In Vivo Imaging of Engraftment and Enrichment of Lentiviral
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Atlas Antibodies in Breast Cancer Research Table of Contents
ATLAS ANTIBODIES IN BREAST CANCER RESEARCH TABLE OF CONTENTS The Human Protein Atlas, Triple A Polyclonals and PrecisA Monoclonals (4-5) Clinical markers (6) Antibodies used in breast cancer research (7-13) Antibodies against MammaPrint and other gene expression test proteins (14-16) Antibodies identified in the Human Protein Atlas (17-14) Finding cancer biomarkers, as exemplified by RBM3, granulin and anillin (19-22) Co-Development program (23) Contact (24) Page 2 (24) Page 3 (24) The Human Protein Atlas: a map of the Human Proteome The Human Protein Atlas (HPA) is a The Human Protein Atlas consortium cell types. All the IHC images for Swedish-based program initiated in is mainly funded by the Knut and Alice the normal tissue have undergone 2003 with the aim to map all the human Wallenberg Foundation. pathology-based annotation of proteins in cells, tissues and organs expression levels. using integration of various omics The Human Protein Atlas consists of technologies, including antibody- six separate parts, each focusing on References based imaging, mass spectrometry- a particular aspect of the genome- 1. Sjöstedt E, et al. (2020) An atlas of the based proteomics, transcriptomics wide analysis of the human proteins: protein-coding genes in the human, pig, and and systems biology. mouse brain. Science 367(6482) 2. Thul PJ, et al. (2017) A subcellular map of • The Tissue Atlas shows the the human proteome. Science. 356(6340): All the data in the knowledge resource distribution of proteins across all eaal3321 is open access to allow scientists both major tissues and organs in the 3. -
The Role of SAMHD1 in Restriction and Immune Sensing of Retroviruses and Retroelements
The role of SAMHD1 in restriction and immune sensing of retroviruses and retroelements Die Rolle von SAMHD1 in der Restriktion und Immunerkennung von Retroviren und Retroelementen Der Naturwissenschaftlichen Fakultät der Friedrich-Alexander-Universität Erlangen-Nürnberg zur Erlangung des Doktorgrades Dr. rer. nat. vorgelegt von Alexandra Herrmann aus Biberach an der Riß Als Dissertation genehmigt von der Naturwissenschaftlichen Fakultät der Friedrich-Alexander-Universität Erlangen-Nürnberg Tag der mündlichen Prüfung: 31.07.2018 Vorsitzender des Promotionsorgans: Prof. Dr. Georg Kreimer Gutachter: Prof. Dr. Lars Nitschke Prof. Dr. Manfred Marschall Table of content Table of content I. Summary ......................................................................................................................... 1 I. Zusammenfassung ......................................................................................................... 3 II. Introduction ..................................................................................................................... 5 1. The human immunodeficiency virus .................................................................................... 5 2. Transposable elements ......................................................................................................... 7 3. Host restriction factors ........................................................................................................ 10 4. The restriction factor SAMHD1 .......................................................................................... -

Canine Influenza Virus Is Mildly Restricted by Canine Tetherin Protein
