Interpretation of Urine Analysis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hyperbilirubinemia
Porphyrins Porphyrins (Porphins) are cyclic tetrapyrol compounds formed by the linkage )). of four pyrrole rings through methenyl bridges (( HC In the reduced porphyrins (Porphyrinogens) the linkage of four pyrrole rings (tetrapyrol) through methylene bridges (( CH2 )) The characteristic property of porphyrins is the formation of complexes with the metal ion bound to nitrogen atoms of the pyrrole rings. e.g. Heme (iron porphyrin). Proteins which contain heme ((hemoproteins)) are widely distributed e.g. Hemoglobin, Myoglobin, Cytochromes, Catalase & Tryptophan pyrrolase. Natural porphyrins have substituent side chains on the eight hydrogen atoms numbered on the pyrrole rings. These side chains are: CH 1-Methyl-group (M)… (( 3 )) 2-Acetate-group (A)… (( CH2COOH )) 3-Propionate-group (P)… (( CH2CH2COOH )) 4-Vinyl-group (V)… (( CH CH2 )) Porphyrins with asymmetric arrangement of the side chains are classified as type III porphyrins while those with symmetric arrangement of the side chains are classified as type I porphyrins. Only types I & III are present in nature & type III series is more important because it includes heme. 1 Heme Biosynthesis Heme biosynthesis occurs through the following steps: 1-The starting reaction is the condensation between succinyl-CoA ((derived from citric acid cycle in the mitochondria)) & glycine, this reaction is a rate limiting reaction in the hepatic heme synthesis, it occurs in the mitochondria & is catalyzed by ALA synthase (Aminolevulinate synthase) enzyme in the presence of pyridoxal phosphate as a cofactor. The product of this reaction is α-amino-β-ketoadipate which is rapidly decarboxylated to form δ-aminolevulinate (ALA). 2-In the cytoplasm condensation reaction between two molecules of ALA is catalyzed by ALA dehydratase enzyme to form two molecules of water & one 2 molecule of porphobilinogen (PBG) which is a precursor of pyrrole. -

Leukocyte Esterase Activity in Vaginal Fluid of Pregnant and Non-Pregnant Women with Vaginitis/Vaginosis and in Controls
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by PubMed Central Infect Dis Obstet Gynecol 2003;11:19–26 Leukocyte esterase activity in vaginal fluid of pregnant and non-pregnant women with vaginitis/vaginosis and in controls Per-Anders Mårdh 1, Natalia Novikova 1, Ola Niklasson 1, Zoltan Bekassy 1 and Lennart Skude 2 1Department of Obstetrics and Gynecology, University Hospital, Lund and 2Department of Clinical Chemistry, County Hospital, Halmstad, Sweden Objectives: Todeterminethe leukocyteesterase (LE) activity invaginal lavage fluid ofwomen with acuteand recurrentvulvovaginal candidosis (VVC and RVVC respectively), bacterial vaginosis(BV), and in pregnant and non-pregnantwomen without evidenceof the threeconditions. Also tocompare the resultof LEtestsin women consultingat differentweeks inthe cycle andtrimesters of pregnancy.The LEactivity was correlatedto vaginal pH, numberof inflammatory cells instained vaginal smears,type of predominatingvaginal bacteria andpresence of yeast morphotypes. Methods: Onehundred and thirteen women with ahistoryof RVVC,i.e. with at least fourattacks of the conditionduring the previousyear and who had consultedwith anassumed new attack ofthe condition,were studied.Furthermore, we studied16 women with VVC,15 women with BV,and 27 women attendingfor control of cytological abnormalities, who all presentedwithout evidenceof either vaginitisor vaginosis. Finally, 73 pregnantwomen wereinvestigated. The LEactivity invaginal fluid duringdifferent weeks inthe cycle of 53 of the women was measured. Results: Inthe non-pregnantwomen, anincreased LE activity was foundin 96, 88, 73 and56% of those with RVVC,VVC and BV andin the non-VVC/BVcases,respectively. In 73% of pregnantwomen inthe second trimester,and 76% of thosein the third,the LEtestwas positive.In all groupsof non-pregnantwomen tested, the LEactivity correlatedwith the numberof leukocytesin vaginal smears,but it didnot in those who were pregnant.There was nocorrelation between LE activity andweek incycle. -

