Epidemiology of Injuries in Ultimate (Frisbee): a Systematic Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

WORLD FLYING DISC FEDERATION (A Colorado Nonprofit Corporation, As Approved by Congress on 1 January 2019)
BYLAWS OF THE WORLD FLYING DISC FEDERATION (a Colorado Nonprofit Corporation, as approved by Congress on 1 January 2019) ARTICLE I - PURPOSES The World Flying Disc Federation (“WFDF”) is organized exclusively for educational purposes and to foster national and international amateur sports competition within the meaning of and pursuant to Section 501(c)(3) of the Internal Revenue Code of 1986, as amended (or under the corresponding provision of any future United States Internal Revenue law). The activities of WFDF include, but are not limited to, such purposes as: 1. To serve as the international governing body of all flying disc sports, with responsibility for sanctioning world championship and other international flying disc events, establishing uniform rules, and setting standards for and recording of world records; 2. To promote and protect the “spirit of the game” and the principle of “self-officiation" as essential aspects of flying disc sports play; 3. To promote flying disc sports play throughout the world and foster the establishment of new national flying disc sports associations, advising them on all flying disc sports activities and general management; 4. To promote and raise public awareness of and lobby for official recognition of flying disc play as sport; 5. To provide an international forum for discussion of all aspects of flying disc sports play; and 6. Consistent with above principles, to transact any and all other lawful business or businesses for which a corporation may be incorporated pursuant to the Colorado Revised Nonprofit Corporation Act, as it may be amended from time to time. ARTICLE II – DEFINITIONS OF DISC SPORTS AND SANCTIONED EVENTS 1. -

Ruog )O\Lqj 'Lvf )Hghudwlrq
:RUOG)O\LQJ'LVF)HGHUDWLRQ 200 Linden • Fort Collins • Colorado 80524 • USA Tel. (970) 484-6932 • Fax (970)490-2714 http://www.wfdf.org *XWV The intent of the game. Guts is one of the team events in the flying disc sports. It is played by two teams of five players each. The official disc of the game is the Pro model Frisbee disc. For informal play, a lightweight, blunt-rim disc such as the 100 G DDC is sometimes used. The playing field consists of two parallel goal-lines 15 m in length and 14 m apart. The teams stand in line opposite each other. Each team defends a goal- line. The disc is thrown back and forth between the teams. The object is to throw the disc through the line of defending players. The throwing team scores a point when the other team does not catch a correctly thrown disc. The receiving team scores a point when the disc is not thrown correctly. When a correctly thrown disc is caught by the other team, no points are scored. The team that first reaches 21 points, wins the game. Tip: if you want you can play with fewer players on a team. Tip: at first you can make the game somewhat easier by suspending the rule that the disc must be caught with one hand. The most important rules. • A game consists of a series of exchanges in which one team throws the disc and the other team attempts to catch the disc. The teams are alternately throwing and receiving: in the next exchange the throwing team becomes the receiving team and vice versa. -

Flying Disc Collector's Association Volume 1 Number 3 $4.00
International Flying Disc Collector's Association Volume 1 Number 3 $4.00 Move over Rover, Purple Pas ion Let Jimmie Flip This Take Over! Free Bird! WK · 930AM Premium Lip erv1• e VOLUME 1, NUMBER 3 From the Director IFDCA is dedicated to promoting flying disc collecting throughout Welcome to the third issue of the International Flying Disc Collector's the world. newsletter We have some really good articles in this issue. One in particular Editorial Offices by Bruce Willis on the Pro Model Frisbee®. Bruce has done years of research IFDCA on this subject and is one of the country's more noteworthy Pro Model collectors. c/o Disc Flights, Inc. In a letter that Bruce wrote to me that carne with his article he noted that there P.O. Box 470794 is some facts that he found that contradict fmdings that were published in Tulsa, OK 74147-0794 Stancil Johnson's book "Frisbee". So keep this in mind when reading Bruce's Membership Rates article. You may even want to update Stancil's book if you have one. $10.00 annually ( 4 issues) In our last two issues we reported on alot of varied discs. In the future we Article Submission will go into more detail on our articles about certain discs. If any of you have or Deadline for next issue- March 12 had a collecting speciality PLEASE contact me by letter or telephone. You, like Bruce, may have information we need to document in our newsletters in Director I Editor Rick Neil the upcoming issues. Assoc. -

