Diving and Hyperbaric Medicine Is for Personal Use Only
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
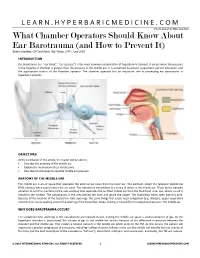
What Chamber Operators Should Know About Ear Barotrauma (And How to Prevent It) Robert Sheffield, CHT and Kevin “Kip” Posey, CHT / June 2018
LEARN.HYPERBARICMEDICINE.COM International ATMO Education What Chamber Operators Should Know About Ear Barotrauma (and How to Prevent It) Robert Sheffield, CHT and Kevin “Kip” Posey, CHT / June 2018 INTRODUCTION Ear barotrauma (i.e. “ear block”, “ear squeeze”) is the most common complication of hyperbaric treatment. It occurs when the pressure in the hyperbaric chamber is greater than the pressure in the middle ear. It is prevented by patient assessment, patient education, and the appropriate actions of the chamber operator. The chamber operator has an important role in preventing ear barotrauma in hyperbaric patients. OBJECTIVES At the conclusion of this article, the reader will be able to: Describe the anatomy of the middle ear Explain the mechanism of ear barotrauma Describe 3 techniques to equalize middle ear pressure ANATOMY OF THE MIDDLE EAR The middle ear is an air space that separates the external ear canal from the inner ear. The eardrum, called the tympanic membrane (TM), vibrates when sound enters the ear canal. The vibration is transmitted to a series of bones in the middle ear. These bones transmit vibration to another membrane (the oval window) that separates the air‐filled middle ear from the fluid‐filled inner ear, where sound is sensed in the cochlea. The nasopharynx is the area behind the nose and above the palate. The Eustachian tubes open into this area. Because of the location of the Eustachian tube openings, the same things that cause nasal congestion (e.g. allergies, upper respiratory infection) can cause swelling around the opening of the Eustachian tubes, making it more difficult to equalize pressure in the middle ear. -

Hypothermia and Respiratory Heat Loss While Scuba Diving
HYPOTHERMIA AND RESPIRATORY HEAT LOSS WHILE SCUBA DIVING Kateřina Kozáková Faculty of Physical Education and Sport, Charles University in Prague, Department of Biomedical Labo- ratory Abstract One of the factors affecting length of stay under water of a diver is heat comfort. During scuba diving there is an increased risk of hypothermia. Hypothermia is one of the most life threatening factors of a diver and significantly affects his performance. The body heat loss runs by different mechanisms. One of them is the respiratory mechanism, which is often overlooked. Compressed dry air or other media is coming out from the cylinder, which have to be heated and humidified to a suitable value. Thus the organism loses body heat and consequently energy. Based on literature search the article will describe safe dive time in terms of hypo- thermia in connection to respiratory heat loss. Key words: hypothermia, heat loss, respiration, scuba diving, water environment Souhrn Jedním z faktorů ovlivňujících délku pobytu potápěče pod vodou je tepelný komfort. Během výkonu přístro- jového potápění hrozí zvýšené riziko hypotermie. Hypotermie představuje jedno z nejzávažnějších ohrožení života potápěče a zásadně ovlivňuje jeho výkon. Ke ztrátám tělesného tepla dochází různými mechanismy. Jednou cestou tepelných ztrát je ztráta tepla dýcháním, která je často opomíjená. Z potápěčského přístroje vychází suchý stlačený vzduch nebo jiné médium, který je třeba při dýchání ohřát a zvlhčit na potřebnou hodnotu. Tím organismus ztrácí tělesné teplo a potažmo energii. Tento článek, na základě literární rešerše, popíše bezpečnou dobou ponoru z hlediska hypotermie a v souvislosti se ztrátou tepla dýcháním. Klíčová slova: hypotermie, ztráta tepla, dýchání, přístrojové potápění, vodní prostředí Introduction amount of body heat. -

Critical Care in the Monoplace Hyperbaric Chamber