Porphyrins & Bile Pigments
Bio. 2. ASPU. Lectu.6. Prof. Dr. F. ALQuobaili Porphyrins & Bile Pigments • Biomedical Importance These topics are closely related, because heme is synthesized from porphyrins and iron, and the products of degradation of heme are the bile pigments and iron. Knowledge of the biochemistry of the porphyrins and of heme is basic to understanding the varied functions of hemoproteins in the body. The porphyrias are a group of diseases caused by abnormalities in the pathway of biosynthesis of the various porphyrins. A much more prevalent clinical condition is jaundice, due to elevation of bilirubin in the plasma, due to overproduction of bilirubin or to failure of its excretion and is seen in numerous diseases ranging from hemolytic anemias to viral hepatitis and to cancer of the pancreas. • Metalloporphyrins & Hemoproteins Are Important in Nature Porphyrins are cyclic compounds formed by the linkage of four pyrrole rings through methyne (==HC—) bridges. A characteristic property of the porphyrins is the formation of complexes with metal ions bound to the nitrogen atom of the pyrrole rings. Examples are the iron porphyrins such as heme of hemoglobin and the magnesium‐containing porphyrin chlorophyll, the photosynthetic pigment of plants. • Natural Porphyrins Have Substituent Side Chains on the Porphin Nucleus The porphyrins found in nature are compounds in which various side chains are substituted for the eight hydrogen atoms numbered in the porphyrin nucleus. As a simple means of showing these substitutions, Fischer proposed a shorthand formula in which the methyne bridges are omitted and a porphyrin with this type of asymmetric substitution is classified as a type III porphyrin. -

Surgeons, Columbia University, New York City) (Received for Publication August 9, 1932)
THE ADDIS SEDIMENT COUNT IN NORMAL CHILDREN By JOHN D. LYTTLE (From the Babies Hospit and the Department of Pediatrics, Colege of Physicians and Surgeons, Columbia University, New York City) (Received for publication August 9, 1932) THE METHOD In 1925 Addis (1) described a method by which, in a concentrated acid urine, the rate of excretion of protein, casts and red and white cells could be determined. His method, with certain modifications, has been followed here. All of the counts were made on the 12 hour night specimen from 7 or 8 P.M. to 7 or 8 A.M. Addis recommended that fluids be restricted during, and for 12 hours preceding the collection, since in dilute and alkaline urine hyaline casts dissolve and red cells may be completely lysed. With children this rigid restriction of fluid proved impossible. Withholding fluid during the afternoon and night except for 200 cc. at the evening meal, gave urines of such concentration and acidity that they were suitable for a count. Most children had an early supper and col- lections were started at 7 or 8 P.M. Under these conditions, the urinary pH was between 5.0 and 6.0 and the specific gravity usually well above 1.020. The specimens were treated as described by Addis: "the con- centrated night urine is thoroughly mixed by repeated inversion of the rubber-stoppered bottle and a 10 cc. sample is transferred to a special graduated tube, and centrifugalized for five minutes at 1,800 revolutions per minute. The supernatant urine is decanted and pipetted down to a known volume which varies with the amount of sediment as judged by direct observation. -