University of Washington Bothell Intramural Sports Ultimate Frisbee Rules
University of Washington Bothell Intramural Sports Ultimate Frisbee Rules Introduction: Ultimate is a non-contact disc sport played by two teams of seven players. The objective is to be the team that scores the most goals. A goal is scored when a player catches the disc in the end zone that their team is attacking. Ultimate is a self-officiated sport, it relies on the players to make all calls 1. EQUIPMENT ● Closed toe shoes must be worn. Rubber and molded cleats are permitted. ● Metal cleats are not permitted. ● Players are not allowed to wear headphones or jewelry of any kind. ● Teams must wear shirts or pennies of matching color. ● The Intramural Activities staff will provide a disc unless both teams agree on a different one. ● Participants must wear athletic attire 2. TEAMS ● Teams are made up of a maximum of seven players. ● A team may start the game with five players. ● If a team has more than seven players they may substitute under the following circumstances: After a goal is scored or if a player is injured. 3. TIMING ● The game consists of two 20-minute halves with a 3-minute halftime. ● The clock will only stop for a timeout or injury. ● Each team gets two timeout per half. ● A team may only call timeout if they are in possession of the disc. (Unless it is in- between goals). 4. OVERTIME ● There will be no overtime during regular season games. ● If a playoff game ends in a tie sudden death overtime period (3 minutes) will be played. 5. PULL ● Play starts at the beginning of each half and after each goal with a “pull.” A pull is when a player on the pulling team throws the disc towards the opposite goal line to begin play. -

What Is Rookie Rugby? Fun, Safe Sporting Experience for Both Boys and Girls
Just pick up the ball and run with it! Rookie Rugby is the best way to be active and have fun with a new sport! Whether you are a teacher, former player, long-time supporter, or new to rugby, this game is for you! USA Rugby invites you to find your place in the rugby community - Rookie Rugby can be found in: * Physical Education Classes * After-School Programs * Recreational Leagues * Community Based Programs * State PE Conferences * Your Neighborhood! ‘Rugby For All’ begins with Rookie Rugby! What is Rugby? Game originated when William Webb Ellis picked up the ball and ran with it over 150 years ago in England! Today the game of rugby is played by over 3 million people in 120 countries across 6 continents! A version of rugby called Rugby Sevens has been included in the 2016 Olympic Games in Rio de Janiero, Brazil. Rugby is a team “invasion” game where the object is to get the rugby ball past an opponents’ ‘Try Line’ and ground the ball. What is Rookie Rugby? Fun, safe sporting experience for both boys and girls Simple rules - the game is easy to learn and minimal equipment is required Promotes excellent skill development, teamwork, health, fitness, and most importantly – fun! Rookie Rugby Basics Object of game is to score a ‘try’ by touching the ball to the ground on or behind the goal line. Two hand touch or flags may be used Ball is passed sideways or backward only Free pass is used to start or a restart the game Play is free-flowing and continuous Rookie Rugby can be played in any indoor or outdoor open space Age and ability determines field size and duration of playing time Rookie Rugby is played between two teams of equal size, generally between 5 and 7 players to a team Boys and Girls play by the same rules Game uses ‘tags’ or ‘flags’ so little to no contact is made between players Playing the Game Rookie Rugby Honor Code Supporter/Parent Player 1) Honor the game in action and language. -

