Renal Tubular Acidosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Paroxysmal Nocturnal Hemoglobinuria
Paroxysmal nocturnal hemoglobinuria Description Paroxysmal nocturnal hemoglobinuria is an acquired disorder that leads to the premature death and impaired production of blood cells. The disorder affects red blood cells (erythrocytes), which carry oxygen; white blood cells (leukocytes), which protect the body from infection; and platelets (thrombocytes), which are involved in blood clotting. Paroxysmal nocturnal hemoglobinuria affects both sexes equally, and can occur at any age, although it is most often diagnosed in young adulthood. People with paroxysmal nocturnal hemoglobinuria have sudden, recurring episodes of symptoms (paroxysmal symptoms), which may be triggered by stresses on the body, such as infections or physical exertion. During these episodes, red blood cells are prematurely destroyed (hemolysis). Affected individuals may pass dark-colored urine due to the presence of hemoglobin, the oxygen-carrying protein in blood. The abnormal presence of hemoglobin in the urine is called hemoglobinuria. In many, but not all cases, hemoglobinuria is most noticeable in the morning, upon passing urine that has accumulated in the bladder during the night (nocturnal). The premature destruction of red blood cells results in a deficiency of these cells in the blood (hemolytic anemia), which can cause signs and symptoms such as fatigue, weakness, abnormally pale skin (pallor), shortness of breath, and an increased heart rate. People with paroxysmal nocturnal hemoglobinuria may also be prone to infections due to a deficiency of white blood cells. Abnormal platelets associated with paroxysmal nocturnal hemoglobinuria can cause problems in the blood clotting process. As a result, people with this disorder may experience abnormal blood clotting (thrombosis), especially in large abdominal veins; or, less often, episodes of severe bleeding (hemorrhage). -

The Effect of Flood Diuresis on Hemo-Globinuria
THE EFFECT OF FLOOD DIURESIS ON HEMO- GLOBINURIA. BY HERBERT HAESSLERj M.D. (From the Laboratories of The Rockefeller Inatitute for Medical Research.) (Received for publication, November 9, 1921.) The fact is well recognized that a considerable quantity of hemo- globin must be free in the plasma if any is to pass the renal barrier and appear in the urine. The pigment is, like dextrose, a "threshold substance." It readily penetrates into the renal tubules but is absorbed again more or less completely during its course through them. t This being true, diuresis should diminish the chances of absorption by hastening the flow of fluid, and tend to lead to the appearance of the pigment in the urine. Evidence will here be presented that such is the case. Hemoglobinuria, like glycosuria, is much favored by flood diuresis. Method. A concentrated solution of hemoglobin was abruptly thrown into the circulation of rabbits and dogs, followed in some instances by a slower injection of salt solution. The amount of pigment introduced was slightly less than that required to produce hemoglobinuria in the absence of diuresis. The urine was collected at intervals by catheter. All of the animals were males. Individuals were selected with normal kidneys, as indicated by ~e general character of the urine and proven by the autopsy findings. Great care was necessary to prevent hemorrhage during the catheterization of the rabbits, and despite it a few red cells were frequently encountered after- wards in the urine. For this reason the experiments were repeated on dogs, in which the complication can be avoided. -
Urine Specific Gravity
Please purchase PDFcamp Printer on http://www.verypdf.com/ to remove this watermark. Urine Specific Gravity Urine Specific Gravity (SG) Specific gravity (SG) is a measurement of the kidneys' ability to concentrate urine. The test compares the density of urine against the density of distilled water, which has an SG of 1.000. Because urine is a solution of minerals, salts, and compounds dissolved in water, the SG is a measure of the density of the dissolved chemicals in the specimen. As a measurement of specimen density, SG is influenced by both the number of particles present and the size of the particles. Osmolality is a more exact measurement and may be needed in certain circumstances. Please purchase PDFcamp Printer on http://www.verypdf.com/ to remove this watermark. • The range of urine SG depends on the state of hydration and varies with urine volume and the load of solids to be excreted under standardized conditions; when fluid intake is restricted or increased, SG measures the concentrating and diluting functions of the kidney. Loss of these functions is an indication of renal dysfunction. Please purchase PDFcamp Printer on http://www.verypdf.com/ to remove this watermark. • Reference Values • Normal • 1.005-1.030 (usually between 1.010 and 1.025) • Concentrated urine: 1.025-1.030+ • Dilute urine: 1.001-1.010 • Infant < 2 years old: 1.001-1.018 Please purchase PDFcamp Printer on http://www.verypdf.com/ to remove this watermark. • Procedure • Test SG with the use of a multiple-test dipstick that has a separate reagent area for SG. -
Blood Or Protein in the Urine: How Much of a Work up Is Needed?
