Young Adults Young Adults (20 - 35 Years)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Reporting of Diseases and Conditions Regulation, Amendment, M.R. 289/2014
THE PUBLIC HEALTH ACT LOI SUR LA SANTÉ PUBLIQUE (C.C.S.M. c. P210) (c. P210 de la C.P.L.M.) Reporting of Diseases and Conditions Règlement modifiant le Règlement sur la Regulation, amendment déclaration de maladies et d'affections Regulation 289/2014 Règlement 289/2014 Registered December 23, 2014 Date d'enregistrement : le 23 décembre 2014 Manitoba Regulation 37/2009 amended Modification du R.M. 37/2009 1 The Reporting of Diseases and 1 Le présent règlement modifie le Conditions Regulation , Manitoba Règlement sur la déclaration de maladies et Regulation 37/2009, is amended by this d'affections , R.M. 37/2009. regulation. 2 Schedules A and B are replaced with 2 Les annexes A et B sont remplacées Schedules A and B to this regulation. par les annexes A et B du présent règlement. Coming into force Entrée en vigueur 3 This regulation comes into force on 3 Le présent règlement entre en vigueur January 1, 2015, or on the day it is registered le 1 er janvier 2015 ou à la date de son under The Statutes and Regulations Act , enregistrement en vertu de Loi sur les textes whichever is later. législatifs et réglementaires , si cette date est postérieure. December 19, 2014 Minister of Health/La ministre de la Santé, 19 décembre 2014 Sharon Blady 1 SCHEDULE A (Section 1) 1 The following diseases are diseases requiring contact notification in accordance with the disease-specific protocol. Common name Scientific or technical name of disease or its infectious agent Chancroid Haemophilus ducreyi Chlamydia Chlamydia trachomatis (including Lymphogranuloma venereum (LGV) serovars) Gonorrhea Neisseria gonorrhoeae HIV Human immunodeficiency virus Syphilis Treponema pallidum subspecies pallidum Tuberculosis Mycobacterium tuberculosis Mycobacterium africanum Mycobacterium canetti Mycobacterium caprae Mycobacterium microti Mycobacterium pinnipedii Mycobacterium bovis (excluding M. -

Where Does Psoriasis Fit
Dr Shan Edwards Dermatologist Dermatology Clinic, Christchurch 11:00 - 11:55 WS #86: Differential Diagnosis Based on Classic Location - Where Does Psoriasis Fit In? 12:05 - 13:00 WS #97: Differential Diagnosis Based on Classic Location - Where Does Psoriasis Fit In? (Repeated) Differential diagnosis based on classic location Where does psoriasis fit in? Dr Shan Edwards , dermatologist Christchurch 2016 2 Conflict statement . This talk sponsored by LEO Pharma Pty Ltd . I have no other association financial or otherwise with LEO Pharma Pty Ltd 3 Acknowedgement I wish to thank and acknowledge and thank A/Prof Amanda Oakley for providing a lot of the material and allowing me to use it in this talk I would also like to acknowledge Dermnet NZ as a source for most of my clinical slides 4 How do you diagnose red scaly skin ? Take a history (90% diagnosis made on history) . When did scaly rash first appear? . What do you think caused it? . What treatments used and their effects? . Personal history of skin problems ? . Family history of similar disorders? . Occupation, hobbies, other life events? . Symptoms: itch? Other eg fever, weightloss unwell Other medical problems?(co-morbidities) . Current medicines : how long, any new ? 7 When did scaly rash first appear? . Infancy: seborrhoeic dermatitis/eczema . Toddler: atopic dermatitis/eczema . Pre-schooler/primary school: tinea capitis/corporis . Primary school: head lice . Teenage/adult: seborrhoeic dermatitis/eczema, psoriasis . Adult/elderly: drug rash, lymphoma, other less common skin conditions(PRP,Lupus) . All age groups:scabies 8 Dear Shan Re: Miss EM age 7yrs I am completely puzzled by EM’s rash and particularly so since there now appear to be other areas of her body being affected by it. -

