Steadman Hawkins
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Al Sise Outstanding Alpine Masters Award
2017 U.S. SKI & SNOWBOARD AWARDS MANUAL U.S. Ski & Snowboard Awards 1 July 20, 2017 TO: U. S. Ski & Snowboard Sport Committee Chairs U. S. Ski & Snowboard Sport Directors U. S. Ski & Snowboard Awards Working Group FROM: Tom Kelly, Awards WG Liaison Bill Slattery, Chairman, U. S. Ski & Snowboard Awards Working Group Following is a complete outline of U. S. Ski & Snowboard’s organizational awards, designed to honor athletes, coaches, officials and volunteers for service on behalf of our ski and snowboard athletes. This manual is designed to assist you in management of awards selection within your sport, and to represent your sport in selection of organizational awards. It also includes a guideline for future awards you may wish to consider in your sport. As a sport committee chair, sport director, we would like you to be working on your nominations during the course of the season, so that you can provide detailed nominations no later than April 2. We will send out nomination information and convene a conference call on April 5 at 3:00 p.m. mountain time so that the working group can participate in a discussion of the award nominations. Thank you for your cooperation! U.S. Ski & Snowboard Awards 2 TABLE OF CONTENTS Page U. S. SKI & SNOWBOARD AWARDS WORKING GROUP............................................................................................... 4 AWARDS RESPONSIBILITIES OF SPORT COMMITTEES ............................................................................................. 5 DISCRETIONARY AWARDS SELECTION PROCESS .................................................................................................... -

Directory of Public Elementary and Secondary Education Agencies, 2000-2001
DOCUMENT RESUME ED 472 649 EA 032 306 AUTHOR McDowell, Lena M.; Sietsema, John P. TITLE Directory of Public Elementary and Secondary Education Agencies, 2000-2001. INSTITUTION National Center for Education Statistics (ED), Washington, DC. REPORT NO NCES-2003-310 PUB DATE 2002-11-00 NOTE 410p.; For the 1999-2000 Directory, see ED 464 396. AVAILABLE FROM ED Pubs, P.O. Box 1398, Jessup, MD 20794-1398. Tel: 877 -433- 7827 (Toll Free). For full text: http://nces.ed.gov/pubs2003/2003310.pdf. PUB TYPE Numerical/Quantitative Data (110) Reference Materials Directories /Catalogs (132) EDRS PRICE EDRS Price MF01/PC17 Plus Postage. DESCRIPTORS Elementary Secondary Education; Enrollment; Government Publications; *Public Agencies; *Public Schools; *School Districts; School Personnel; School Statistics; State Departments of Education IDENTIFIERS Grade Span Configuration ABSTRACT This directory lists all public elementary and secondary education agencies in the 50 states, the District of Columbia, five outlying areas, the Bureau of Indian Affairs, and the Department of Defense, as reported from the National Center for Education Statistics (NCES) Common Core of Data (CCD) Local Education Agency Universe data collection of spring 2001. In the introduction, several tables summarizing the file contents are provided. The seven types of agencies listed include regular school districts, supervisory union components, supervisory union administrative centers, regional educational service agencies, state-operated agencies, federally operated agencies, and other agencies that cannot be appropriately classified using another CCD designation. The directory provides up to 12 items of information for each public elementary and secondary agency listed: state, name of agency, mailing address, telephone number, name of county, metropolitan status code, grade span, total student membership, number of regular high school graduates for the 1999-2000 school year, number of students with an individualized education program (IEP), number of teachers, and number of schools. -

In the Spirit of Harambee
THE EQUAL RIGHTS TRUST IN PARTNERSHIP WITH THE KENYA HUMAN RIGHTS COMMISSION In the Spirit of Harambee Addressing Discrimination and Inequality in Kenya ERT Country Report Series: 1 London, February 2012 The Equal Rights Trust (ERT) is an independent international organisation whose purpose is to combat discrimination and promote equality as a fundamental human right and a basic principle of social justice. Established as an advocacy organisation, resource centre and think tank, ERT focuses on the complex relationship between different types of discrimination, developing strategies for translating the principles of equality into practice. © February 2012 The Equal Rights Trust © Cover February 2012 Dafina Gueorguieva Printed in the UK by Prontaprint Bayswater DesignISBN: and layout: 978-0-9560717-5-0 Dafina Gueorguieva All rights reserved. No part of this publication may be translated, reproduced, stored in a retrieval system or transmitted in any form or by other means without the prior written permission of the publisher, or a licence for restricted copying from the Copyright Licensing Agency Ltd., UK, or the Copyright Clearance Centre, USA. The Equal Rights Trust 126 North End Road London W14 9PP United Kingdom Tel. +44 (0) 207 610 2786 Fax: +44 (0) 203 441 7436 www.equalrightstrust.org The Equal Rights Trust is a company limited by guarantee incorporated in England, and a registered charity. Company number 5559173. Charity number 1113288. “Our motto ‘harambee’* was conceived in the realisation of the challenge of national building that now lies ahead of us. It was conceived in the knowl- edge that to meet this challenge, the government and the people of Kenya must pull together. -