viruses Article Canine Influenza Virus is Mildly Restricted by Canine Tetherin Protein Yun Zheng 1,2,3,†, Xiangqi Hao 1,2,3,†, Qingxu Zheng 1,2,3, Xi Lin 1,2,3, Xin Zhang 1,2,3, Weijie Zeng 1,2,3, Shiyue Ding 1, Pei Zhou 1,2,3,* and Shoujun Li 1,2,3,* 1 College of Veterinary Medicine, South China Agricultural University, Guangzhou 510642, China; [email protected] (Y.Z.); [email protected] (X.H.); [email protected] (Q.Z.); [email protected] (X.L.); [email protected] (X.Z.); [email protected] (W.Z.); [email protected] (S.D.) 2 Guangdong Provincial Key Laboratory of Prevention and Control for Severe Clinical Animal Diseases, Guangzhou 510642, China 3 Guangdong Provincial Pet Engineering Technology Research Center, Guangzhou 510642, China * Correspondence: [email protected] (P.Z.); [email protected] (S.L.) † These authors contributed equally to this work. Received: 10 July 2018; Accepted: 10 October 2018; Published: 16 October 2018 Abstract: Tetherin (BST2/CD317/HM1.24) has emerged as a key host-cell ·defence molecule that acts by inhibiting the release and spread of diverse enveloped virions from infected cells. We analysed the biological features of canine tetherin and found it to be an unstable hydrophilic type I transmembrane protein with one transmembrane domain, no signal peptide, and multiple glycosylation and phosphorylation sites. Furthermore, the tissue expression profile of canine tetherin revealed that it was particularly abundant in immune organs. The canine tetherin gene contains an interferon response element sequence that can be regulated and expressed by canine IFN-α. -

Tetherin/BST-2 Promotes Dendritic Cell Activation and Function During Acute Retrovirus Infection Received: 21 October 2015 Sam X
www.nature.com/scientificreports OPEN Tetherin/BST-2 promotes dendritic cell activation and function during acute retrovirus infection Received: 21 October 2015 Sam X. Li1,2, Bradley S. Barrett1, Kejun Guo1, George Kassiotis3, Kim J. Hasenkrug4, Accepted: 06 January 2016 Ulf Dittmer5, Kathrin Gibbert5 & Mario L. Santiago1,2 Published: 05 February 2016 Tetherin/BST-2 is a host restriction factor that inhibits retrovirus release from infected cells in vitro by tethering nascent virions to the plasma membrane. However, contradictory data exists on whether Tetherin inhibits acute retrovirus infection in vivo. Previously, we reported that Tetherin-mediated inhibition of Friend retrovirus (FV) replication at 2 weeks post-infection correlated with stronger natural killer, CD4+ T and CD8+ T cell responses. Here, we further investigated the role of Tetherin in counteracting retrovirus replication in vivo. FV infection levels were similar between wild-type (WT) and Tetherin KO mice at 3 to 7 days post-infection despite removal of a potent restriction factor, Apobec3/Rfv3. However, during this phase of acute infection, Tetherin enhanced myeloid dendritic cell (DC) function. DCs from infected, but not uninfected, WT mice expressed significantly higher MHC class II and the co-stimulatory molecule CD80 compared to Tetherin KO DCs. Tetherin-associated DC activation during acute FV infection correlated with stronger NK cell responses. Furthermore, Tetherin+ DCs from FV-infected mice more strongly stimulated FV-specific CD4+ T cells ex vivo compared to Tetherin KO DCs. The results link the antiretroviral and immunomodulatory activity of Tetherin in vivo to improved DC activation and MHC class II antigen presentation. Restriction factors are host-encoded type I interferon-stimulated genes (ISG) that directly inhibit virus replication1. -
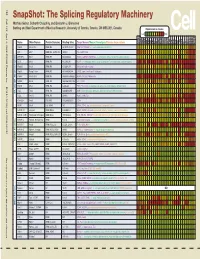
Snapshot: the Splicing Regulatory Machinery Mathieu Gabut, Sidharth Chaudhry, and Benjamin J
