Urine Dipstick Testing: Everything You Need to Know
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
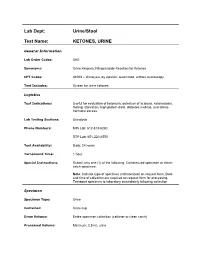
Ketones, Urine
Lab Dept: Urine/Stool Test Name: KETONES, URINE General Information Lab Order Codes: UKE Synonyms: Urine Ketones; Nitroprusside Reaction for Ketones CPT Codes: 81003 – Urinalysis, by dipstick; automated, without microscopy Test Includes: Screen for urine ketones. Logistics Test Indications: Useful for evaluation of ketonuria, detection of acidosis, ketoacidosis, fasting, starvation, high protein diets, diabetes mellitus, and stress- hormone excess. Lab Testing Sections: Urinalysis Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours Turnaround Time: 1 hour Special Instructions: Submit only one (1) of the following: Catheterized specimen or clean- catch specimen. Note: Indicate type of specimen (catheterized) on request form. Date and time of collection are required on request form for processing. Transport specimen to laboratory immediately following collection Specimen Specimen Type: Urine Container: Urine cup Draw Volume: Entire specimen collection (catheter or clean catch) Processed Volume: Minimum: 0.5 mL urine Collection: A specimen collected by catheterization is optimal; however, a clean- catch or mid-stream specimen is also acceptable. Random, voided specimens will be accepted, but are the least desirable and are not recommended if a urine culture is also being requested. Special Processing: N/A Patient Preparation: None Sample Rejection: Less than 0.5 mL urine submitted; mislabeled or unlabeled specimen Interpretive Reference Range: Negative Critical Values: N/A Limitations: Specimens containing -

Leukocyte Esterase Activity in Vaginal Fluid of Pregnant and Non-Pregnant Women with Vaginitis/Vaginosis and in Controls
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by PubMed Central Infect Dis Obstet Gynecol 2003;11:19–26 Leukocyte esterase activity in vaginal fluid of pregnant and non-pregnant women with vaginitis/vaginosis and in controls Per-Anders Mårdh 1, Natalia Novikova 1, Ola Niklasson 1, Zoltan Bekassy 1 and Lennart Skude 2 1Department of Obstetrics and Gynecology, University Hospital, Lund and 2Department of Clinical Chemistry, County Hospital, Halmstad, Sweden Objectives: Todeterminethe leukocyteesterase (LE) activity invaginal lavage fluid ofwomen with acuteand recurrentvulvovaginal candidosis (VVC and RVVC respectively), bacterial vaginosis(BV), and in pregnant and non-pregnantwomen without evidenceof the threeconditions. Also tocompare the resultof LEtestsin women consultingat differentweeks inthe cycle andtrimesters of pregnancy.The LEactivity was correlatedto vaginal pH, numberof inflammatory cells instained vaginal smears,type of predominatingvaginal bacteria andpresence of yeast morphotypes. Methods: Onehundred and thirteen women with ahistoryof RVVC,i.e. with at least fourattacks of the conditionduring the previousyear and who had consultedwith anassumed new attack ofthe condition,were studied.Furthermore, we studied16 women with VVC,15 women with BV,and 27 women attendingfor control of cytological abnormalities, who all presentedwithout evidenceof either vaginitisor vaginosis. Finally, 73 pregnantwomen wereinvestigated. The LEactivity invaginal fluid duringdifferent weeks inthe cycle of 53 of the women was measured. Results: Inthe non-pregnantwomen, anincreased LE activity was foundin 96, 88, 73 and56% of those with RVVC,VVC and BV andin the non-VVC/BVcases,respectively. In 73% of pregnantwomen inthe second trimester,and 76% of thosein the third,the LEtestwas positive.In all groupsof non-pregnantwomen tested, the LEactivity correlatedwith the numberof leukocytesin vaginal smears,but it didnot in those who were pregnant.There was nocorrelation between LE activity andweek incycle. -