Smelly Foot Rash
CLINICAL Smelly foot rash Paulo Morais Ligia Peralta Keywords: skin diseases, infectious Case study A previously healthy Caucasian girl, 6 years of age, presented with pruritic rash on both heels of 6 months duration. The lesions appeared as multiple depressions 1–2 mm in diameter that progressively increased in size. There was no history of trauma or insect bite. She reported local pain when walking, worse with moisture and wearing sneakers. On examination, multiple small crater- like depressions were present, some Figure 1. Heel of patient coalescing into a larger lesion on both heels (Figure 1). There was an unpleasant ‘cheesy’ protective/occluded footwear for prolonged odour and a moist appearance. Wood lamp periods.1–4 examination and potassium hydroxide testing for fungal hyphae were negative. Answer 2 Question 1 Pitted keratolysis is frequently seen during What is the diagnosis? summer and rainy seasons, particularly in tropical regions, although it occurs Question 2 worldwide.1,3,4 It is caused by Kytococcus What causes this condition? sedentarius, Dermatophilus congolensis, or species of Corynebacterium, Actinomyces or Question 3 Streptomyces.1–4 Under favourable conditions How would you confirm the diagnosis? (ie. hyperhidrosis, prolonged occlusion and increased skin surface pH), these bacteria Question 4 proliferate and produce proteinases that destroy What are the differential diagnoses? the stratum corneum, creating pits. Sulphur containing compounds produced by the bacteria Question 5 cause the characteristic malodor. What is your management strategy? Answer 3 Answer 1 Pitted keratolysis is usually a clinical Based on the typical clinical picture and the negative diagnosis with typical hyperhidrosis, malodor ancillary tests, the diagnosis of pitted keratolysis (PK) (bromhidrosis) and occasionally, tenderness, is likely. -

What Certified Athletic Trainers and Therapists Need to Know Thomas M
PHYSICIAN PERSPECTIVE Tracy Ray, MD, Column Editor Sports Dermatology: What Certified Athletic Trainers and Therapists Need to Know Thomas M. Dougherty, MD • American Sports Medicine Institute, Birmingham AL OST SPECIAL SKIN problems of athletes are ting shoes for all athletes and gloves for weight lifters M easily observable and can be recognized and racket-sport players can help. and treated early. Proper care can prevent Occlusive folliculitis, also known as acne mechanica disruption of the training or competition schedule. or “football acne,” is a flare of sometimes preexisting Various athletic settings expose the skin to a multi- acne caused by heat, occlusion, and pressure distrib- tude of infectious organisms while increasing its vul- uted in areas under bulky playing equipment (e.g., nerability to infection. A working knowledge of skin shoulders, forehead, chin in football players; legs, arms, disorders in athletes is essential for athletic trainers, trunk in wrestlers). Inflammatory papules and pustules who are often the first to evaluate athletes for medi- are present. A clean absorbent T-shirt should be worn cal problems. under equipment, and the affected areas should be cleansed after a workout. Direct Cutaneous Injury Follicular keloidalis is seen mostly in African-Ameri- can athletes and is a progression of occlusive folliculi- Calluses are the skin’s compensatory, protective re- tis with nontender, firm, fibrous papules around the sponse to friction, most commonly seen on the feet edges of the football helmet, especially at the posterior but also on the hands of golfers and in oar and racket neck and occipital scalp. Surgical treatment, if indicated, sports. -
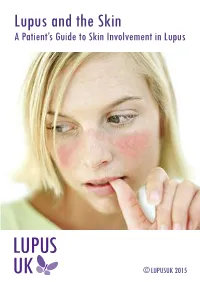
Lupus and the Skin a Patient’S Guide to Skin Involvement in Lupus
Lupus and the Skin A Patient’s Guide to Skin Involvement in Lupus © LUPUSUK 2015 LUPUS and the Skin LUPUS UK acknowledges with gratitude the assistance of Sue Brown, Consultant Nurse in Rheumatology (Connective Tissue Diseases), Royal National Hospital for Rheumatic Diseases NHS Foundation Trust, Bath and Dr Chris Lovell, Consultant Dermatologist, Royal United Hospital and Royal National Hospital for Rheumatic Diseases NHS Foundation Trust, Bath in the provision of clinical information towards the production of this booklet. ACKNOWLEDGEMENT The authors would like to thank Professor Peter Maddison, Consultant Rheumatologist and Dr Andrew Macfarlane, Consultant Dermatologist at Ysbyty Gwynedd, Bangor, Wales, who wrote the first edition of this booklet and have kindly agreed to its revision. LUPUS UK is the national charity caring for those with systemic lupus erythematosus (SLE) and discoid lupus erythematosus (DLE), supporting people as they develop the symptoms prior to diagnosis and those already diagnosed. You can help by taking up membership For more information contact: LUPUS UK, St James House, Eastern Road, Romford, Essex RM1 3NH Tel: 01708 731251 www.lupusuk.org.uk Reg. charity nos 1051610, SC039682 © LUPUS UK 2012 All rights reserved. No part of this book may be reproduced in any form without written permission from LUPUS UK. Index Section Page No 1 Introduction 1 2 Types of rashes 2 3 Mechanism of photosensitivity 5 4 Treatment of the skin in lupus 7 5 Sun protection 10 6 Quality of life 11 7 Fatigue 12 8 Self help 12 9 Research 14 10 Further reading 14 1. Introduction Many people with lupus may have skin problems, and a rash may be the first sign of the condition. -