192 Cell SnapShot: The Splicing Regulatory Machinery Mathieu Gabut, Sidharth Chaudhry, and Benjamin J. Blencowe 133 Banting and Best Department of Medical Research, University of Toronto, Toronto, ON M5S 3E1, Canada Expression in mouse , April4, 2008©2008Elsevier Inc. Low High Name Other Names Protein Domains Binding Sites Target Genes/Mouse Phenotypes/Disease Associations Amy Ceb Hip Hyp OB Eye SC BM Bo Ht SM Epd Kd Liv Lu Pan Pla Pro Sto Spl Thy Thd Te Ut Ov E6.5 E8.5 E10.5 SRp20 Sfrs3, X16 RRM, RS GCUCCUCUUC SRp20, CT/CGRP; −/− early embryonic lethal E3.5 9G8 Sfrs7 RRM, RS, C2HC Znf (GAC)n Tau, GnRH, 9G8 ASF/SF2 Sfrs1 RRM, RS RGAAGAAC HipK3, CaMKIIδ, HIV RNAs; −/− embryonic lethal, cond. KO cardiomyopathy SC35 Sfrs2 RRM, RS UGCUGUU AChE; −/− embryonic lethal, cond. KO deficient T-cell maturation, cardiomyopathy; LS SRp30c Sfrs9 RRM, RS CUGGAUU Glucocorticoid receptor SRp38 Fusip1, Nssr RRM, RS ACAAAGACAA CREB, type II and type XI collagens SRp40 Sfrs5, HRS RRM, RS AGGAGAAGGGA HipK3, PKCβ-II, Fibronectin SRp55 Sfrs6 RRM, RS GGCAGCACCUG cTnT, CD44 DOI 10.1016/j.cell.2008.03.010 SRp75 Sfrs4 RRM, RS GAAGGA FN1, E1A, CD45; overexpression enhances chondrogenic differentiation Tra2α Tra2a RRM, RS GAAARGARR GnRH; overexpression promotes RA-induced neural differentiation SR and SR-Related Proteins Tra2β Sfrs10 RRM, RS (GAA)n HipK3, SMN, Tau SRm160 Srrm1 RS, PWI AUGAAGAGGA CD44 SWAP Sfrs8 RS, SWAP ND SWAP, CD45, Tau; possible asthma susceptibility gene hnRNP A1 Hnrnpa1 RRM, RGG UAGGGA/U HipK3, SMN2, c-H-ras; rheumatoid arthritis, systemic lupus -

Modulating Antiviral Response Via CRISPR–Cas Systems
viruses Review Immunity and Viral Infections: Modulating Antiviral Response via CRISPR–Cas Systems Sergey Brezgin 1,2,3,† , Anastasiya Kostyusheva 1,†, Ekaterina Bayurova 4 , Elena Volchkova 5, Vladimir Gegechkori 6 , Ilya Gordeychuk 4,7, Dieter Glebe 8 , Dmitry Kostyushev 1,3,*,‡ and Vladimir Chulanov 1,3,5,‡ 1 National Medical Research Center of Tuberculosis and Infectious Diseases, Ministry of Health, 127994 Moscow, Russia; [email protected] (S.B.); [email protected] (A.K.); [email protected] (V.C.) 2 Institute of Immunology, Federal Medical Biological Agency, 115522 Moscow, Russia 3 Scientific Center for Genetics and Life Sciences, Division of Biotechnology, Sirius University of Science and Technology, 354340 Sochi, Russia 4 Chumakov Federal Scientific Center for Research and Development of Immune-and-Biological Products of Russian Academy of Sciences, 108819 Moscow, Russia; [email protected] (E.B.); [email protected] (I.G.) 5 Department of Infectious Diseases, Sechenov University, 119991 Moscow, Russia; [email protected] 6 Department of Pharmaceutical and Toxicological Chemistry, Sechenov University, 119991 Moscow, Russia; [email protected] 7 Department of Organization and Technology of Immunobiological Drugs, Sechenov University, 119991 Moscow, Russia 8 National Reference Center for Hepatitis B Viruses and Hepatitis D Viruses, Institute of Medical Virology, Justus Liebig University of Giessen, 35392 Giessen, Germany; [email protected] * Correspondence: [email protected] † Co-first authors. Citation: Brezgin, S.; Kostyusheva, ‡ Co-senior authors. A.; Bayurova, E.; Volchkova, E.; Gegechkori, V.; Gordeychuk, I.; Glebe, Abstract: Viral infections cause a variety of acute and chronic human diseases, sometimes resulting D.; Kostyushev, D.; Chulanov, V. Immunity and Viral Infections: in small local outbreaks, or in some cases spreading across the globe and leading to global pandemics. -

Logistic Regression Analysis for the Identification of the Metastasis-Associated Signaling Pathways of Osteosarcoma