"DO DOGS APE?" OR "DO APES DOG?" and DOES Rr MATTER? BROADENING and DEEPENING COGNITIVE ETHOLOGY
"DO DOGS APE?" OR "DO APES DOG?" AND DOES rr MATTER? BROADENING AND DEEPENING COGNITIVE ETHOLOGY By MA~c BEKOFF4' "Certainlyit seems like a dirty double-cross to enter into a relationshipof trust and affection with any creaturethat can enter into such a relationship, and then to be a party to'its premeditated and premature destruction."1 I. RAiN WrrHouT TmmDER, ANimAS Wrrour MINDS In Rain Without Thunder, Gary Francione raises numerous impor- tant issues and takes on many important people.2 The phrase "rain with- out thunder" made me think about the notion of animals without minds- animals without thoughts or feelings. This idea is troublesome for the nonhuman animals (hereafter animals) to whom it is attributed because it is much easier for humans to exploit animals when we believe that they don't have thoughts or feelings. I have been privileged to study various aspects of animal behavior for over 25 years, including animal cognition3 (cognitive ethology), and have attempted to learn more about how the study of animal cognition can aid discussions of animal protection. 4 As a * Professor of Biology, University of Colorado, Boulder;, A.B. and PILD., Washington University, St. Louis, Missouri; Guggenheim Fellow and Fellow of the Animal Behavior Soci- ety; Correspondence: Marc Bekoff, 296 Canyonside Drive, Boulder, Colorado 80302; Emaih [email protected] 1 LAWRENCE E. JoHNsoN, A MORALLY DEEP WoRLD: AN E.sxe*ON MORAL SIGNIFICANCE AND ENvmonwNAL ETmcs 122 (1991). 2 GARY L. FPNtcioNE, RAiN WmoUr TnuDER TIE IDEOLOGY OF mm.EAn,,AL RPiurrs MovmiErr (1996). 3 INTERPRrrATION AND EXPLANATION IN T-E STUDY OF Amm- Bcsxion (Marc Bekoff & Dale Jamieson eds., 1990); READINGS 1N AmAL COGNMON (Marc Bekoff & Dale Jamieson eds., 1996); Marc Bekoff & Colin Allen, Cognitive Ethology: Slayers, Skeptics, and Propo- nents, in ANmRoPoiORPmS.e ANscDoTE, ANzmms: TuE EMpERiO's NEW CLOTnts? 313 (Rob- ert W. -
Collegian 2007 04 25.Pdf (15.00Mb)
College avenue hits raCks today! THE ROCKY MOUNTAIN Fort Collins, Colorado COLLEGIAN Volume 115 | No. 149 wednesday, april 25, 2007 www.collegian.com THE STUDENT VOICE OF COLORADO STATE UNIVERSITY SINCE 1891 the LIMELIGHT GOING VetHOME delivers mercy By Brandon lowrey contacts The Rocky Mountain Collegian • For grief counselors at the Argus In stitute at the CSU Veterinary Teaching Hospital: LOVELAND — Joni O’Neill runs a hand (970) 217-7069 along her black Labrador’s coat. • Home to Heaven: (970) 412-6212 Jonah, lying down on a mat in the O’Neill family’s country-style home, answers excit- edly by wagging his tail. And if dogs grin, he’s grinning. sic. Her dark blue Toyota van fills with silence, His tongue shoots out to score a few quick and the silence fills with focus. kisses on O’Neill’s face. She manages to smile. She’s not religious, but she prays — a rem- But for a few moments too long, Jonah’s nant of her Catholic upbringing. old eyes stare up into hers. O’Neill finally Let it be a peaceful passing. Let everything looks away as tears and a stifled sob betray go well. her feelings. “It’s almost like a superstitious thing, This is how she wants it to end. now,” she says. “I wanted to put him down with a smile on Cooney recently performed her his face,” she said. “I put one down suffering 103rd euthanasia — about 30 procedures in before, and...” April, alone — unthinkable if she felt guilty, She trails off. even for a moment. -