Blood or Protein in the Urine: How much of a work up is needed? Diego H. Aviles, M.D. Disclosure • In the past 12 months, I have not had a significant financial interest or other relationship with the manufacturers of the products or providers of the services discussed in my presentation • This presentation will not include discussion of pharmaceuticals or devices that have not been approved by the FDA Screening Urinalysis • Since 2007, the AAP no longer recommends to perform screening urine dipstick • Testing based on risk factors might be a more effective strategy • Many practices continue to order screening urine dipsticks Outline • Hematuria – Definition – Causes – Evaluation • Proteinuria – Definition – Causes – Evaluation • Cases You are about to leave when… • 10 year old female seen for 3 day history URI symptoms and fever. Urine dipstick showed 2+ for blood and no protein. Questions? • What is the etiology for the hematuria? • What kind of evaluation should be pursued? • Is this an indication of a serious renal condition? • When to refer to a Pediatric Nephrologist? Hematuria: Definition • Dipstick > 1+ (large variability) – RBC vs. free Hgb – RBC lysis common • > 5 RBC/hpf in centrifuged urine • Can be – Microscopic – Macroscopic Hematuria: Epidemiology • Microscopic hematuria occurs 4-6% with single urine evaluation • 0.1-0.5% of school children with repeated testing • Gross hematuria occurs in 1/1300 Localization of Hematuria • Kidney – Brown or coke-colored urine – Cellular casts • Lower tract – Terminal gross hematuria – (Blood -

Usefulness of Medi Test Combi 9 in the Diagnosis of Hemoglobinuria in Limited Recourse Setting
Bodi JM, et al. J Nephrol Renal Ther 2021, 7: 044 DOI: 10.24966/NRT-7313/100044 HSOA Journal of Nephrology & Renal Therapy Research Article 10Division of Nephrology, Department of Internal Medicine, University Hos- pitals of Kinshasa, School of Medicine, University of Kinshasa, Democratic Usefulness of Medi Test Republic of Congo Combi 9 in the Diagnosis of Abstract Hemoglobinuria in Limited Background: Detection of hemoglobin in fresh urine remains a challenge in resource limited setting since quantitative measurements Recourse Setting of hemoglobinuria is not always technically feasible. This study aimed to evaluate the performance of 3 types of dipstick for the 1 2 Joseph Mabiala Bodi *, Mamie Ngole , Célestin Ndosimao diagnosis of hemoglobinuria in children suffering Blackwater fever. Nsibu1, Roland Loway Longenge1, Mamygloire Manzi Monkoti1, Thideline Manknga Mabela1, Vicky Niangi Mayifuila1, Michel Methods: In a case-control study, 129 patients (43 inpatients with Ntetani Aloni3, Pierre Zalagile Akilimali4, Pierre Manianga dark urine versus 86 outpatients with clear urine) were screened Tshibassu5, Patrick Kalambayi Kayembe4, Ahmeddin Hassan for hemoglobinuria. A spot urine sample from each subject was Omar6, Kenji Hirayama7, Jan Verhaegen8, Aimé Lumaka9, Pros- tested both with 3 dipsticks (Medi Test Combi 9, as well as 9 per Lukusa Tshilobo9, Ernest Kiswaya Sumaili10 and Nazaire and 10 parameters Cypress) and a spectrophotometer using 3, Mangani Nseka10 3′ dimethylbenzidine reagent. The performance of dipstick was compared and -

