Brief History of American Hospitals
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Origin of Bimaristans (Hospitals) in Islamic Medical History
The Origin of Bimaristans (Hospitals) in Islamic Medical History IMPORTANT NOTICE: Author: Dr. Sharif Kaf Al-Ghazal Chief Editor: Prof. Mohamed El-Gomati All rights, including copyright, in the content of this document are owned or controlled for these purposes by FSTC Limited. In Deputy Editor: Prof. Mohammed Abattouy accessing these web pages, you agree that you may only download the content for your own personal non-commercial Associate Editor: Dr. Salim Ayduz use. You are not permitted to copy, broadcast, download, store (in any medium), transmit, show or play in public, adapt or Release Date: April 2007 change in any way the content of this document for any other purpose whatsoever without the prior written permission of FSTC Publication ID: 682 Limited. Material may not be copied, reproduced, republished, Copyright: © FSTC Limited, 2007 downloaded, posted, broadcast or transmitted in any way except for your own personal non-commercial home use. Any other use requires the prior written permission of FSTC Limited. You agree not to adapt, alter or create a derivative work from any of the material contained in this document or use it for any other purpose other than for your personal non-commercial use. FSTC Limited has taken all reasonable care to ensure that pages published in this document and on the MuslimHeritage.com Web Site were accurate at the time of publication or last modification. Web sites are by nature experimental or constantly changing. Hence information published may be for test purposes only, may be out of date, or may be the personal opinion of the author. -

Hospital Patient and Visitor Signs and Notices Federal Requirements Required to Post Placement Authority Additional Information
Hospital Patient and Visitor Signs and Notices Federal Requirements Required to Post Placement Authority Additional Information Affordable Care Act – Language In significant publications and Notice requirement, HHS Translated Resources for Covered Entities: Assistance Service. significant communications 45 C.F.R. §§ https://www.hhs.gov/civil-rights/for-individuals/section- targeted to beneficiaries, 92.8(d)(1)-(2). 1557/translated-resources/index.html. enrollees, applicants, and members of the public, except for significant publications and significant communications that are small-sized, such as postcards and tri-fold brochures; In conspicuous physical locations where the entity interacts with the public; and In a conspicuous location on the covered entity's website accessible from the home page of the covered entity's website. Affordable Care Act – Participation in Post signs in the facility in 42 C.F.R. § 312(a)(2). Standardized written notices must be made available upon Shared Savings Program. settings in which beneficiaries request. Provide notice to beneficiaries at point receive primary care. of care of the participation in the Must use template language developed by CMS and must Shared Savings Program and of the meet marketing material requirements per 42 C.F.R. § opportunity to decline claims data 425.310. sharing under § 425.708. Notice is carried out when signs are posted. CMS has provided template poster language in the ACO Marketing Toolkit on the Shared Savings Program ACO Portal, accessible to ACO participants, available at: https://portal.cms.gov. Illinois Health and Hospital Association Last updated February, 2020 This document is intended to be a guide for IHA Members on the signs and notices hospitals are required to post or provide to patients and visitors under federal law. -

Strengthening the Public Health Infrastructure
STRENGTHENING THE PUBLIC HEALTH INFRASTRUCTURE American College of Physicians A Position Paper 2012 STRENGTHENING THE PUBLIC HEALTH INFRASTRUCTURE A Position Paper of the American College of Physicians This paper, written by Michelle Kline, was developed for the Health and Public Policy Committee of the American College of Physicians: Robert M. Centor, MD, FACP, Chair; Robert McLean, MD, FACP, Vice Chair; Vineet Arora, MD, FACP; Charles Cutler, MD, FACP; Thomas D. DuBose, Jr. MD, MACP; Jacqueline W. Fincher, MD, MACP; Luke. O. Hansen, MD; Richard P. Holm, MD, FACP; Ali Kahn, MD; Lindsey S. Merritt; Mary Newman, MD, FACP; P. Preston Reynolds, MD, FACP; and Wayne Riley, MD, MBA, MACP with contributions from Virginia L. Hood, MBBS MPH FACP (ACP President); Yul Ejnes, MD, FACP (Chair, ACP Board of Regents), and Donald W. Hatton, MD, FACP (Chair, Medical Practice and Quality Committee). It was approved by the Board of Regents on 16 April 2012. i How to cite this paper: American College of Physicians. Strengthening the Public Health Infrastructure in a Reformed Health Care System. Philadelphia: American College of Physicians; 2012: Policy Paper. (Available from American College of Physicians, 190 N. Independence Mall West, Philadelphia, PA 19106.) Copyright © 2012 American College of Physicians. All rights reserved. Individuals may photocopy all or parts of Position Papers for educational, not-for-profit uses. These papers may not be reproduced for commercial, for-profit use in any form, by any means (electronic, mechanical, xerographic, or other) or held in any information storage or retrieval system without the written permission of the publisher. For questions about the content of this Position Paper, please contact ACP, Division of Governmental Affairs and Public Policy, Suite 700, 25 Massachusetts Avenue NW, Washington, DC 20001-7401; telephone 202-261-4500. -