Different Response of Body Weight Change According to Ketonuria After Fasting in the Healthy Obese
ORIGINAL ARTICLE Endocrinology, Nutrition & Metabolism http://dx.doi.org/10.3346/jkms.2012.27.3.250 • J Korean Med Sci 2012; 27: 250-254 Different Response of Body Weight Change According to Ketonuria after Fasting in the Healthy Obese Hyeon-Jeong Kim1, Nam-Seok Joo1, The relationship between obesity and ketonuria is not well-established. We conducted a Kwang-Min Kim1, Duck-Joo Lee1, retrospective observational study to evaluate whether their body weight reduction response and Sang-Man Kim2 differed by the presence of ketonuria after fasting in the healthy obese. We used the data of 42 subjects, who had medical records of initial urinalysis at routine health check-up and 1Department of Family Practice and Community Health, Ajou University School of Medicine, Suwon; follow-up urinalysis in the out-patient clinic, one week later. All subjects in the initial 2Department of Family Medicine, CHA Biomedical urinalysis showed no ketonuria. However, according to the follow-up urinalysis after three Center, CHA University College of Medicine, Seoul, subsequent meals fasts, the patients were divided into a non-ketonuria group and Korea ketonuria group. We compared the data of conventional low-calorie diet programs for ± Received: 20 August 2011 3 months for both groups. Significantly greater reduction of body weight (-8.6 3.6 kg vs 2 2 Accepted: 17 January 2012 -1.1 ± 2.2 kg, P < 0.001), body mass index (-3.16 ± 1.25 kg/m vs -0.43 ± 0.86 kg/m , P < 0.001) and waist circumference (-6.92 ± 1.22 vs -2.32 ± 1.01, P < 0.001) was Address for Correspondence: observed in the ketonuria group compared to the non-ketonuria group. -

Deficient Diabetic Mice
Diminished Loss of Proteoglycans and Lack of Albuminuria in Protein Kinase C-␣–Deficient Diabetic Mice Jan Menne,1,2 Joon-Keun Park,2 Martin Boehne,2 Marlies Elger,2 Carsten Lindschau,2 Torsten Kirsch,2 Matthias Meier,2 Faikah Gueler,2 Annette Fiebeler,3 Ferdinand H. Bahlmann,2 Michael Leitges,4 and Hermann Haller2 Activation of protein kinase C (PKC) isoforms has been implicated in the pathogenesis of diabetic nephropathy. We showed earlier that PKC-␣ is activated in the kid- iabetes affects Ͼ300 million people worldwide; -neys of hyperglycemic animals. We now used PKC-␣؊/؊ 20–40% will develop overt nephropathy. Diabe mice to test the hypothesis that this PKC isoform tes is the most common cause of end-stage mediates streptozotocin-induced diabetic nephropathy. Drenal disease. The earliest clinical sign of ne- We observed that renal and glomerular hypertrophy was phropathy is microalbuminuria. Microalbuminuria also ؊ ؊ similar in diabetic wild-type and PKC-␣ / mice. How- heralds impending cardiovascular morbidity and mortality ever, the development of albuminuria was almost absent (1–4). Microalbuminuria predicts overt proteinuria, which ؊/؊␣ in the diabetic PKC- mice. The hyperglycemia-in- is now believed to actively promote renal insufficiency (5). duced downregulation of the negatively charged base- Therefore, successful treatment of diabetic patients ment membrane heparan sulfate proteoglycan perlecan -؊ ؊ should aim for the prevention or regression of albumin was completely prevented in the PKC-␣ / mice, com- pared with controls. We then asked whether transform- uria. Hyperglycemia seems to cause microalbuminuria in   diabetic patients (6,7). However, how the metabolic dis- ing growth factor- 1 (TGF- 1) and/or vascular endothelial growth factor (VEGF) is implicated in the turbance causes cellular effects is incompletely under- PKC-␣–mediated changes in the basement membrane. -