Critical Care in the Monoplace Hyperbaric Critical Care - Monoplace Chamber • 30 minutes, so only key points • Highly suggest critical care medicine is involved • Pitfalls Lindell K. Weaver, MD Intermountain Medical Center Murray, Utah, and • Ventilator and IV issues LDS Hospital Salt Lake City, Utah Key points Critical Care in the Monoplace Chamber • Weaver LK. Operational Use and Patient Care in the Monoplace Chamber. In: • Staff must be certified and experienced Resp Care Clinics of N Am-Hyperbaric Medicine, Part I. Moon R, McIntyre N, eds. Philadelphia, W.B. Saunders Company, March, 1999: 51-92 in CCM • Weaver LK. The treatment of critically ill patients with hyperbaric oxygen therapy. In: Brent J, Wallace KL, Burkhart KK, Phillips SD, and Donovan JW, • Proximity to CCM services (ed). Critical care toxicology: diagnosis and management of the critically poisoned patient. Philadelphia: Elsevier Mosby; 2005:181-187. • Must have study patient in chamber • Weaver, LK. Critical care of patients needing hyperbaric oxygen. In: Thom SR and Neuman T, (ed). The physiology and medicine of hyperbaric oxygen therapy. quickly Philadelphia: Saunders/Elsevier, 2008:117-129. • Weaver LK. Management of critically ill patients in the monoplace hyperbaric chamber. In: Whelan HT, Kindwall E., Hyperbaric Medicine Practice, 4th ed.. • CCM equipment North Palm Beach, Florida: Best, Inc. 2017; 65-95. • Without certain modifications, treating • Gossett WA, Rockswold GL, Rockswold SB, Adkinson CD, Bergman TA, Quickel RR. The safe treatment, monitoring and management -

Development of the Crew Dragon ECLSS
ICES-2020-333 Development of the Crew Dragon ECLSS Jason Silverman1, Andrew Irby2, and Theodore Agerton3 Space Exploration Technologies, Hawthorne, California, 90250 SpaceX designed the Crew Dragon spacecraft to be the safest ever flown and to restore the ability of the United States to launch astronauts. One of the key systems required for human flight is the Environmental Control and Life Support System (ECLSS), which was designed to work in concert with the spacesuit and spacecraft. The tight coupling of many subsystems combined with an emphasis on simplicity and fault tolerance created unique challenges and opportunities for the design team. During the development of the crew ECLSS, the Dragon 1 cargo spacecraft flew with a simple ECLSS for animals, providing an opportunity for technology development and the early characterization of system-level behavior. As the ECLSS design matured a series of tests were conducted, including with humans in a prototype capsule in November 2016, the Demo-1 test flight to the ISS in March 2019, and human-in-the-loop ground testing in the Demo-2 capsule in January 2020 before the same vehicle performs a crewed test flight. This paper describes the design and operations of the ECLSS, the development process, and the lessons learned. Nomenclature AC = air conditioning AQM = air quality monitor AVV = active vent valve CCiCap = Commercial Crew Integrated Capability CCtCap = Commercial Crew Transportation Capability CFD = computational fluid dynamics conops = concept of operations COPV = composite overwrapped -

Consensus Conference, the ECHM
24 Diving and Hyperbaric Medicine Volume 47 No. 1 March 2017 Consensus Conference Tenth European Consensus Conference on Hyperbaric Medicine: recommendations for accepted and non-accepted clinical indications and practice of hyperbaric oxygen treatment Daniel Mathieu, Alessandro Marroni and Jacek Kot Abstract (Mathieu D, Marroni A, Kot J. Tenth European Consensus Conference on Hyperbaric Medicine: recommendations for accepted and non-accepted clinical indications and practice of hyperbaric oxygen treatment. Diving and Hyperbaric Medicine. 2017 March;47(1):24-32.) The tenth European Consensus Conference on Hyperbaric Medicine took place in April 2016, attended by a large delegation of experts from Europe and elsewhere. The focus of the meeting was the revision of the European Committee on Hyperbaric Medicine (ECHM) list of accepted indications for hyperbaric oxygen treatment (HBOT), based on a thorough review of the best available research and evidence-based medicine (EBM). For this scope, the modified GRADE system for evidence analysis, together with the DELPHI system for consensus evaluation, were adopted. The indications for HBOT, including those promulgated by the ECHM previously, were analysed by selected experts, based on an extensive review of the literature and of the available EBM studies. The indications were divided as follows: Type 1, where HBOT is strongly indicated as a primary treatment method, as it is supported by sufficiently strong evidence; Type 2, where HBOT is suggested as it is supported by acceptable levels of evidence; Type 3, where HBOT can be considered as a possible/optional measure, but it is not yet supported by sufficiently strong evidence. For each type, three levels of evidence were considered: A, when the number of randomised controlled trials (RCTs) is considered sufficient; B, when there are some RCTs in favour of the indication and there is ample expert consensus; C, when the conditions do not allow for proper RCTs but there is ample and international expert consensus. -