INTERNATIONAL JOURNAL OF MOLECULAR MEDICINE 41: 1233-1244, 2018 Logistic regression analysis for the identification of the metastasis-associated signaling pathways of osteosarcoma YANG LIU1, WEI SUN2, XIAOJUN MA2, YUEDONG HAO3, GANG LIU3, XIAOHUI HU3, HOULAI SHANG3, PENGFEI WU3, ZEXUE ZHAO3 and WEIDONG LIU3 1Department of Orthopedics, Affiliated Hospital of Inner Mongolia University for The Nationalities, Tongliao, Inner Mongolia 028007; 2Department of Orthopaedics, Shanghai General Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai 200080; 3Department of Orthopedics, Huai'an First People's Hospital, Nanjing Medical University, Huai'an, Jiangsu 223300, P.R. China Received February 20, 2017; Accepted September 26, 2017 DOI: 10.3892/ijmm.2018.3360 Abstract. Osteosarcoma (OS) is the most common histological migration were identified as the terms that were significantly type of primary bone cancer. The present study was designed different. ICAM1, PDGFB, PDGFRB and TGFB1 were iden- to identify the key genes and signaling pathways involved in the tified to be enriched in cell migration and regulation of cell metastasis of OS. Microarray data of GSE39055 were down- migration. Nucleotide excision repair and the Wnt signaling loaded from the Gene Expression Omnibus database, which pathway were the metastasis-associated pathways of OS. In included 19 OS biopsy specimens before metastasis (control addition, ICAM1, PDGFB, PDGFRB and TGFB1, which were group) and 18 OS biopsy specimens after metastasis (case involved in cell migration and regulation of cell migration may group). After the differentially expressed genes (DEGs) were affect the metastasis of OS. identified using the Linear Models for Microarray Analysis package, hierarchical clustering analysis and unsupervised Introduction clustering analysis were performed separately, using orange software and the self-organization map method. -

Endocytosis Elicited by Nectins Transfers Cytoplasmic Cargo, Including Infectious Material, Between Cells Alex R
© 2019. Published by The Company of Biologists Ltd | Journal of Cell Science (2019) 132, jcs235507. doi:10.1242/jcs.235507 RESEARCH ARTICLE Trans-endocytosis elicited by nectins transfers cytoplasmic cargo, including infectious material, between cells Alex R. Generous1,2, Oliver J. Harrison3, Regina B. Troyanovsky4, Mathieu Mateo1,*, Chanakha K. Navaratnarajah1, Ryan C. Donohue1,2, Christian K. Pfaller1,2, Olga Alekhina5, Alina P. Sergeeva3,6, Indrajyoti Indra4, Theresa Thornburg7,‡, Irina Kochetkova7, Daniel D. Billadeau5, Matthew P. Taylor7, Sergey M. Troyanovsky4, Barry Honig3,6, Lawrence Shapiro3 and Roberto Cattaneo1,2,§ ABSTRACT development, where the Bride of sevenless protein is internalized by the Sevenless tyrosine kinase receptor (Cagan et al., 1992). Here, we show that cells expressing the adherens junction protein Transfer of specific transmembrane proteins also occurs during nectin-1 capture nectin-4-containing membranes from the surface tissue patterning in embryonic development of higher of adjacent cells in a trans-endocytosis process. We find that vertebrates, during epithelial cell movement and at the immune internalized nectin-1–nectin-4 complexes follow the endocytic synapse (Gaitanos et al., 2016; Hudrisier et al., 2001; Marston et al., pathway. The nectin-1 cytoplasmic tail controls transfer: its deletion 2003; Matsuda et al., 2004; Qureshi et al., 2011). At the immune prevents trans-endocytosis, while its exchange with the nectin-4 tail synapse, the CTLA-4 protein captures its ligands CD80 and CD86 reverses transfer direction. Nectin-1-expressing cells acquire dye- from donor cells by a process of trans-endocytosis; after removal, labeled cytoplasmic proteins synchronously with nectin-4, a process these ligands are degraded inside the acceptor cell, resulting in most active during cell adhesion. -