Ileal Neobladder: an Important Cause of Non-Anion Gap Metabolic Acidosis
The Journal of Emergency Medicine, Vol. 52, No. 5, pp. e179–e182, 2017 Ó 2017 Elsevier Inc. All rights reserved. 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2016.12.036 Clinical Communications: Adult ILEAL NEOBLADDER: AN IMPORTANT CAUSE OF NON-ANION GAP METABOLIC ACIDOSIS Jesse W. St. Clair, MD and Matthew L. Wong, MD, MPH Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Boston, Massachusetts and Department of Emergency Medicine, Harvard Medical School, Boston, Massachusetts Reprint Address: Matthew L. Wong, MD, MPH, Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Rosenberg Building, 2nd Floor, 1 Deaconess Road, Boston, MA 02446 , Abstract—Background: The differential diagnosis for a disease, or medications such as acetazolamide. non-anion gap metabolic acidosis is probably less well Commonly used mnemonics to remember the differential known than the differential diagnosis for an anion gap for the non-anion gap metabolic acidosis include metabolic acidosis. One etiology of a non-anion gap acidosis ‘‘ABCD’’ for ‘‘Addison’s, Bicarbonate loss, Chloride is the consequence of ileal neobladder urinary diversion (administration), and Drugs,’’ as well as ‘‘HARDUP’’ for the treatment of bladder cancer. Case Report: We pre- for ‘‘Hyperchloremia, Acetazolamide and Addison’s, sent a case of a patient with an ileal neobladder with a severe non-anion gap metabolic acidosis caused by a Renal Tubular Acidosis, Diarrhea, Ureteroenterostomies, urinary tract infection and ureteroenterostomy. Why and Pancreaticoenterostomies’’ (Table 1) (1). Should an Emergency Physician Be Aware of This?: Part Ureteroenterostomies are when the ureter has an of the ileal neobladder surgery includes ureteroenteros- abnormal connection with a segment of intestine. -
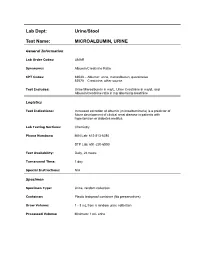
Lab Dept: Urine/Stool Test Name: MICROALBUMIN, URINE
Lab Dept: Urine/Stool Test Name: MICROALBUMIN, URINE General Information Lab Order Codes: UMAR Synonyms: Albumin/Creatinine Ratio CPT Codes: 82043 – Albumin: urine, microalbumin, quantitative 82570 – Creatinine; other source Test Includes: Urine Microalbumin in mg/L, Urine Creatinine in mg/dL and Albumin/creatinine ratio in mg albumin/g creatinine Logistics Test Indications: Increased excretion of albumin (microalbuminuria) is a predictor of future development of clinical renal disease in patients with hypertension or diabetes mellitus. Lab Testing Sections: Chemistry Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours Turnaround Time: 1 day Special Instructions: N/A Specimen Specimen Type: Urine, random collection Container: Plastic leakproof container (No preservatives) Draw Volume: 1 - 3 mL from a random urine collection Processed Volume: Minimum: 1 mL urine Collection: A random urine sample may be obtained by voiding into a urine cup and is often performed at the laboratory. Bring the refrigerated container to the lab. Make sure all specimens submitted to the laboratory are properly labeled with the patient’s name, medical record number and date of birth. Special Processing: Lab Staff: Centrifuge specimen before analysis. Patient Preparation: Sample should not be collected after exertion, in the presence of a urinary tract infection, during acute illness, immediately after surgery, or after acute fluid load. Sample Rejection: Mislabled or unlabeled specimens; samples contaminated with blood Interpretive Reference Range: Albumin/creatinine ratio (A/C <30 mg/g Normal ratio) 30 - 299 mg/g Microalbuminuria >300 mg/g Clinical albuminuria Urine Creatinine: No reference ranges established Critical Values: N/A Limitations: Due to variability in urinary albumin excretion, at least two of three test results measured within a 6-month period should show elevated levels before a patient is designated as having microalbuminuria. -

Interpretation of Canine and Feline Urinalysis
$50. 00 Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Preface Urine is that golden body fluid that has the potential to reveal the answers to many of the body’s mysteries. As Thomas McCrae (1870-1935) said, “More is missed by not looking than not knowing.” And so, the authors would like to dedicate this handbook to three pioneers of veterinary nephrology and urology who emphasized the importance of “looking,” that is, the importance of conducting routine urinalysis in the diagnosis and treatment of diseases of dogs and cats. To Dr. Carl A. Osborne , for his tireless campaign to convince veterinarians of the importance of routine urinalysis; to Dr. Richard C. Scott , for his emphasis on evaluation of fresh urine sediments; and to Dr. Gerald V. Ling for his advancement of the technique of cystocentesis. Published by The Gloyd Group, Inc. Wilmington, Delaware © 2004 by Nestlé Purina PetCare Company. All rights reserved. Printed in the United States of America. Nestlé Purina PetCare Company: Checkerboard Square, Saint Louis, Missouri, 63188 First printing, 1998. Laboratory slides reproduced by permission of Dennis J. Chew, DVM and Stephen P. DiBartola, DVM. This book is protected by copyright. ISBN 0-9678005-2-8 Table of Contents Introduction ............................................1 Part I Chapter 1 Sample Collection ...............................................5 -