Clinical Significance of Biochemical Detection in Urine the Importance Of
Clinical significance of biochemical detection in urine The Importance of Urinalysis for Veterinary use In addition to the external excretion of metabolic products, sick pet urine also contains other pathogens as well as physical particles and cellular components. The physical , biochemical and cellular analysis of pet urine allows a comprehensive pathological assessment for pet various diseases. Due to their special body structure, pets such as cats, dogs etc. are prone to suffer from diseases of the urinary tract, which can endanger the health of pets. Urinalysis testing allows a profound diagnosis of pet diseases such as: • Kidney disease • Liver diseases • Diabetes mellitus • Anemia • Inflammation of urinary tract In addition, periodic physical examination is an important measure to maintain the health of pets, and early regular urine examinations also provides a wide range of comprehensive health information for pets. Ⅰ. Uric acid base reaction Clinical significance: The clinical significance of urine acid-base changes. The change of urine pH will affect the type of crystal formation in urine is as follows: 1. Pathological acid urine is found in animals, such as carnivores, suckling animals, and starved animals. Pathological acid urine is found in fever, acidosis (diabetes, uremia, etc.). Oral acid salts, such as phosphate, ammonium chloride, and sodium chloride, can cause artificial acid urine. 2. Alkaline urine is present in herbivores. Pathologically alkaline urine is present in cystitis, urinary retention (bacterial breakdown of urea into ammonia), and alkalosis. Artificially alkaline urine can be produced by alkaline salts, such as sodium bicarbonate, sodium citrate, and sodium lactate. Ⅱ.Urine protein Clinical meaning: The protein content in the urine increases, the physiology and pathology should be considered when increased protein is seen. -

The Global Genes RARE Foundation Alliance Is Made up of Over 600 Disease Foundations That Have Committed to Collaborating Wi
The Global Genes RARE Foundation Alliance is made up of over 600 disease foundations that have committed to collaborating with Global Genes and other nonprofit foundations in order to create a stronger, collective voice in the rare disease community. #Bold Lips For Sickle Cell – Sickle Cell Disease 11q Research & Resource Group – Jacobsen Syndrome, 11q Chromosome 1p36 Deletion Support & Awareness – 1p36 Deletion Syndrome 22q 11 Ireland support group – 22q11.2 deletion syndrome 4p- Support Group – Wolf-Hirschhorn Syndrome and related 4p conditions 5p-Society– 5p- Syndrome, Cat Cry Syndrome, Cri du Chat Syndrome 17q12 Foundation - 17q12 Deletions and Duplications A Foundation Building Strength for Nemaline Myopathy – Nemaline Myopathy A Nonprofit Group Enriching Lives (ANGEL AID) - Multiple rare diseases Aaron’s Ohtahara – Ohtahara Syndrome Acid Maltase Deficiency Association– Acid Maltase