Al Sise Outstanding Alpine Masters Award
2017 U.S. SKI & SNOWBOARD AWARDS MANUAL U.S. Ski & Snowboard Awards 1 July 20, 2017 TO: U. S. Ski & Snowboard Sport Committee Chairs U. S. Ski & Snowboard Sport Directors U. S. Ski & Snowboard Awards Working Group FROM: Tom Kelly, Awards WG Liaison Bill Slattery, Chairman, U. S. Ski & Snowboard Awards Working Group Following is a complete outline of U. S. Ski & Snowboard’s organizational awards, designed to honor athletes, coaches, officials and volunteers for service on behalf of our ski and snowboard athletes. This manual is designed to assist you in management of awards selection within your sport, and to represent your sport in selection of organizational awards. It also includes a guideline for future awards you may wish to consider in your sport. As a sport committee chair, sport director, we would like you to be working on your nominations during the course of the season, so that you can provide detailed nominations no later than April 2. We will send out nomination information and convene a conference call on April 5 at 3:00 p.m. mountain time so that the working group can participate in a discussion of the award nominations. Thank you for your cooperation! U.S. Ski & Snowboard Awards 2 TABLE OF CONTENTS Page U. S. SKI & SNOWBOARD AWARDS WORKING GROUP ...................................................................................................... 4 AWARDS RESPONSIBILITIES OF SPORT COMMITTEES ..................................................................................................... 5 DISCRETIONARY AWARDS SELECTION -
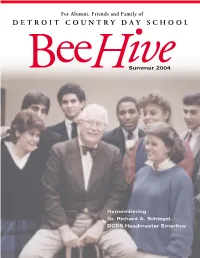
For Alumni, Friends and Family of DETROIT COUNTRY DAY SCHOOL
For Alumni, Friends and Family of DETROIT COUNTRY DAY SCHOOL Summer 2004 Remembering Dr. Richard A. Schlegel, DCDS Headmaster Emeritus THE BEEHIVE IS PUBLISHED TWICE ANNUALLY FOR ALUMNI, PARENTS, PAST PARENTS, STUDENTS AND FRIENDS OF DETROIT COUNTRY DAY SCHOOL HEADMASTER GERALD T. HANSEN EDITOR MARY ELLEN ROWE PHOTOGRAPHY SCOTT C. BERTSCHY CLAYTON T. MATTHEWS DEVELOPMENT OFFICE STAFF DIRECTOR OF DEVELOPMENT SCOTT C. BERTSCHY ASSOCIATE DIRECTOR OF DEVELOPMENT BARBARA A. MOWER AND PARENT RELATIONS DIRECTOR OF ALUMNI RELATIONS KIRA T. MANN ASSOCIATE DIRECTOR OF ALUMNI RELATIONS JEAN L. CROSSLEY DIRECTOR OF COMMUNICATIONS CLAYTON T. MATTHEWS ASSOCIATE DIRECTOR OF COMMUNICATIONS MARY ELLEN ROWE ADMINISTRATIVE ASSISTANT KIMBERLY M. ARNOLD ADMINISTRATIVE ASSISTANT DONNA CRONBERGER ADMINISTRATIVE ASSISTANT JACKIE MARTIN BEEHIVE DESIGN AND PRODUCTION SUSAN BACHMAN ’76, MARKET ARTS Front cover: Dr. Schlegel surrounds himself with Country Day students in 1986. (L-R) Natalie Greenspan ‘86, Bill Passer ‘86, Keith Fenton ‘86, Dr. Schlegel, Dennis Archer ‘86, Kathy Williams ‘87, Carol Gillow Giles ‘86 and David Levine ‘86. Contents BeeHive • Summer 2004 A NOTE FROM THE HEADMASTER 2 16 BEEHIVE CORRECTIONS 3 CAMPUS BRIEFS 3 REMEMBERING DR. SCHLEGEL 6 CLASS OF 2004 COMMENCEMENT 10 2004 HONORS CONVOCATION 12 AS SEEN IN... THE TRAVERSE CITY 13 RECORD EAGLE DCDS NAMED MICROSOFT CENTER 14 23 OF INNOVATION 24 DCDS CELEBRATES THE ARTS 16 BEACH BASH! AUCTION 2004 18 FLAT STANLEY MANIA AT THE 19 LOWER SCHOOL JUNIOR SCHOOL MOOSE 20 REVEALS HIS ROOTS VISITING ARTIST JACK GANTOS WROTE 22 THE BOOK ON STORYTELLING GRADE 7 FLORIDA TRIP 23 A DAY TIMES SPECIAL - HANDS ON 24 DETROIT GIVES BACK TO THE CITY DIRECTOR OF ALUMNI RELATIONS 25 MESSAGE CAREER DAY 2004 26 6 2004 REGIONAL RECEPTIONS 28 THAT’S AMORÉ! FINE DINING WITH 29 ADRIAN TONON ‘91 ALUMNI SPORTS 32 ALUMNI MOTHERS’ LUNCHEON 34 RETIREMENTS 35 CLASS NOTES 37 IN MEMORIAM 45 32 CONTENTS 1 A Note from The Headmaster By Gerald T. -