Code of Federal Regulations GPO Access
4±23±97 Wednesday Vol. 62 No. 78 April 23, 1997 Pages 19667±19896 Briefings on how to use the Federal Register For information on briefings in Washington, DC, see announcement on the inside cover of this issue. Now Available Online Code of Federal Regulations via GPO Access (Selected Volumes) Free, easy, online access to selected Code of Federal Regulations (CFR) volumes is now available via GPO Access, a service of the United States Government Printing Office (GPO). CFR titles will be added to GPO Access incrementally throughout calendar years 1996 and 1997 until a complete set is available. GPO is taking steps so that the online and printed versions of the CFR will be released concurrently. The CFR and Federal Register on GPO Access, are the official online editions authorized by the Administrative Committee of the Federal Register. New titles and/or volumes will be added to this online service as they become available. http://www.access.gpo.gov/nara/cfr For additional information on GPO Access products, services and access methods, see page II or contact the GPO Access User Support Team via: ★ Phone: toll-free: 1-888-293-6498 ★ Email: [email protected] federal register 1 II Federal Register / Vol. 62, No. 78 / Wednesday, April 23, 1997 SUBSCRIPTIONS AND COPIES PUBLIC Subscriptions: Paper or fiche 202±512±1800 Assistance with public subscriptions 512±1806 General online information 202±512±1530; 1±888±293±6498 FEDERAL REGISTER Published daily, Monday through Friday, Single copies/back copies: (not published on Saturdays, Sundays, or on official holidays), by the Office of the Federal Register, National Archives and Paper or fiche 512±1800 Records Administration, Washington, DC 20408, under the Federal Assistance with public single copies 512±1803 Register Act (49 Stat. -

Deep Sea Dive Ebook Free Download
DEEP SEA DIVE PDF, EPUB, EBOOK Frank Lampard | 112 pages | 07 Apr 2016 | Hachette Children's Group | 9780349132136 | English | London, United Kingdom Deep Sea Dive PDF Book Zombie Worm. Marrus orthocanna. Deep diving can mean something else in the commercial diving field. They can be found all over the world. Depth at which breathing compressed air exposes the diver to an oxygen partial pressure of 1. Retrieved 31 May Diving medicine. Arthur J. Retrieved 13 March Although commercial and military divers often operate at those depths, or even deeper, they are surface supplied. Minimal visibility is still possible far deeper. The temperature is rising in the ocean and we still don't know what kind of an impact that will have on the many species that exist in the ocean. Guiel Jr. His dive was aborted due to equipment failure. Smithsonian Institution, Washington, DC. Depth limit for a group of 2 to 3 French Level 3 recreational divers, breathing air. Underwater diving to a depth beyond the norm accepted by the associated community. Limpet mine Speargun Hawaiian sling Polespear. Michele Geraci [42]. Diving safety. Retrieved 19 September All of these considerations result in the amount of breathing gas required for deep diving being much greater than for shallow open water diving. King Crab. Atrial septal defect Effects of drugs on fitness to dive Fitness to dive Psychological fitness to dive. The bottom part which has the pilot sphere inside. List of diving environments by type Altitude diving Benign water diving Confined water diving Deep diving Inland diving Inshore diving Muck diving Night diving Open-water diving Black-water diving Blue-water diving Penetration diving Cave diving Ice diving Wreck diving Recreational dive sites Underwater environment. -

Symptomatic Middle Ear and Cranial Sinus Barotraumas As a Complication of Hyperbaric Oxygen Treatment