Deficiency, Pompe’s Disease Acromegaly Community – Acromegaly and Gigantism Acromegaly Ottawa Awareness & Support Network - Acromegaly Acoustic Neuroma Association – Acoustic Neuroma ADCY5.org – ADCY5 Mutation Addi & Cassi Fund – Niemann Pick Type C ADNPkids – ADNP Syndrome, Helsmoortal_Van Der AA Syndrome Adrenal Alternatives Foundation - Adrenal Diseases Adrenal Insufficiency United – Adrenal Insufficiency Adult Polyglucosan Body Disease Research Foundation (APBDRF) – APBD Advancing Sickle Cell Advocacy Project, Inc. – Sickle Cell Disease Advocacy & Awareness for Immune Disorders Association – Primary Immunodeficiency Diseases -

Interpretation of Urine Analysis
UNDERSTANDING URINALYSIS Slides __________________________________________________________________________________________________________ Urine Analysis Interpretation of • Appearance or color • Specific gravity • pH Urine Analysis • Leukocyte esterase March 2015 • Nitrites • Urobilinogen • Bilirubin • Glucose • Ketones • Protein • Blood • Microscopic examination Denise K Link, MPAS, PA-C The University of Texas Southwestern Medical Center [email protected] Proper Specimen Collection Routine Urine Analysis Appearance Chemical tests (dipstick) • Teach every patient how to collect proper specimen • pH 1. Clean-catch midstream • Protein 2. In patients with indwelling urinary catheters, a • Glucose recently produced urine sample should be obtained • Ketones (directly from the catheter tubing) • Blood 3. Best examined when fresh. Chemical composition • Urobilinogen of urine changes with standing and formed • Bilirubin elements degenerate with time • Nitrites • Leukocyte esterase 4. Refrigerated is best when infection is suspected • Specific gravity 5. First voided morning urine is ideal when evaluating suspected glomerulonephritis Microscopic examination of spun urinary sediment Urine Analysis with Microscopy Dipstick Methodology • Paper tabs impregnated with chemical reagents • Reagents are chromogenic • Reagents are timed developed • Some rxns are highly specific • Other are sensitive to the presence of interfering substances or extremes of pH • Rapid, semiquantitative assessment of urinary characteristics © 2015 National Kidney Foundation, -

A Discussion of Hemoglobinuria and Hematuria R
Volume 17 | Issue 3 Article 7 1955 A Discussion of Hemoglobinuria and Hematuria R. L. Nelson Iowa State College Follow this and additional works at: https://lib.dr.iastate.edu/iowastate_veterinarian Part of the Large or Food Animal and Equine Medicine Commons, and the Veterinary Pathology and Pathobiology Commons Recommended Citation Nelson, R. L. (1955) "A Discussion of Hemoglobinuria and Hematuria," Iowa State University Veterinarian: Vol. 17 : Iss. 3 , Article 7. Available at: https://lib.dr.iastate.edu/iowastate_veterinarian/vol17/iss3/7 This Article is brought to you for free and open access by the Journals at Iowa State University Digital Repository. It has been accepted for inclusion in Iowa State University Veterinarian by an authorized editor of Iowa State University Digital Repository. For more information, please