Seborrheic Dermatitis: an Overview ROBERT A
Seborrheic Dermatitis: An Overview ROBERT A. SCHWARTZ, M.D., M.P.H., CHRISTOPHER A. JANUSZ, M.D., and CAMILA K. JANNIGER, M.D. University of Medicine and Dentistry at New Jersey-New Jersey Medical School, Newark, New Jersey Seborrheic dermatitis affects the scalp, central face, and anterior chest. In adolescents and adults, it often presents as scalp scaling (dandruff). Seborrheic dermatitis also may cause mild to marked erythema of the nasolabial fold, often with scaling. Stress can cause flare-ups. The scales are greasy, not dry, as commonly thought. An uncommon generalized form in infants may be linked to immunodeficiencies. Topical therapy primarily consists of antifungal agents and low-potency steroids. New topical calcineurin inhibitors (immunomodulators) sometimes are administered. (Am Fam Physician 2006;74:125-30. Copyright © 2006 American Academy of Family Physicians.) eborrheic dermatitis can affect patients levels, fungal infections, nutritional deficits, from infancy to old age.1-3 The con- neurogenic factors) are associated with the dition most commonly occurs in condition. The possible hormonal link may infants within the first three months explain why the condition appears in infancy, S of life and in adults at 30 to 60 years of age. In disappears spontaneously, then reappears adolescents and adults, it usually presents as more prominently after puberty. A more scalp scaling (dandruff) or as mild to marked causal link seems to exist between seborrheic erythema of the nasolabial fold during times dermatitis and the proliferation of Malassezia of stress or sleep deprivation. The latter type species (e.g., Malassezia furfur, Malassezia tends to affect men more often than women ovalis) found in normal dimorphic human and often is precipitated by emotional stress. -

Syphilis Staging and Treatment Syphilis Is a Sexually Transmitted Disease (STD) Caused by the Treponema Pallidum Bacterium
Increasing Early Syphilis Cases in Illinois – Syphilis Staging and Treatment Syphilis is a sexually transmitted disease (STD) caused by the Treponema pallidum bacterium. Syphilis can be separated into four different stages: primary, secondary, early latent, and late latent. Ocular and neurologic involvement may occur during any stage of syphilis. During the incubation period (time from exposure to clinical onset) there are no signs or symptoms of syphilis, and the individual is not infectious. Incubation can last from 10 to 90 days with an average incubation period of 21 days. During this period, the serologic testing for syphilis will be non-reactive but known contacts to early syphilis (that have been exposed within the past 90 days) should be preventatively treated. Syphilis Stages Primary 710 (CDC DX Code) Patient is most infectious Chancre (sore) must be present. It is usually marked by the appearance of a single sore, but multiple sores are common. Chancre appears at the spot where syphilis entered the body and is usually firm, round, small, and painless. The chancre lasts three to six weeks and will heal without treatment. Without medical attention the infection progresses to the secondary stage. Secondary 720 Patient is infectious This stage typically begins with a skin rash and mucous membrane lesions. The rash may manifest as rough, red, or reddish brown spots on the palms of the hands, soles of the feet, and/or torso and extremities. The rash does usually does not cause itching. Rashes associated with secondary syphilis can appear as the chancre is healing or several weeks after the chancre has healed. -