Ileal Neobladder: an Important Cause of Non-Anion Gap Metabolic Acidosis
The Journal of Emergency Medicine, Vol. 52, No. 5, pp. e179–e182, 2017 Ó 2017 Elsevier Inc. All rights reserved. 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2016.12.036 Clinical Communications: Adult ILEAL NEOBLADDER: AN IMPORTANT CAUSE OF NON-ANION GAP METABOLIC ACIDOSIS Jesse W. St. Clair, MD and Matthew L. Wong, MD, MPH Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Boston, Massachusetts and Department of Emergency Medicine, Harvard Medical School, Boston, Massachusetts Reprint Address: Matthew L. Wong, MD, MPH, Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Rosenberg Building, 2nd Floor, 1 Deaconess Road, Boston, MA 02446 , Abstract—Background: The differential diagnosis for a disease, or medications such as acetazolamide. non-anion gap metabolic acidosis is probably less well Commonly used mnemonics to remember the differential known than the differential diagnosis for an anion gap for the non-anion gap metabolic acidosis include metabolic acidosis. One etiology of a non-anion gap acidosis ‘‘ABCD’’ for ‘‘Addison’s, Bicarbonate loss, Chloride is the consequence of ileal neobladder urinary diversion (administration), and Drugs,’’ as well as ‘‘HARDUP’’ for the treatment of bladder cancer. Case Report: We pre- for ‘‘Hyperchloremia, Acetazolamide and Addison’s, sent a case of a patient with an ileal neobladder with a severe non-anion gap metabolic acidosis caused by a Renal Tubular Acidosis, Diarrhea, Ureteroenterostomies, urinary tract infection and ureteroenterostomy. Why and Pancreaticoenterostomies’’ (Table 1) (1). Should an Emergency Physician Be Aware of This?: Part Ureteroenterostomies are when the ureter has an of the ileal neobladder surgery includes ureteroenteros- abnormal connection with a segment of intestine. -

Interpretation of Canine and Feline Urinalysis
$50. 00 Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Interpretation of Canine and Feline Urinalysis Dennis J. Chew, DVM Stephen P. DiBartola, DVM Clinical Handbook Series Preface Urine is that golden body fluid that has the potential to reveal the answers to many of the body’s mysteries. As Thomas McCrae (1870-1935) said, “More is missed by not looking than not knowing.” And so, the authors would like to dedicate this handbook to three pioneers of veterinary nephrology and urology who emphasized the importance of “looking,” that is, the importance of conducting routine urinalysis in the diagnosis and treatment of diseases of dogs and cats. To Dr. Carl A. Osborne , for his tireless campaign to convince veterinarians of the importance of routine urinalysis; to Dr. Richard C. Scott , for his emphasis on evaluation of fresh urine sediments; and to Dr. Gerald V. Ling for his advancement of the technique of cystocentesis. Published by The Gloyd Group, Inc. Wilmington, Delaware © 2004 by Nestlé Purina PetCare Company. All rights reserved. Printed in the United States of America. Nestlé Purina PetCare Company: Checkerboard Square, Saint Louis, Missouri, 63188 First printing, 1998. Laboratory slides reproduced by permission of Dennis J. Chew, DVM and Stephen P. DiBartola, DVM. This book is protected by copyright. ISBN 0-9678005-2-8 Table of Contents Introduction ............................................1 Part I Chapter 1 Sample Collection ...............................................5 -

A Dipstick Test Combined with Urine Specific Gravity Improved the Accuracy of Proteinuria Determination in Pregnancy Screening
Kobe J. Med. Sci., Vol. 56, No. 4, pp. E165-E172, 2010 A Dipstick Test Combined with Urine Specific Gravity Improved the Accuracy of Proteinuria Determination in Pregnancy Screening NATSUKO MAKIHARA1, MINEO YAMASAKI1,2, HIROKI MORITA1, and HIDETO YAMADA1* 1Division of Obstetrics and Gynecology, Department of Surgery-related, and 2Division of Integrated Medical Education, Department of Community Medicine and Social Healthcare Science, Kobe University Graduate School of Medicine, 7-5-1 Kusunoki-cho, Chuo-ku, Kobe, 650-0017, Japan. Received 12 July 2010/ Accepted 20 August 2010 Key Words: dipstick test, pregnancy proteinuria, protein/creatinine ratio, urine specific gravity Proteinuria screening using a semi-quantitative dipstick test of the spot urine in antenatal clinic is known to have high false-positive rates. The aim of this study was to assess availability of a dipstick test combined with the urine specific gravity for the determination of pathological proteinuria. A dipstick test was performed on 582 urine samples obtained from 283 pregnant women comprising 260 with normal blood pressure and 23 with pregnancy-induced hypertension. The urine protein (P) and creatinine (C) concentrations, specific gravity (SG), P/C ratio were determined, and compared with dipstick test results. The P concentration increased along the stepwise augmentations in dipstick test result. Frequencies of the urine samples with 0.265 or more P/C ratio were 0.7% with − dipstick test result, 0.7% with the ± result, 3.3% with the 1+ result, and 88.9% with the ≥2+ result. However, if the urine specific gravity was low, frequencies of the high P/C ratio were 5.0% with ± dipstick test result and 9.3% with the 1+ result. -