923466Magazine1final
www.globalvillagefestival.ca Global Village Festival 2015 Publisher: Silk Road Publishing Founder: Steve Moghadam General Manager: Elly Achack Production Manager: Bahareh Nouri Team: Mike Mahmoudian, Sheri Chahidi, Parviz Achak, Eva Okati, Alexander Fairlie Jennifer Berry, Tony Berry Phone: 416-500-0007 Email: offi[email protected] Web: www.GlobalVillageFestival.ca Front Cover Photo Credit: © Kone | Dreamstime.com - Toronto Skyline At Night Photo Contents 08 Greater Toronto Area 49 Recreation in Toronto 78 Toronto sports 11 History of Toronto 51 Transportation in Toronto 88 List of sports teams in Toronto 16 Municipal government of Toronto 56 Public transportation in Toronto 90 List of museums in Toronto 19 Geography of Toronto 58 Economy of Toronto 92 Hotels in Toronto 22 History of neighbourhoods in Toronto 61 Toronto Purchase 94 List of neighbourhoods in Toronto 26 Demographics of Toronto 62 Public services in Toronto 97 List of Toronto parks 31 Architecture of Toronto 63 Lake Ontario 99 List of shopping malls in Toronto 36 Culture in Toronto 67 York, Upper Canada 42 Tourism in Toronto 71 Sister cities of Toronto 45 Education in Toronto 73 Annual events in Toronto 48 Health in Toronto 74 Media in Toronto 3 www.globalvillagefestival.ca The Hon. Yonah Martin SENATE SÉNAT L’hon Yonah Martin CANADA August 2015 The Senate of Canada Le Sénat du Canada Ottawa, Ontario Ottawa, Ontario K1A 0A4 K1A 0A4 August 8, 2015 Greetings from the Honourable Yonah Martin Greetings from Senator Victor Oh On behalf of the Senate of Canada, sincere greetings to all of the organizers and participants of the I am pleased to extend my warmest greetings to everyone attending the 2015 North York 2015 North York Festival. -
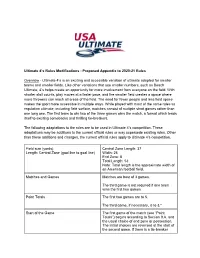
Ultimate 4'S Rules Modifications
Ultimate 4’s Rules Modifications - Proposed Appendix to 2020-21 Rules Overview - Ultimate 4’s is an exciting and accessible variation of ultimate adapted for smaller teams and smaller fields. Like other variations that use smaller numbers, such as Beach Ultimate, 4’s helps create an opportunity for more involvement from everyone on the field. With shorter stall counts, play moves at a faster pace, and the smaller field creates a space where more throwers can reach all areas of the field. The need for fewer people and less field space makes the sport more accessible in multiple ways. While played with most of the same rules as regulation ultimate, including field surface, matches consist of multiple short games rather than one long one. The first team to win two of the three games wins the match, a format which lends itself to exciting comebacks and thrilling tie-breakers. The following adaptations to the rules are to be used in Ultimate 4’s competition. These adaptations may be additions to the current official rules or may supersede existing rules. Other than these additions and changes, the current official rules apply to Ultimate 4’s competition. Field size (yards) Central Zone Length: 37 Length: Central Zone (goal line to goal line) Width: 25 End Zone: 8 Total Length: 53 Note: Total length is the approximate width of an American football field. Matches and Games Matches are best of 3 games. The third game is not required if one team wins the first two games. Point Totals The first two games are to 5. -
Sevens Rugby Implementation Guide
Rugby Canada LTRd SuPPLEMEnTaRy SEVENS RUGBY IMPLEMENTATION GUIDE LTRD: COMMUNITY AND COUNTRY 1 2 LTRD: SEVENS RUGBY IMPLEMENTATION GUIDE Introduction The sevens specific Long Term Rugby Development model implementation guide is an extension of the current LTRD model implemented by Rugby Canada. The aim of the sevens specific model is to inform children, parents, and all other stake holders of the requirements needed to potentially perform in the shortened version of the game. Sevens is now a recognized pathway to national and international competition, with a World Series and Olympic tournament the pinnacle for sevens players. The document has been produced to provide a specific pathway for players wishing to specialize in sevens and give all stakeholders a formal model to follow. The sevens specific model presents a road-map, a developmental check list, for coaches to remedy these traditional shortcomings by training players according to the LTRD outlined by Rugby Canada. A series of itemized tables or “matrices” show expressly which player skills and attributes should be prioritized at each stage of LTRD. Like the full Rugby Canada LTRD the sevens specific pathway is a work in progress and probably always will be. It is based on current knowledge and experience along with available research in areas of physiological testing and human development. LTRD: SEVENS RUGBY IMPLEMENTATION GUIDE 3 A REMINDER OF THE DEFINITIONS OF THE RUGBY CANADA (LTRD) Technical Capacities Knowledge and understanding of rugby specific skills necessary to play the game efficiently. Tactical Capacities Knowledge and understanding of the game and application of its principles to achieve goals. -

World Flying Disc Federation 200 Linden • Fort Collins • Colorado 80524 • USA Tel
World Flying Disc Federation 200 Linden • Fort Collins • Colorado 80524 • USA Tel. (970) 484-6932 • Fax (970)490-2714 http://www.wfdf.org Ultimate in ten rules The intent of the game Ultimate is played with two teams of seven players each and with one disc. The playing field has a size of 100 by 37 m. Indoors it is played on a handball court and then with five players on a team. At both ends of the playing field there is an end zone of 18 m (outdoor) or 6 m (indoor). The throw-off end-line side-line goal-line At the start of the game and after each point scored both teams stand on their goal-line. The team that scored the last point throws the disc. The other team gets disc pos- end-zone 37 m session where the disc lands and becomes the offensive team. Scoring 18 m 64 m 18 m A point is scored when the offensive team catches a disc within the end-zone of the defensive team. The score is valid only when a player of the offensive team threw the disc. In-bounds and out-of-bounds A disc is in-bounds when it is caught inside the playing field. The side-lines and end-lines are out-of- bounds. Also an offensive player must catch the disc inside the end-zone, without touching a line, to score a point. Playing the disc A player in possession of the disc can play it in any direction. He has to do this within ten seconds; a defender will stand before him and count to ten. -

Disc Sports 1984-08
~ ~' ->'.J ·· . DISC WARES UNLIMITED. INC. ' .3:;t St..::·"'cr1t., BULK RATE P.O. BOX 333 U.S. POST AGE AMHERST, MA 01004 PAID Permit No. 10 PH.'FN ~X A1.. Amherst, MA 01004 Forwarding Postage Guaranteed Address Correction Requested Plecue Fonvard If Necessary From the Editor Amid this season of exciting tour league; subcribe to regional newsletters; AMF VOlT INTRODUCES naments, yet more new discs on the teach a disc class in your school or park; market, and more popular recreational support clubs and player organizations; Vol. 2, No.2 disc play, Disc Sport Magazine is seeing invite media personnel to disc events; THE ULTIMATE IN ULTIMATE™ new growth, and strong support from the -sell quality discs, etc. Together, we can disc community. We have plans for con build flying disc sports. Publisher-: tinued expansion and improvements and The new discs on the market are a full Di sc Wares nlimited, Inc. we have new advertising support and line from Ed Headrick, the Phantom new subscribers! With this issue we have from Discraft and the A viar from Innova Editot-: introduced our first four-color page Champion Discs. All are for golf and/or Daryl Elliott which we hope to increase in number in distance. each issue heretofore. We also hope to In closing, I'd like for us to consider expand to 36 or 40 pages and we may the benefits of a national inter ub cription : even move to a glossy format! disciplinary umbrella disc organization. One year: 7.00 To successfully expand DSM, we must It could help with public relations, coor Two year : 12.00 increase our subscription base. -
And Convention
AND CONVENTION EVENT GUIDE $2 www.breakmark.com FACEBOOK.COM/BREAKMARK TWITTER.COM/BREAKMARKULTI Email us at: [email protected] $20 dollar team spot sub tanks just in time for Wildwood. Promo code: wild2015 AND CONVENTION TABLE OF CONTENTS EVENT INFORMATION Welcome from USA Ultimate ............................................................................................ 3 Welcome from Local Organizing Committee .................................................................... 5 Schedule of Events .......................................................................................................7-8 Competition Rules ........................................................................................................... 9 Site Rules ........................................................................................................................ 9 Directions ...................................................................................................................... 10 Convention Session Descriptions .............................................................................11-12 SPECTATOR INFORMATION Information Tent ............................................................................................................ 13 Food at the U.S. Open .................................................................................................... 13 Shooting Photos & Videos.............................................................................................. 13 Men’s Teams.............................................................................................................14-19 -

Ultimate Frisbee Study Sheet
Ultimate Frisbee Study Sheet Ultimate is an exciting, non-contact team sport, played by thousands the world over. It mixes the best features of sports such as Soccer, Basketball, American Football and Netball into an elegantly simple yet fascinating and demanding game. To compete at the top level, Ultimate players require an unmatched degree of speed, stamina and agility . Yet the simplicity of the rules means it's easy and fun for newcomers to pick up. Originating from pie dishes thrown around by American Students, Frisbees have been around most of this century. The sport of Ultimate has its roots in the college campuses of “Sixties America”. The game: A general description Ultimate is played between two teams on a large rectangular pitch. A line drawn across the pitch at either end creates two "end zones" (like in American Football). These are the goal-scoring areas. A goal is scored when a team completes a pass to a player who is in the end zone they are attacking. Players cannot run with the disc . When you get the disc you must come to a stop and try to throw it to another player. By passing from player to player, the offense attempts to work the disc up the pitch towards the end zone they are attacking. If the disc hits the ground or is intercepted or knocked down by the other team, then the opposition takes possession (a change of possession is called a "turnover"). Possession also changes if a receiver is outside the playing area when he or she catches it.