A Dipstick Test Combined with Urine Specific Gravity Improved the Accuracy of Proteinuria Determination in Pregnancy Screening
Kobe J. Med. Sci., Vol. 56, No. 4, pp. E165-E172, 2010 A Dipstick Test Combined with Urine Specific Gravity Improved the Accuracy of Proteinuria Determination in Pregnancy Screening NATSUKO MAKIHARA1, MINEO YAMASAKI1,2, HIROKI MORITA1, and HIDETO YAMADA1* 1Division of Obstetrics and Gynecology, Department of Surgery-related, and 2Division of Integrated Medical Education, Department of Community Medicine and Social Healthcare Science, Kobe University Graduate School of Medicine, 7-5-1 Kusunoki-cho, Chuo-ku, Kobe, 650-0017, Japan. Received 12 July 2010/ Accepted 20 August 2010 Key Words: dipstick test, pregnancy proteinuria, protein/creatinine ratio, urine specific gravity Proteinuria screening using a semi-quantitative dipstick test of the spot urine in antenatal clinic is known to have high false-positive rates. The aim of this study was to assess availability of a dipstick test combined with the urine specific gravity for the determination of pathological proteinuria. A dipstick test was performed on 582 urine samples obtained from 283 pregnant women comprising 260 with normal blood pressure and 23 with pregnancy-induced hypertension. The urine protein (P) and creatinine (C) concentrations, specific gravity (SG), P/C ratio were determined, and compared with dipstick test results. The P concentration increased along the stepwise augmentations in dipstick test result. Frequencies of the urine samples with 0.265 or more P/C ratio were 0.7% with − dipstick test result, 0.7% with the ± result, 3.3% with the 1+ result, and 88.9% with the ≥2+ result. However, if the urine specific gravity was low, frequencies of the high P/C ratio were 5.0% with ± dipstick test result and 9.3% with the 1+ result. -

Paroxysmal Nocturnal Hemoglobinuria
Paroxysmal nocturnal hemoglobinuria Description Paroxysmal nocturnal hemoglobinuria is an acquired disorder that leads to the premature death and impaired production of blood cells. The disorder affects red blood cells (erythrocytes), which carry oxygen; white blood cells (leukocytes), which protect the body from infection; and platelets (thrombocytes), which are involved in blood clotting. Paroxysmal nocturnal hemoglobinuria affects both sexes equally, and can occur at any age, although it is most often diagnosed in young adulthood. People with paroxysmal nocturnal hemoglobinuria have sudden, recurring episodes of symptoms (paroxysmal symptoms), which may be triggered by stresses on the body, such as infections or physical exertion. During these episodes, red blood cells are prematurely destroyed (hemolysis). Affected individuals may pass dark-colored urine due to the presence of hemoglobin, the oxygen-carrying protein in blood. The abnormal presence of hemoglobin in the urine is called hemoglobinuria. In many, but not all cases, hemoglobinuria is most noticeable in the morning, upon passing urine that has accumulated in the bladder during the night (nocturnal). The premature destruction of red blood cells results in a deficiency of these cells in the blood (hemolytic anemia), which can cause signs and symptoms such as fatigue, weakness, abnormally pale skin (pallor), shortness of breath, and an increased heart rate. People with paroxysmal nocturnal hemoglobinuria may also be prone to infections due to a deficiency of white blood cells. Abnormal platelets associated with paroxysmal nocturnal hemoglobinuria can cause problems in the blood clotting process. As a result, people with this disorder may experience abnormal blood clotting (thrombosis), especially in large abdominal veins; or, less often, episodes of severe bleeding (hemorrhage). -

The Effect of Flood Diuresis on Hemo-Globinuria
THE EFFECT OF FLOOD DIURESIS ON HEMO- GLOBINURIA. BY HERBERT HAESSLERj M.D. (From the Laboratories of The Rockefeller Inatitute for Medical Research.) (Received for publication, November 9, 1921.) The fact is well recognized that a considerable quantity of hemo- globin must be free in the plasma if any is to pass the renal barrier and appear in the urine. The pigment is, like dextrose, a "threshold substance." It readily penetrates into the renal tubules but is absorbed again more or less completely during its course through them. t This being true, diuresis should diminish the chances of absorption by hastening the flow of fluid, and tend to lead to the appearance of the pigment in the urine. Evidence will here be presented that such is the case. Hemoglobinuria, like glycosuria, is much favored by flood diuresis. Method. A concentrated solution of hemoglobin was abruptly thrown into the circulation of rabbits and dogs, followed in some instances by a slower injection of salt solution. The amount of pigment introduced was slightly less than that required to produce hemoglobinuria in the absence of diuresis. The urine was collected at intervals by catheter. All of the animals were males. Individuals were selected with normal kidneys, as indicated by ~e general character of the urine and proven by the autopsy findings. Great care was necessary to prevent hemorrhage during the catheterization of the rabbits, and despite it a few red cells were frequently encountered after- wards in the urine. For this reason the experiments were repeated on dogs, in which the complication can be avoided. -