Paroxysmal Nocturnal Hemoglobinuria
Paroxysmal nocturnal hemoglobinuria Description Paroxysmal nocturnal hemoglobinuria is an acquired disorder that leads to the premature death and impaired production of blood cells. The disorder affects red blood cells (erythrocytes), which carry oxygen; white blood cells (leukocytes), which protect the body from infection; and platelets (thrombocytes), which are involved in blood clotting. Paroxysmal nocturnal hemoglobinuria affects both sexes equally, and can occur at any age, although it is most often diagnosed in young adulthood. People with paroxysmal nocturnal hemoglobinuria have sudden, recurring episodes of symptoms (paroxysmal symptoms), which may be triggered by stresses on the body, such as infections or physical exertion. During these episodes, red blood cells are prematurely destroyed (hemolysis). Affected individuals may pass dark-colored urine due to the presence of hemoglobin, the oxygen-carrying protein in blood. The abnormal presence of hemoglobin in the urine is called hemoglobinuria. In many, but not all cases, hemoglobinuria is most noticeable in the morning, upon passing urine that has accumulated in the bladder during the night (nocturnal). The premature destruction of red blood cells results in a deficiency of these cells in the blood (hemolytic anemia), which can cause signs and symptoms such as fatigue, weakness, abnormally pale skin (pallor), shortness of breath, and an increased heart rate. People with paroxysmal nocturnal hemoglobinuria may also be prone to infections due to a deficiency of white blood cells. Abnormal platelets associated with paroxysmal nocturnal hemoglobinuria can cause problems in the blood clotting process. As a result, people with this disorder may experience abnormal blood clotting (thrombosis), especially in large abdominal veins; or, less often, episodes of severe bleeding (hemorrhage). -

The Effect of Flood Diuresis on Hemo-Globinuria
THE EFFECT OF FLOOD DIURESIS ON HEMO- GLOBINURIA. BY HERBERT HAESSLERj M.D. (From the Laboratories of The Rockefeller Inatitute for Medical Research.) (Received for publication, November 9, 1921.) The fact is well recognized that a considerable quantity of hemo- globin must be free in the plasma if any is to pass the renal barrier and appear in the urine. The pigment is, like dextrose, a "threshold substance." It readily penetrates into the renal tubules but is absorbed again more or less completely during its course through them. t This being true, diuresis should diminish the chances of absorption by hastening the flow of fluid, and tend to lead to the appearance of the pigment in the urine. Evidence will here be presented that such is the case. Hemoglobinuria, like glycosuria, is much favored by flood diuresis. Method. A concentrated solution of hemoglobin was abruptly thrown into the circulation of rabbits and dogs, followed in some instances by a slower injection of salt solution. The amount of pigment introduced was slightly less than that required to produce hemoglobinuria in the absence of diuresis. The urine was collected at intervals by catheter. All of the animals were males. Individuals were selected with normal kidneys, as indicated by ~e general character of the urine and proven by the autopsy findings. Great care was necessary to prevent hemorrhage during the catheterization of the rabbits, and despite it a few red cells were frequently encountered after- wards in the urine. For this reason the experiments were repeated on dogs, in which the complication can be avoided. -

Acute Kidney Injury and Chronic Kidney Disease: Classifications and Interventions for Children and Adults Teresa V
Acute Kidney Injury and Chronic Kidney Disease: Classifications and Interventions for Children and Adults Teresa V. Lewis, PharmD, BCPS Assistant Professor of Pharmacy Practice University of Oklahoma College of Pharmacy Adjunct Assistant Professor of Pediatrics University of Oklahoma College of Medicine 1 Disclosures • Teresa V. Lewis, Pharm.D., BCPS • Nothing to disclose Objectives 1. When given specific patient details, identify those with increased Identify which adult or pediatric patients are at risk for development of acute kidney injury (AKI) and recommend appropriate preventive interventions. 2. Design an evidence-based plan to manage AKI for a given patient. 3. Compare and contrast the RIFLE, pRIFLE, and Kidney Disease Improving Global Outcomes (KDIGO) classification systems for AKI. 4. List risk factors for development of chronic kidney disease (CKD). 5. Compare and contrast the Kidney Disease Outcomes Quality Initiative (KDOQI) staging of CKD with the Kidney Disease Improving Global Outcomes (KDIGO) CKD staging criteria. 6. Design an evidence-based plan to prevent progression of CKD for a given patient. 3 Kidney Development and Maturation • Nephrogenesis • Begins around 9 weeks of gestation • Complete by 36 weeks of gestation • Immature renal function at birth • Lower renal blood flow • Immature glomeruli • Immature renal tubule function • Kidney function will be similar to adult values by age 2 years 4 Presentation Outline • Diagnostic Workup • Acute Kidney Injury • Drug Induced Nephrotoxicity • Chronic Kidney Disease 5 DIAGNOSTIC WORK-UP Blood Urea Nitrogen (BUN) • Normal: 8-20 mg/dL • Amino-acids metabolized to ammonia and converted in liver to urea • Urea is filtered and reabsorbed in proximal tubule (dependent on water reabsorption) • Normal BUN:Serum creatinine (Scr) ratio is 10-15:1 • Elevated BUN:Scr ratio suggests true or effective volume depletion 7 Serum Creatinine (Scr) • Freely filtered • Actively secreted • Scr lags behind glomerular filtration rate (GFR) by 1-2 days due to: 1. -