Analysis of Alternative Splicing Associated with Aging and Neurodegeneration in the Human Brain
Downloaded from genome.cshlp.org on October 2, 2021 - Published by Cold Spring Harbor Laboratory Press Research Analysis of alternative splicing associated with aging and neurodegeneration in the human brain James R. Tollervey,1 Zhen Wang,1 Tibor Hortoba´gyi,2 Joshua T. Witten,1 Kathi Zarnack,3 Melis Kayikci,1 Tyson A. Clark,4 Anthony C. Schweitzer,4 Gregor Rot,5 Tomazˇ Curk,5 Blazˇ Zupan,5 Boris Rogelj,2 Christopher E. Shaw,2 and Jernej Ule1,6 1MRC Laboratory of Molecular Biology, Hills Road, Cambridge CB2 0QH, United Kingdom; 2MRC Centre for Neurodegeneration Research, King’s College London, Institute of Psychiatry, De Crespigny Park, London SE5 8AF, United Kingdom; 3EMBL–European Bioinformatics Institute, Wellcome Trust Genome Campus, Hinxton, Cambridge CB10 1SD, United Kingdom; 4Expression Research, Affymetrix, Inc., Santa Clara, California 95051, USA; 5Faculty of Computer and Information Science, University of Ljubljana, Trzˇasˇka 25, SI-1000 Ljubljana, Slovenia Age is the most important risk factor for neurodegeneration; however, the effects of aging and neurodegeneration on gene expression in the human brain have most often been studied separately. Here, we analyzed changes in transcript levels and alternative splicing in the temporal cortex of individuals of different ages who were cognitively normal, affected by frontotemporal lobar degeneration (FTLD), or affected by Alzheimer’s disease (AD). We identified age-related splicing changes in cognitively normal individuals and found that these were present also in 95% of individuals with FTLD or AD, independent of their age. These changes were consistent with increased polypyrimidine tract binding protein (PTB)– dependent splicing activity. We also identified disease-specific splicing changes that were present in individuals with FTLD or AD, but not in cognitively normal individuals. -

Structural and Functional Analyses of the Interaction of Tetherin with the Dendritic Cell Receptor ILT7 Nicolas Aschman
Structural and functional analyses of the interaction of tetherin with the dendritic cell receptor ILT7 Nicolas Aschman To cite this version: Nicolas Aschman. Structural and functional analyses of the interaction of tetherin with the dendritic cell receptor ILT7. Biomolecules [q-bio.BM]. Université Grenoble Alpes, 2015. English. NNT : 2015GREAV064. tel-01682995 HAL Id: tel-01682995 https://tel.archives-ouvertes.fr/tel-01682995 Submitted on 12 Jan 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. #$ !"#$% '!"(%")!*+%"+% %&'$()*%$*+,(-./$)#.0*%$*2)$-&3+$ ,-.0'*('$."1"34565748*#9:;<9;:=68*89*-=>5?4565748 2!!3$."5'&'6$.!'%("1"7"*8$"9::; !.6% $.%"-*! -4<56=@*A#'BA- <=>6%"+'!').%"-*!"(%"C:"D4>E:48F*D$.##$-&)- -!.-*!.%"* "6%' "+%"( (>49*5E*/4:; *5 9*'866*.>98:=<945> +* 6"6G0<568*%5<95:=68*'(4I48*89*#<48><8 *F;*/4J=>9 A>=6K 8 * 9:;<9;:8668 *89* E5><945>>8668 *F8*6,4>9,:=<945>* F8*6=*9,9(8:4>8*=J8<*68*:,<8N98;: .+. <=>6%"6 $% %"- #('A %5% $"(%*P0*=J:46*P12TB +%C* $"(%"D !E"05-6."+%"1" %:*A>F:8=*'.BA)$++. FG*--!$% !( %:*4J8 *2A(%.- FG*--!$% !( C:*B=:<*5AB.- -

Dynamic Changes in RNA–Protein Interactions and RNA Secondary Structure in Mammalian Erythropoiesis