İst Tıp Fak Derg 2016; 79: 4 KLİNİK ARAŞTIRMA / CLINICAL RESEARCH J Ist Faculty Med 2016; 79: 4 http://dergipark.ulakbim.gov.tr/iuitfd http://www.journals.istanbul.edu.tr/iuitfd SYMPTOMATIC MIDDLE EAR AND CRANIAL SINUS BAROTRAUMAS AS A COMPLICATION OF HYPERBARIC OXYGEN TREATMENT HİPERBARİK OKSİJEN TEDAVİSİ KOMPLİKASYONU: SEMPTOMATİK ORTA KULAK VE KRANYAL SİNUS BAROTRAVMASI Bengüsu MİRASOĞLU*, Aslıcan ÇAKKALKURT*, Maide ÇİMŞİT* ABSTRACT Objective: Hyperbaric oxygen therapy (HBOT) is applied for various diseases. It is generally considered safe but has some benign complications and adverse effects. The most common complication is middle ear barotrauma. The aim of this study was to collect data about middle ear and cranial sinus barotraumas in our department and to evaluate factors affecting the occurrence of barotrauma. Material and methods: Files of patients who had undergone hyperbaric oxygen therapy between June 1st, 2004, and April 30th, 2012, and HBOT log books for the same period were searched for barotraumas. Patients who were intubated and unconscious were excluded. Data about demographics and medical history of conscious patients with barotrauma (BT) were collected and evaluated retrospectively. Results: It was found that over eight years and 23,645 sessions, 39 of a total 896 patients had BT; thus, the general BT incidence of our department was 4.4%. The barotrauma incidence was significantly less in the multiplace chamber (3.1% vs. 8.7%) where a health professional attended the therapies. Most barotraumas were seen during early sessions and were generally mild. A significant accumulation according to treatment indications was not determined. Conclusion: It was thought that the low barotrauma incidence was related to the slow compression rate as well as training patients thoroughly and monitoring them carefully. -
Leonardo User Manual
Direction for use Computer Leonardo ENGLISH cressi.com 2 TABLE OF CONTENTS Main specifications page 4 TIME SET mode: General recommendations Date and time adjustment page 31 and safety measures page 5 SYSTEM mode: Introduction page 10 Setting of measurement unit and reset page 31 1 - COMPUTER CONTROL 3 - WHILE DIVING: COMPUTER Operation of the Leonardo computer page 13 FUNCTIONS 2 - BEFORE DIVING Diving within no decompression limits page 36 DIVE SET mode: DIVE AIR function: Setting of dive parameters page 16 Dive with Air page 37 Oxygen partial pressure (PO2) page 16 DIVE NITROX function: Nitrox - Percentage of the oxygen (FO2) page 18 Dive with Nitrox page 37 Dive Safety Factor (SF) page 22 Before a Nitrox dive page 37 Deep Stop page 22 Diving with Nitrox page 40 Altitude page 23 CNS toxicity display page 40 PLAN mode: PO2 alarm page 43 Dive planning page 27 Ascent rate page 45 GAGE mode: Safety Stop page 45 Depth gauge and timer page 27 Decompression forewarning page 46 Deep Stop page 46 3 Diving outside no decompression limits page 50 5 - CARE AND MAINTENANCE Omitted Decompression stage alarm page 51 Battery replacement page 71 GAGE MODE depth gauge and timer) page 52 6 - TECHNICAL SPECIFICATIONS Use of the computer with 7 - WARRANTY poor visibility page 56 4 - ON SURFACE AFTER DIVING Data display and management page 59 Surface interval page 59 PLAN function - Dive plan page 60 LOG BOOK function - Dive log page 61 HISTORY function - Dive history page 65 DIVE PROFILE function - Dive profile page 65 PCLINK function Pc compatible interface page 66 System Reset Reset of the instrument page 70 4 Congratulations on your purchase of your Leo - trox) dive. -

Thermo Valves Corporation
Thermo Valves Corporation Scuba Diving Valves The Leader in High Pressure Technology Date: 05/31/04 Thermo Scuba Products are Sold Through Authorized Distributors Only Thermo PRO Thermo PRO Modular with H Connector Thermo DIN WWW.THERMOVALVES.COM Page 2 Thermo Valves Corporation Table of Contents Introduction 4 Products and Features 5 Scuba Valve Outlets 6 Breathing Air or EAN? 6 Stand Alone Valves 5251 Thermo K 7 5651 Thermo PRO 8 5262 Thermo DIN 9 5282 Thermo DIN 10 Modular Valves 8043 Thermo Modular 11 8063 Thermo Modular 12 8082 Thermo Modular 13 Modular Valve Attachments 9020 Thermo 230 Bar H Connector 14 9040 Thermo 300 Bar DIN H Connector 15 