Preventive Health Care
PREVENTIVE HEALTH CARE DANA BARTLETT, BSN, MSN, MA, CSPI Dana Bartlett is a professional nurse and author. His clinical experience includes 16 years of ICU and ER experience and over 20 years of as a poison control center information specialist. Dana has published numerous CE and journal articles, written NCLEX material, written textbook chapters, and done editing and reviewing for publishers such as Elsevire, Lippincott, and Thieme. He has written widely on the subject of toxicology and was recently named a contributing editor, toxicology section, for Critical Care Nurse journal. He is currently employed at the Connecticut Poison Control Center and is actively involved in lecturing and mentoring nurses, emergency medical residents and pharmacy students. ABSTRACT Screening is an effective method for detecting and preventing acute and chronic diseases. In the United States healthcare tends to be provided after someone has become unwell and medical attention is sought. Poor health habits play a large part in the pathogenesis and progression of many common, chronic diseases. Conversely, healthy habits are very effective at preventing many diseases. The common causes of chronic disease and prevention are discussed with a primary focus on the role of health professionals to provide preventive healthcare and to educate patients to recognize risk factors and to avoid a chronic disease. nursece4less.com nursece4less.com nursece4less.com nursece4less.com 1 Policy Statement This activity has been planned and implemented in accordance with the policies of NurseCe4Less.com and the continuing nursing education requirements of the American Nurses Credentialing Center's Commission on Accreditation for registered nurses. It is the policy of NurseCe4Less.com to ensure objectivity, transparency, and best practice in clinical education for all continuing nursing education (CNE) activities. -

The Evolution of Hospitals from Antiquity to the Renaissance
Acta Theologica Supplementum 7 2005 THE EVOLUTION OF HOSPITALS FROM ANTIQUITY TO THE RENAISSANCE ABSTRACT There is some evidence that a kind of hospital already existed towards the end of the 2nd millennium BC in ancient Mesopotamia. In India the monastic system created by the Buddhist religion led to institutionalised health care facilities as early as the 5th century BC, and with the spread of Buddhism to the east, nursing facilities, the nature and function of which are not known to us, also appeared in Sri Lanka, China and South East Asia. One would expect to find the origin of the hospital in the modern sense of the word in Greece, the birthplace of rational medicine in the 4th century BC, but the Hippocratic doctors paid house-calls, and the temples of Asclepius were vi- sited for incubation sleep and magico-religious treatment. In Roman times the military and slave hospitals were built for a specialised group and not for the public, and were therefore not precursors of the modern hospital. It is to the Christians that one must turn for the origin of the modern hospital. Hospices, originally called xenodochia, ini- tially built to shelter pilgrims and messengers between various bishops, were under Christian control developed into hospitals in the modern sense of the word. In Rome itself, the first hospital was built in the 4th century AD by a wealthy penitent widow, Fabiola. In the early Middle Ages (6th to 10th century), under the influence of the Be- nedictine Order, an infirmary became an established part of every monastery. -
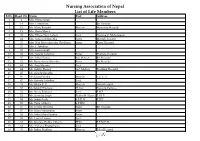
Nursing Association of Nepal List of Life Members S.No
Nursing Association of Nepal List of Life Members S.No. Regd. No. Name Post Address 1 2 Mrs. Prema Singh 2 14 Mrs. I. Mathema Bir Hospital 3 15 Ms. Manu Bangdel Matron Maternity Hospital 4 19 Mrs. Geeta Murch 5 20 Mrs. Dhana Nani Lohani Lect. Nursing C. Maharajgunj 6 24 Mrs. Saraswati Shrestha Sister Mental Hospital 7 25 Mrs. Nati Maya Shrestha (Pradhan) Sister Kanti Hospital 8 26 Mrs. I. Tuladhar 9 32 Mrs. Laxmi Singh 10 33 Mrs. Sarada Tuladhar Sister Pokhara Hospital 11 37 Mrs. Mita Thakur Ad. Matron Bir Hospital 12 42 Ms. Rameshwori Shrestha Sister Bir Hospital 13 43 Ms. Anju Sharma Lect. 14 44 Ms. Sabitry Basnet Ast. Matron Teaching Hospital 15 45 Ms. Sarada Shrestha 16 46 Ms. Geeta Pandey Matron T.U.T. H 17 47 Ms. Kamala Tuladhar Lect. 18 49 Ms. Bijaya K. C. Matron Teku Hospital 19 50 Ms.Sabitry Bhattarai D. Inst Nursing Campus 20 52 Ms. Neeta Pokharel Lect. F.H.P. 21 53 Ms. Sarmista Singh Publin H. Nurse F. H. P. 22 54 Ms. Sabitri Joshi S.P.H.N F.H.P. 23 55 Ms. Tuka Chhetry S.P.HN 24 56 Ms. Urmila Shrestha Sister Bir Hospital 25 57 Ms. Maya Manandhar Sister 26 58 Ms. Indra Maya Pandey Sister 27 62 Ms. Laxmi Thakur Lect. 28 63 Ms. Krishna Prabha Chhetri PHN F.P.M.C.H. 29 64 Ms. Archana Bhattacharya Lect. 30 65 Ms. Indira Pradhan Matron Teku Hospital S.No. Regd. No. Name Post Address 31 67 Ms. -