contact [email protected]. A Discussion of Hemoglobinuria and Helllaturia R. L. Nelson EMOGLOBINURIA MAY BE DE give rise to these symptoms. Some cases EI FINED as the symptom of a patho are of unknown causes. logical state in which the animal passes Etiology of Hematuria and hemoglobin in the urine. In this condition the urine will be pink to brownish-red in Hemoglobinuria color depending upon the amount of hem Bacteria and Viruses oglobin passed. ''Leptospira pomona of bovine *Corynebacterium renale Hematuria is a symptom of that patho *Clostridium hemolyticum logical condition in which the animal pass *Bacillus anthracis es whole blood in the urine. The erythro *Staphylococcus sp. cytes do not hemolyze and the urine will *Streptococcus sp. Proteus ammon,ae appear pink to brownish-red in color de Mycobacterium tuberculosis pending upon the amount of blood passed. -

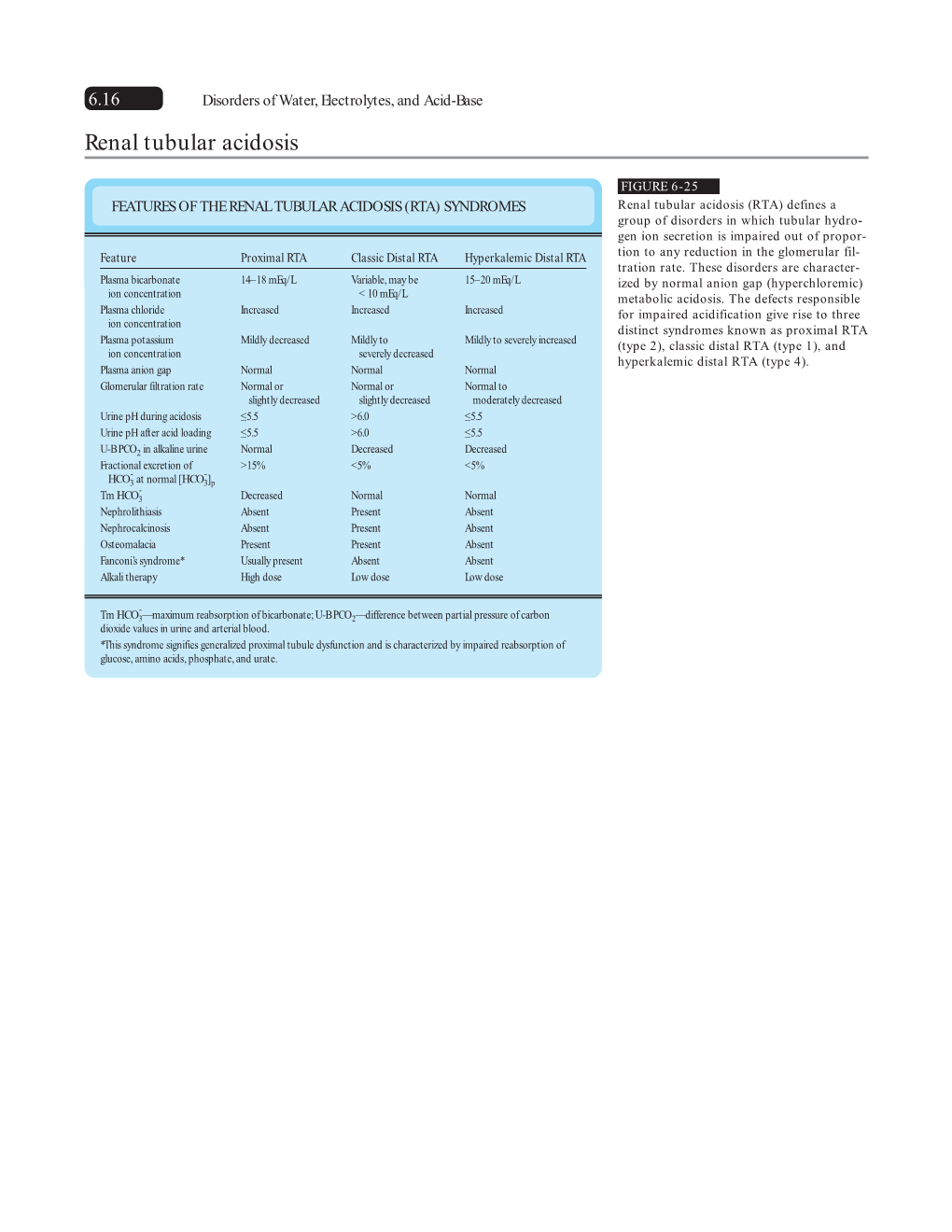
Renal Tubular Acidosis
Clinical DIMENSION Renal Tubular Acidosis Abigail S. Brown, BSN, RN, CCRN Renal tubular acidosis is a relatively uncommon clinical syndrome characterized by the inability of the kidney to adequately excrete hydrogen ions, retain adequate bicarbonate, or both. This syndrome can be categorized into 3 separate disorders, each with unique clinical characteristics. Although an uncommon finding, prompt and inexpensive tests can lead to early intervention and subsequently reduce complications from persistent renal dysfunction. The purpose of this article was to bring awareness of the clinical manifestations, diagnosis, and treatments of renal tubular acidosis to critical care nurses. Keywords: Renal disease, Renal physiology, Renal tubular acidosis [DIMENS CRIT CARE NURS. 2010;29(3):112/119] INTRODUCTION AND BACKGROUND general weakness over the past month. Examination results Renal tubular acidosis (RTA) is a relatively uncommon were relatively benign aside from general, diffuse muscle clinical syndrome characterized by the inability of the kidney weakness, dry buccal mucosa, and dry eyes. Her medical to adequately excrete hydrogen ions, retain adequate and surgical history were unremarkable except for an bicarbonate, or both.1,2 First illustrated in 1935, this approximate 6-month history of dry eyes that which was syndrome was further delineated as RTA in 1951.2 Renal unrelieved by over-the-counter eye drops. Her current tubular acidosis syndrome is manifested in the presence of a medications were only over-the-counter eye drops (artifi- relatively normal glomerular filtration rate, normal plasma cial tears). She denied any known allergies to medications anion gap, and a hyperchloremic metabolic acidosis.2-4 and denied the use of alcohol or tobacco products. -

Urine Dipstick Testing: Everything You Need to Know