Albuminuria Versus Egfr
Albuminuria versus GFR as markers of diabetic CKD progression KDIGO Controversies Conference: “Diabetic Kidney Disease” New Delhi, March 2012 Richard J MacIsaac PhD FRACP Director of Endocrinology & Diabetes, St Vincent's Hospital Professorial Fellow, University of Melbourne Evolution of Diabetic CKD Incipient Overt Nephropathy Nephropathy GFR 100 Log AER (ml/min) GFR 10 15 20 yrs Normoalbuminuria Microalbuminuria Macroalbuminuria (AER < 20 µµµg/min) (AER 20-200 µµµg/min) (AER > 200 µµµg/min) Stages of CKD Stage eGFR Description Predominant (ml/min/1.73 m2) AER status 1 > 90 Kidney damage with normal/high GFR Normo- Micro- 2 60-89 Kidney damage with mild reduction in GFR Micro- 3 30-59 Kidney damage with moderate reduction in Micro/Macro- GFR 4 15-29 Kidney damage with severe reduction in Macro- GFR 5 < 15 Kidney failure Albuminuria versus GFR as markers of diabetic CKD progression 1. Albuminuria as a predictor of diabetic CKD 2. GFR as a predictor of diabetic CKD 3. Albuminuria & GFR uncoupling/coupling 4. Summary Albuminuria as a marker of diabetic CKD progression • High Variability M N • Low Specificity • Spontaneous Regression µ • Δ AER ≠ Δ GFR Higher levels of urinary albumin excretion within the normal range predict faster decline in glomerular filtration rate in diabetic patients Babazono T et al. Diabetes Care 2009;32:1518-1520 Albuminuria versus GFR as markers of diabetic CKD progression 1. Albuminuria as a predictor of diabetic CKD 2. GFR as a predictor of diabetic CKD 3. ALbuminuria & GFR uncoupling/coupling 4. Summary GFR as -

Prevalence of Microalbuminuria and Associated Risk Factors Among Adult Korean Hypertensive Patients in a Primary Care Setting
Hypertension Research (2013) 36, 807–823 & 2013 The Japanese Society of Hypertension All rights reserved 0916-9636/13 www.nature.com/hr ORIGINAL ARTICLE Prevalence of microalbuminuria and associated risk factors among adult Korean hypertensive patients in a primary care setting Yon Su Kim 1, Han Soo Kim2, Ha Young Oh3, Moon-Kyu Lee4, Cheol Ho Kim5, Yong Soo Kim6,DavidWu6, Amy O Johnson-Levonas6 and Byung-Hee Oh7 Microalbuminuria is an early sign of nephropathy and an independent predictor of end-stage renal disease. The purpose of this study was to assess microalbuminuria prevalence and its contributing factors in Korean hypertensive patients. This cross-sectional study enrolled male and female patients of X35 years old with an essential hypertension diagnosis as made by 841 physicians in primary care clinics and 17 in general hospitals in the Republic of Korea between November 2008 and July 2009. To assess microalbuminuria prevalence, urine albumin/creatinine ratio (UACR) was measured in patients with a positive dipstick test. Of the 40 473 enrolled patients, 5713 (14.1%) had a positive dipstick test. Of 5393 patients with a positive dipstick test and valid UACR values, 2657 (6.6%) had significantly elevated UACR (X30 lgmgÀ1), 2158 (5.4%) had microalbuminuria (30 lgmgÀ1pUACR o300 lgmgÀ1) and 499 (1.2%) had macroalbuminuria (UACR X300 lgmgÀ1). Based on multivariate analysis, independent factors associated with elevated UACR included low adherence to antihypertensive medication (23% higher; P ¼ 0.042), poorly controlled blood pressure (BP; 38% higher for systolic BP/diastolic BP X130 mm Hg/X80 mm Hg; Po0.001), obesity (47% higher for body mass index (BMI) X25.0 kg m À2; Po0.001), age (17% lower and 58% higher for age categories 35–44 years (P ¼ 0.043) and 475 years (Po0.001), respectively) and a prior history of diabetes (151% higher; Po0.001) and kidney-related disease (71% higher; Po0.001).