Published Online: 27 July, 2021 | Supp Info: http://doi.org/10.26508/lsa.202000659 Downloaded from life-science-alliance.org on 30 September, 2021 Resource Dynamic changes in RNA–protein interactions and RNA secondary structure in mammalian erythropoiesis Mengge Shan1,2 , Xinjun Ji3, Kevin Janssen5 , Ian M Silverman3 , Jesse Humenik3, Ben A Garcia5, Stephen A Liebhaber3,4, Brian D Gregory1,2 Two features of eukaryotic RNA molecules that regulate their and RNA secondary structure. These techniques generally either post-transcriptional fates are RNA secondary structure and RNA- use chemical probing agents or structure-specific RNases (single- binding protein (RBP) interaction sites. However, a comprehen- stranded RNases (ssRNases) and double-stranded RNases [dsRNa- sive global overview of the dynamic nature of these sequence ses]) to provide site-specific evidence for a region being in single- or features during erythropoiesis has never been obtained. Here, we double-stranded configurations (4, 5). use our ribonuclease-mediated structure and RBP-binding site To date, the known repertoire of RBP–RNA interaction sites has mapping approach to reveal the global landscape of RNA sec- been built on a protein-by-protein basis, with studies identifying ondary structure and RBP–RNA interaction sites and the dynamics the targets of a single protein of interest, often through the use of of these features during this important developmental process. techniques such as crosslinking and immunoprecipitation se- We identify dynamic patterns of RNA secondary structure and RBP quencing (CLIP-seq) (6). In CLIP-seq, samples are irradiated with UV binding throughout the process and determine a set of corre- to induce the cross-linking of proteins to their RNA targets. -

Large-Scale Analysis of Genome and Transcriptome Alterations in Multiple Tumors Unveils Novel Cancer-Relevant Splicing Networks
Downloaded from genome.cshlp.org on October 2, 2021 - Published by Cold Spring Harbor Laboratory Press Large-scale analysis of genome and transcriptome alterations in multiple tumors unveils novel cancer-relevant splicing networks Endre Sebestyén1,*, Babita Singh1,*, Belén Miñana1,2, Amadís Pagès1, Francesca Mateo3, Miguel Angel Pujana3, Juan Valcárcel1,2,4, Eduardo Eyras1,4,5 1Universitat Pompeu Fabra, Dr. Aiguader 88, E08003 Barcelona, Spain 2Centre for Genomic Regulation, Dr. Aiguader 88, E08003 Barcelona, Spain 3Program Against Cancer Therapeutic Resistance (ProCURE), Catalan Institute of Oncology (ICO), Bellvitge Institute for Biomedical Research (IDIBELL), E08908 L’Hospitalet del Llobregat, Spain. 4Catalan Institution for Research and Advanced Studies, Passeig Lluís Companys 23, E08010 Barcelona, Spain *Equal contribution 5Correspondence to: [email protected] Keywords: alternative splicing, RNA binding proteins, splicing networks, cancer 1 Downloaded from genome.cshlp.org on October 2, 2021 - Published by Cold Spring Harbor Laboratory Press Abstract Alternative splicing is regulated by multiple RNA-binding proteins and influences the expression of most eukaryotic genes. However, the role of this process in human disease, and particularly in cancer, is only starting to be unveiled. We systematically analyzed mutation, copy number and gene expression patterns of 1348 RNA-binding protein (RBP) genes in 11 solid tumor types, together with alternative splicing changes in these tumors and the enrichment of binding motifs in the alternatively spliced sequences. Our comprehensive study reveals widespread alterations in the expression of RBP genes, as well as novel mutations and copy number variations in association with multiple alternative splicing changes in cancer drivers and oncogenic pathways. Remarkably, the altered splicing patterns in several tumor types recapitulate those of undifferentiated cells.