Disseminated Mycobacterium Tuberculosis with Ulceronecrotic Cutaneous Disease Presenting As Cellulitis Kelly L
Lehigh Valley Health Network LVHN Scholarly Works Department of Medicine Disseminated Mycobacterium Tuberculosis with Ulceronecrotic Cutaneous Disease Presenting as Cellulitis Kelly L. Reed DO Lehigh Valley Health Network, [email protected] Nektarios I. Lountzis MD Lehigh Valley Health Network, [email protected] Follow this and additional works at: http://scholarlyworks.lvhn.org/medicine Part of the Dermatology Commons, and the Medical Sciences Commons Published In/Presented At Reed, K., Lountzis, N. (2015, April 24). Disseminated Mycobacterium Tuberculosis with Ulceronecrotic Cutaneous Disease Presenting as Cellulitis. Poster presented at: Atlantic Dermatological Conference, Philadelphia, PA. This Poster is brought to you for free and open access by LVHN Scholarly Works. It has been accepted for inclusion in LVHN Scholarly Works by an authorized administrator. For more information, please contact [email protected]. Disseminated Mycobacterium Tuberculosis with Ulceronecrotic Cutaneous Disease Presenting as Cellulitis Kelly L. Reed, DO and Nektarios Lountzis, MD Lehigh Valley Health Network, Allentown, Pennsylvania Case Presentation: Discussion: Patient: 83 year-old Hispanic female Cutaneous tuberculosis (CTB) was first described in the literature in 1826 by Laennec and has since been History of Present Illness: The patient presented to the hospital for chest pain and shortness of breath and was treated for an NSTEMI. She was noted reported to manifest in a variety of clinical presentations. The most common cause is infection with the to have redness and swelling involving the right lower extremity she admitted to having for 5 months, which had not responded to multiple courses of antibiotics. She acid-fast bacillus Mycobacterium tuberculosis via either primary exogenous inoculation (direct implantation resided in Puerto Rico but recently moved to the area to be closer to her children. -

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group D07A (Corticosteroids, Plain) Table of Contents Page INTRODUCTION 4 DISCLAIMER 6 GLOSSARY OF TERMS USED IN THIS DOCUMENT 7 ACTIVE SUBSTANCES Methylprednisolone (ATC: D07AA01) 8 Hydrocortisone (ATC: D07AA02) 9 Prednisolone (ATC: D07AA03) 11 Clobetasone (ATC: D07AB01) 13 Hydrocortisone butyrate (ATC: D07AB02) 16 Flumetasone (ATC: D07AB03) 18 Fluocortin (ATC: D07AB04) 21 Fluperolone (ATC: D07AB05) 22 Fluorometholone (ATC: D07AB06) 23 Fluprednidene (ATC: D07AB07) 24 Desonide (ATC: D07AB08) 25 Triamcinolone (ATC: D07AB09) 27 Alclometasone (ATC: D07AB10) 29 Hydrocortisone buteprate (ATC: D07AB11) 31 Dexamethasone (ATC: D07AB19) 32 Clocortolone (ATC: D07AB21) 34 Combinations of Corticosteroids (ATC: D07AB30) 35 Betamethasone (ATC: D07AC01) 36 Fluclorolone (ATC: D07AC02) 39 Desoximetasone (ATC: D07AC03) 40 Fluocinolone Acetonide (ATC: D07AC04) 43 Fluocortolone (ATC: D07AC05) 46 2 Diflucortolone (ATC: D07AC06) 47 Fludroxycortide (ATC: D07AC07) 50 Fluocinonide (ATC: D07AC08) 51 Budesonide (ATC: D07AC09) 54 Diflorasone (ATC: D07AC10) 55 Amcinonide (ATC: D07AC11) 56 Halometasone (ATC: D07AC12) 57 Mometasone (ATC: D07AC13) 58 Methylprednisolone Aceponate (ATC: D07AC14) 62 Beclometasone (ATC: D07AC15) 65 Hydrocortisone Aceponate (ATC: D07AC16) 68 Fluticasone (ATC: D07AC17) 69 Prednicarbate (ATC: D07AC18) 73 Difluprednate (ATC: D07AC19) 76 Ulobetasol (ATC: D07AC21) 77 Clobetasol (ATC: D07AD01) 78 Halcinonide (ATC: D07AD02) 81 LIST OF AUTHORS 82 3 INTRODUCTION The availability of medicines with or without a medical prescription has implications on patient safety, accessibility of medicines to patients and responsible management of healthcare expenditure. The decision on prescription status and related supply conditions is a core competency of national health authorities. -