Biochemical Profiling of Renal Diseases
INTRODUCTION TO LABORATORY PROFILING Alan H. Rebar, DVM, Ph.D., Diplomate ACVP Purdue University, Discovery Park 610 Purdue Mall, West Lafayette, IN 47907-2040 Biochemical profiling may be defined as the use of multiple blood chemistry determinations to assess the health status of various organ systems simultaneously. Biochemical profiling rapidly has become a major diagnostic aid for the practicing veterinarian for several reasons. First, a more educated clientele has come to expect increased diagnostic sophistication. Secondly, the advent of high-volume clinical pathology laboratories has resulted in low prices that make profiling in veterinary practice feasible and convenient. In addition, improved technology has resulted in the development of procedures that can be used to obtain accurate analyses on microsamples of serum. Such procedures offer obvious advantages to veterinarians, who in the past were hindered by requirements for large sample size. Although biochemical profiling offers exciting potential, it is not a panacea. Since standard chemical screens provide 12 to 30 test results, interpretation of data may be extremely complex. Interpretation is often clouded by the fact that perfectly normal animals may have, indeed, are expected to have, an occasional abnormal test result. It is estimated that in a panel of 12 chemistry tests, approximately 46% of all normal subjects will have at least one abnormal test result. Such abnormalities do not reflect inaccuracies in laboratory test procedures but rather the way in which reference (or normal) values are determined. In order to establish the "normal range" for a given test, the procedure is performed on samples from a large population of clinically normal individuals. -

Evaluation of Gross and Microscopic Hematuria
EVALUATION OF GROSS AND MICROSCOPIC HEMATURIA APRIL GARDNER, MSBS, PA - C ASSOCIATE PROGRAM DIRECTOR THE UNIVERSITY OF TOLEDO PA PROGRAM OBJECTIVES • Define the terms gross hematuria and microscopic hematuria. • Identify etiologies of hematuria. • Identify risk factors for a urologic cancer in a patient with gross or microscopic hematuria. • Define the term “full evaluation.” • Identify indications for a full evaluation. • Identify labs and diagnostics to evaluate hematuria. • Identify the appropriate follow-up for patients with hematuria. 2 CASE #1 Ms. T is a healthy 50 year-old female, s/p TAH/BSO 15 years ago for severe endometriosis. She presents today for her annual physical exam required by her employer. She has no new complaints and there is no history of any urologic complaints. Physical exam is completely normal Urine dipstick shows 1+ blood, pH 6.0, negative for ketones, glucose, nitrites and leukocyte esterase Microscopic evaluation shows 8 RBCs, no WBCs, bacteria, yeast, crystals, or casts CASE #1 • Should you prescribe an antibiotic for Ms. T today? • Does she need any further follow-up? • If yes, what would follow-up include? CASE #2 Mr. D is a 38 year-old healthy, monogamous married male with 4 children, presenting for a vasectomy consultation. He denies any complaints, including urologic complaints. He takes no medications. He tells you he ran a marathon 2 days ago and then finished building a deck in his backyard yesterday. Physical exam is completely normal Urine dipstick shows 1+ blood, pH 6.0, negative for protein, ketones, glucose, nitrites and leukocyte esterase Microscopic evaluation shows 3 RBCs, no WBCs, bacteria, yeast, crystals, or casts CASE #2 • Should you prescribe an antibiotic for Mr.