INFOCUS Urine Dipstick Testing: Everything You Need to Know BY JAMES R. ROBERTS, MD The latter function is disrupted in a variety of diseases. hink of all the times you order The normal USG ranges from Turinalysis each shift. It seems 1.003 to 1.030. USG less than 1.010 to be a straightforward test, and is suggestive of relative hydration, most physicians think they are and values greater than 1.020 in- well versed in the interpretation dicate relative dehydration. Patho- of the results: You give it a glance logic conditions that increase the and make a decision. The dipstick USG without regard to hydration analysis, the microscopic exam, included glycosuria and syndrome and other information gleaned of inappropriate antidiuretic from a UA make their way into hormone secretion (SIADH). decision-making for a variety of Osmolality is the more important diagnostic, therapeutic, and dis- parameter to measure in such position issues. Like most things cases. A decreased USG, also learned in detail many years known as dilute urine, is associated ago, the interpretation of the UA with diuretic use, diabetes insip- should be revisited on a regular idus, adrenal insufficiency, aldoster- basis. onism, or a plethora of conditions I find myself thinking I know James R. Roberts, MD causing impaired renal function. Clear urine with a dipstick strongly positive for blood usually means everything about a certain test It should be noted that the myoglobinuria. In such cases, the microscopic analysis would be negative only to find that the guidelines for RBCs. Significant myoglobinuria can produce acute renal failure. -

OPTN Policies Effective As of July 27 2021
Policies Contents Policy 1: Administrative Rules and Definitions 1 Policy 2: Deceased Donor Organ Procurement 21 Policy 3: Candidate Registrations, Modifications, and Removals 36 Policy 4: Histocompatibility 47 Policy 5: Organ Offers, Acceptance, and Verification 78 Policy 6: Allocation of Hearts and Heart-Lungs 90 Policy 7: Allocation of Intestines 127 Policy 8: Allocation of Kidneys 129 Policy 9: Allocation of Livers and Liver-Intestines 158 Policy 10: Allocation of Lungs 213 Policy 11: Allocation of Pancreas, Kidney-Pancreas, and Islets 244 Policy 12: Allocation of Vascularized Composite Allografts (VCA) 254 Policy 13: Kidney Paired Donation (KPD) 255 Policy 14: Living Donation 272 Policy 15: Identification of Transmissible Diseases 295 Policy 16: Organ and Extra Vessel Packaging, Labeling, Shipping, and Storage 304 Policy 17: International Organ Transplantation 312 Policy 18 Data Submission Requirements 315 Policy 19: Data Release 325 Policy 20: Travel Expense and Reimbursement 325 Organ Procurement and Transplantation Network (OPTN) Policies Policy 1: Administrative Rules and Definitions 1.1 Rules of Construction 1 1.2 Definitions 1 1.3 Variances 17 1.4 Allocation of Organs during Emergencies 19 1.5 Department of Defense Directive 20 1.1 Rules of Construction The rules and definitions set forth in this Policy apply to all OPTN Policies. 1.1.A Time A day ends at midnight Eastern Standard Time (EST). 1.1.B Headings, Notes, and History All headings, notes, and history sections of these Policies, are intended only as guidance and to supplement the OPTN Policies and are not part of the Policies. These sections and headings are nonbinding to members and should not be treated as policy or used to infer the intent of the Policies.