Scalp Eczema Factsheet the Scalp Is an Area of the Body That Can Be Affected by Several Types of Eczema
12 Scalp eczema factsheet The scalp is an area of the body that can be affected by several types of eczema. The scalp may be dry, itchy and scaly in a chronic phase and inflamed (red), weepy and painful in an acute (eczema flare) phase. Aside from eczema, there are a number of reasons why the scalp can become dry and itchy (e.g. psoriasis, fungal infection, ringworm, head lice etc.), so it is wise to get a firm diagnosis if there is uncertainty. Types of eczema • Hair clips and headgear – especially those containing that affect the scalp rubber or nickel. Seborrhoeic eczema (dermatitis) is one of the most See the NES booklet on Contact Dermatitis for more common types of eczema seen on the scalp and hairline. details. It can affect babies (cradle cap), children and adults. The Irritant contact dermatitis is a type of eczema that skin appears red and scaly and there is often dandruff as occurs when the skin’s surface is irritated by a substance well, which can vary in severity. There may also be a rash that causes the skin to become dry, red and itchy. on other parts of the face, such as around the eyebrows, For example, shampoos, mousses, hair gels, hair spray, eyelids and sides of the nose. Seborrhoeic eczema can perm solution and fragrance can all cause irritant contact become infected. See the NES factsheets on Adult dermatitis. See the NES booklet on Contact Dermatitis for Seborrhoeic Dermatitis and Infantile Seborrhoeic more details. Dermatitis and Cradle Cap for more details. -

Pdf/Bookshelf NBK368467.Pdf
BMJ 2019;365:l4159 doi: 10.1136/bmj.l4159 (Published 28 June 2019) Page 1 of 11 Practice BMJ: first published as 10.1136/bmj.l4159 on 28 June 2019. Downloaded from PRACTICE CLINICAL UPDATES Syphilis OPEN ACCESS Patrick O'Byrne associate professor, nurse practitioner 1 2, Paul MacPherson infectious disease specialist 3 1School of Nursing, University of Ottawa, Ottawa, Ontario K1H 8M5, Canada; 2Sexual Health Clinic, Ottawa Public Health, Ottawa, Ontario K1N 5P9; 3Division of Infectious Diseases, Ottawa Hospital General Campus, Ottawa, Ontario What you need to know Box 1: Symptoms of syphilis by stage of infection (see fig 1) • Incidence rates of syphilis have increased substantially around the Primary world, mostly affecting men who have sex with men and people infected • Symptoms appear 10-90 days (mean 21 days) after exposure with HIV http://www.bmj.com/ • Main symptom is a <2 cm chancre: • Have a high index of suspicion for syphilis in any sexually active patient – Progresses from a macule to papule to ulcer over 7 days with genital lesions or rashes – Painless, solitary, indurated, clean base (98% specific, 31% sensitive) • Primary syphilis classically presents as a single, painless, indurated genital ulcer (chancre), but this presentation is only 31% sensitive; – On glans, corona, labia, fourchette, or perineum lesions can be painful, multiple, and extra-genital – A third are extragenital in men who have sex with men and in women • Diagnosis is usually based on serology, using a combination of treponemal and non-treponemal tests. Syphilis remains sensitive to • Localised painless adenopathy benzathine penicillin G Secondary on 24 September 2021 by guest. -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA).