016 Alodeani EA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Acne vulgaris is a chronic inflammatory skin disease; it's one of the most common skin disorders and affects mainly adolescents and young adults. Keratolytic agents are widely used in treatment of acne from several years. In this study we aimed to evaluate and compare the cutaneous response of different keratolytic agents in management of acne vulgaris. Ninety patients were selected among those attending the outpatient dermatology clinic in AD- Dwadmi hospital during the period from October 2015 to February 2016. The selected patients had different forms of acne vulgaris, papulo-pustular, comedonal and post acne scar. Three types of keratolytic agents were used, glycolic acid 50%, salicylic acid 20% and jessner solution. In papulopustular lesions, the three agents were effective with non-significant difference between them; however, there was more excellent results with jessner solution (70 % of patients) then glycolic acid (50%) and lastly salicylic acid (40%).