Manifold Center Bars 16 Exploded View Drawings 5251 Series Exploded View 17 5651, 5262 & 5282 Exploded View 18 8043, 8063 & 8082 Exploded View 19 9020 & 9040 Exploded View 20 8002 CTR W VLV Manifold Center Bar Exploded View 21 Parts Index 22 Scuba Valve Parts Warnings 23 Warnings, Terms and Conditions of Sale 24 Page 3 Thermo Valves Corporation The Leader in High Pressure Technology Who We Are Thermo Valves Corporation was founded in 1972 as a manufacturer of compressed gas cylinder valves and adaptors to a wide variety of international standards. Thermo was acquired in 1988 by Hamai Industries Limited who has been manufacturing cyl- inder valves for over 75 years! Thermo now spe- cializes in specialty gas valves, valves for the semi- conductor industry and scuba diving valves. Thermo’s mission is to supply state of the art equip- ment with a focus on safety and innovation SCUBA Diving Valves With over 75 years of manufacturing experi- ence, Thermo Valves full line includes the Thermo K, Thermo PRO, Thermo DIN and Thermo Modu- lar Series of scuba diving valves. -
Special Operations Rebreathers
Special Operations Underwater Life Support Systems INTRODUCTION TO JFD JFD is the world leading underwater capability provider facilitating the commercial and defence diving industries by offering innovative diving, submarine rescue and subsea technical solutions. JFD has a well-established history in the development of advanced and innovative diving and submarine rescue systems spanning over 30 years. Our systems continue to set the president in terms of capability and performance and JFD is relied upon by divers worldwide across both the defence and commercial sectors. Our products and services have been delivered to a large number of countries across all continents. With in-service support established in many of these locations and tailored Integrated Logistics Support (ILS) packages, JFD is able to provide high customer equipment availability, rapid technical support and tailored training packages. 2 | Introduction JFD offers two highly capable underwater life support systems to meet the full mission profile of today’s Special Operations diver. A modular approach enables customisation of the life support system in response to demands across the full operational spectrum. SHADOW ENFORCER The solution for extended duration and deeper diving The lightweight solution for short duration mission mission profiles. profiles. 3 | Offering A common life support platform facilitates a multi-mission capability offering numerous operational and logistic benefits that include: ENHANCED MISSION EFFECTIVENESS • Front and back mount options • Oxygen -
Hyperbaric Oxygen Therapy (HBOT) Final Evidence Report
20, 2012 Health Technology Assessment Hyperbaric Oxygen Therapy (HBOT) for Tissue Damage, Including Wound Care and Treatment of Central Nervous System (CNS) Conditions Final Evidence Report February 15, 2013 Health Technology Assessment Program (HTA) Washington State Health Care Authority PO Box 42712 Olympia, WA 98504-2712 (360) 725-5126 hta.hca.wa.gov [email protected] Hyperbaric Oxygen Therapy (HBOT) for Tissue Damage, Including Wound Care and Treatment of Central Nervous System (CNS) Conditions A Health Technology Assessment Prepared for Washington State Health Care Authority FINAL REPORT – February 15, 2013 Acknowledgement This report was prepared by: Hayes, Inc. 157 S. Broad Street Suite 200 Lansdale, PA 19446 P: 215.855.0615 F: 215.855.5218 This report is intended to provide research assistance and general information only. It is not intended to be used as the sole basis for determining coverage policy or defining treatment protocols or medical modalities, nor should it be construed as providing medical advice regarding treatment of an individual’s specific case. Any decision regarding claims eligibility or benefits, or acquisition or use of a health technology is solely within the discretion of your organization. Hayes, Inc. assumes no responsibility or liability for such decisions. Hayes employees and contractors do not have material, professional, familial, or financial affiliations that create actual or potential conflicts of interest related to the preparation of this report. Prepared by Winifred Hayes, Inc. Page i February