RECEIVED Apri14, 2019 APR 0 5 2019
RECEIVED Apri14, 2019 APR 0 5 2019 Ben Haller BUREAU OF Kansas Department of Health and Environment ENVIRONMENTAL REMEDIATION Bureau of Environmental Remediation Remedial Section/Site Remediation Unit I 000 SW Jackson Street, Suite 420 Approved with Comments Topeka, Kansas 66612-1367 Date(s) /3 1-J '1-12.. ~ 2..D/1 RE: STF Suspected Waste Area Characterization Report Former Coastal Refinery, El Dorado, Kansas Dear Mr. Haller: On behalf of El Paso Merchant Energy-Petroleum Company (EPME-PC), Stantec Consulting Services, Inc. (Stantec) submits this South Tank Farm (STF) Suspected Waste Area Characterization report presenting data to further delineate and characterize a waste-like material reported in the September 2009 Third Phase Environmental Investigation Report (Third Phase Investigation Report) for the former Coastal Refinery (Site) located in El Dorado, Kansas (Figure I). This work is being conducted as part of the Corrective Action Plan (CAP) called for in the Site Final Corrective Action Decision (CAD, November 20 16). In addition, during soil grading/earthwork completed in December 2018 to improve surface water drainage from a former STF bermed area, a second suspected waste are.a was discovered. Both areas are identified on Figure 2, they were investigated, and the findings are presented in this letter report. NORTH STF SUSPECTED WASTE AREA The North STF suspected waste area was identified in 2008 during the Third Phase Investigation. History Sixteen shallow borings were advanced (STFPSB-0 I through STFPSB-16) as part of the Third Phase Investigation to assess the extent of the buried material during pipeline removal activities. The borings shown on Figure 3 were installed using a Geoprobe® rig to a maximum depth of eight feet, transecting the area. -

Tax Hikes May Be Needed to Balance Budget
iianr^fst^r lEawtmg M? ralb MANCHESTER, CONN., FRIDAY, JANUARY 10, 1975- VOL. XCIV, No. 85 Manchester—A City of. Village Charm TWENTY PAGES PRICE: EIETEEN CENTS Gov, Grasso Still Opposes Income Tax Tax Hikes May Be Needed to Balance Budget HARTFORD (UPI) - Gov. Ella T. When asked whether she would request Mrs. Grasso also said there will be cuts “The problem now is to stay off the red.” Gaffney’s nomination by former Gov. millions is no easy task, but any Grasso, who campaigned on a pledge of no the Democratic-controlled legislature for in the state labor force, either through at Throughout the campaign against her state tax increases, today said some tax a tax increase for the remainder of the Thomas J. Meskill has been opposed by homemaker knows its the little savings trition or outright layoffs, although she Republican opponent, Robert H. Steele, the Connecticut Bar Association and he hikes may be needed in fiscal 1976 to present fiscal year, Mrs. Grasso said, ‘T declined to speculate on the number of and enough of them, that add up. Mrs. Grasso denied Steele’s charges the has been involved in the legislature’s balance the budget. have no intention to do so.” workers who will be affected. On Thursday, the day after her in Democratic platform contained many probe into irregularities in state leasing “I would think we have to look forward auguration, Mrs Grasso told her agency Deficit Forecast “I would think there would be some spending programs that would require tax practices. to some higher taxes,” she said in her firings,” she said. -

New Observations of Meat Eating and Sharing in Wild Bonobos (Pan Paniscus) at Iyema, Lomako Forest Reserve, Democratic Republic of the Congo
Short Communication Folia Primatol 2019;90:179–189 Received: September 9, 2018 DOI: 10.1159/000496026 Accepted after revision: December 1, 2018 Published online: March 19, 2019 New Observations of Meat Eating and Sharing in Wild Bonobos (Pan paniscus) at Iyema, Lomako Forest Reserve, Democratic Republic of the Congo a b b Monica L. Wakefield Alexana J. Hickmott Colin M. Brand a a b, c Ian Y. Takaoka Lindsey M. Meador Michel T. Waller b Frances J. White a Department of Sociology, Anthropology and Philosophy, Northern Kentucky b University, Highland Heights, KY, USA; Department of Anthropology, University of c Oregon, Eugene, OR, USA; Department of World Languages and Culture, Central Oregon Community College, Bend, OR, USA Keywords Behavioral diversity · Faunivory · Food sharing · Prey preference · Female control Abstract Bonobos (Pan paniscus) consume a variety of vertebrates, although direct observa- tions remain relatively rare compared to chimpanzees (Pan troglodytes). We report the first direct observations of meat eating and sharing among bonobos at Iyema, Lomako Forest, Democratic Republic of Congo. We collected meat consumption data ad libitum from June to November 2017 over 176.5 observation hours and conducted monthly censuses to measure the abundance of potential prey species. We observed 3 occasions of duiker consumption and found indirect evidence of meat consumption twice (n = 5). We identified the prey species as Weyn’s duiker (Cephalophus weynsi) in all 4 cases that we saw the carcass. This species was the most abundant duiker species at Iyema, but other potential prey species were also available. Meat sharing was observed or inferred during all 3 observations. -

Available Only Within the Gorilla Journal PDF File
Gorilla Journal Journal of Berggorilla & Regenwald Direkthilfe No. 32, June 2006 The Stories of Bwindi-Impenetra- The Cross-Sanaga Humans and Go- Mugaruka and ble: 15 Years as a Gorillas: North- rillas – what Kind Chimanuka National Park ernmost Gorilla of Relationship? Populations BERGGORILLA & REGENWALD DIREKTHILFE Authors of this Issue a scientifi c assistant at the Inst. of Bio- CONTENTS science at the University of Rostock. D. R. Congo 3 Stephen Asuma is a Field Offi cer Jean Claude Kyungu Kasolene Trip to Kahuzi-Biega 3 for IGCP in Uganda. led an ecology NGO, the Tayna Gorilla Attack on the Mugaba Patrol Post 3 James Byamukama has worked Reserve and the Walikale Community Le Gorille Magazine 2006 4 for IGCP as a Field Offi cer since April Gorilla Reserve and is now Project Ma- The Stories of Mugaruka and Chi- 2004. Since 1991 he has worked with nager for Tshiabirimu Gorilla Project. manuka ... so far 4 the Uganda Forest Department and Dr. Eric Leroy is a virologist and the The Silverback Mugaruka 5 with UNDP/GEF. chief of the “Emerging Viruses Unit” in New Patrol Post at Mt. Tshiabirimu 6 Prof. Dr. Raymond Corbey is a the Centre International de Recherch- Uganda 8 philosopher and anthropologist who is es Médicales de Franceville, Gabon. Bwindi-Impenetrable: 15 Years 8 connected to the Dept. of Philosophy of Dr. Alastair McNeilage is currently HuGo – the Uganda Experience 10 Tilburg University and the Dept. of Ar- the director of the Institute of Tropical Cross River 13 chaeology of Leiden University. Forest Conservation in Bwindi. He has Trip to Nigeria 13 Prof. -

Happy Birthday Colo: US Gorilla Turns 60 the Nation’S Oldest Living Gorilla
HEALTH SATURDAY, DECEMBER 24, 2016 Happy birthday Colo: US gorilla turns 60 The nation’s oldest living gorilla COLUMBUS: She is a mother of three, crowd. “It’s all about connecting people years) by more than two decades. Other grandmother of 16, great-grandmother and wildlife,” he said. Colo is one of sev- age-defying zoo animals: of 12 and great-great-grandmother of eral elderly gorillas around the country. three. She recently had surgery to The oldest known living male gorilla, POLAR BEAR remove a malignant tumor, but doctors Ozzie, is 55 years old and lives at the Coldilocks, a 36-year-old polar bear at say she’s doing well. She’s Colo, the Atlanta Zoo, which has a geriatric gorilla the Philadelphia Zoo and considered KUCHKI: A picture taken on November 25, 2016 shows nation’s oldest living gorilla, and she specialty. At Seattle’s Woodland Park the oldest polar bear in the US The a policeman as he stands inside of an illicit vodka dis- turned 60 on Thursday at the Columbus Zoo, staff members use acupuncture, bears’ typical lifespan in captivity is 23 tillery. — AFP Zoo and Aquarium. Colo was the first massage, laser therapy, and heat and years. The zoo says treating her early for gorilla in the world born in a zoo and joint supplements to help Emma, a 13- kidney disease appears to have helped Russia works to abolish has surpassed the usual life expectancy year-old rabbit. At the National Zoo in prolong her life. of captive gorillas by two decades.