Lawrlwytho'r Atodiad Gwreiddiol
Operational services structure April 2021 14/04/2021 Operational Leadership Structures Director of Operations Director of Nursing & Quality Medical Director Lee McMenamy Joanne Hiley Dr Tessa Myatt Medical Operations Operations Clinical Director of Operations Deputy Director of Nursing & Deputy Medical Director Hazel Hendriksen Governance Dr Jose Mathew Assistant Clinical Director Assistant Director of Assistant Clinical DWiraerctringor ton & Halton Operations Corporate Corporate Lorna Pink Assistant Assistant Director Julie Chadwick Vacant Clinical Director of Nursing, AHP & Associate Clinical Director Governance & Professional Warrington & Halton Compliance Standards Assistant Director of Operations Assistant Clinical Director Dr Aravind Komuravelli Halton & Warrington Knowsley Lee Bloomfield Claire Hammill Clare Dooley Berni Fay-Dunkley Assistant Director of Operations Knowsley Associate Medical Director Nicky Over Assistant Clinical Director Allied Health Knowsley Assistant Director of Sefton Professional Dr Ashish Kumar AssiOstapenrta Dtiironesc tKnor oofw Oslpeeyr ations Sara Harrison Lead Nicola Over Sefton James Hester Anne Tattersall Assistant Clinical Director Associate Clinical Director Assistant Director of St Helens & Knowsley Inpatients St Helens Operations Sefton Debbie Tubey Dr Raj Madgula AssistanAt nDniree Tcatttore ofrs aOllp erations Head of St Helens & Knowsley Inpatients Safeguarding Tim McPhee Assistant Clinical Director Sarah Shaw Assistant Director of Associate Medical Director Operations St Helens Mental Health -

Indonesia Healthcare: Growing Opportunities
Indonesia Healthcare: Growing Opportunities Presented on 23 April 2021 by Leona A. Karnali About the Presenters Leona A. Karnali CEO Primaya Hospital, Indonesia Leona leads Primaya Hospital Group, a leading private hospital group operating 10 hospitals located strategically across Indonesia. Prior to her appointment as CEO, she was the COO for the past 5 years leading the hospital’s transformation in human capital, procurement, marketing and international relationships. Her expertise and experience range from operational and strategic management to risk and financial management through previous work experiences in education, banking, and private equity. Leona graduated with a Master of Science degree in mechanical engineering from Massachusetts Institute of Technology. She is a CFA charterholder and is a certified FRM. Company Profile About Primaya Hospital 10 1325 3 operating operating regional hospitals beds clusters 672 157 1661 general licensed specialists practitioners nurses A Multi-Specialty Hospital Network Providing Accredited by Joint Commission International Professional & Caring since 2014 Healthcare Services Our Hospital Network West Bekasi Makassar Bekasi Cluster: Tangerang Cluster: Makassar Cluster: PRIMAYA HOSPITAL WEST BEKASI PRIMAYA HOSPITAL TANGERANG PRIMAYA HOSPITAL MAKASSAR Kalimalang, West Bekasi Cikokol, Tangerang Jend. Urip Sumohardjo, Makassar PRIMAYA HOSPITAL EAST BEKASI PRIMAYA HOSPITAL PASAR KEMIS PRIMAYA HOSPITAL INCO SOROWAKO Margahayu, East Bekasi Pasar Kemis, Tangerang – Opening March 2021 Sorowako PRIMAYA HOSPITAL NORTH BEKASI PRIMAYA EVASARI HOSPITAL Teluk Pucung, North Bekasi Rawasari, Central Jakarta • Mid-size to Large Hospitals PRIMAYA HOSPITAL KARAWANG PRIMAYA HOSPITAL BETANG PAMBELUM with 100-250 beds Galuh Mas, Karawang Tjilik Riwut, Palangkaraya • Located across Indonesia PRIMAYA HOSPITAL SUKABUMI PRIMAYA HOSPITAL PANGKAL PINANG • All Primaya Hospitals are Sukaraja, Sukabumi – Opening March 2021 Pangkal Pinang City, Kep. -

THE DEVELOPMENT of NURSING EDUCATION in the ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I
THE DEVELOPMENT OF NURSING EDUCATION IN THE ENGLISH-SPEAKING CARIBBEAN ISLANDS by PEARL I. GARDNER, B.S.N., M.S.N., M.Ed. A DISSERTATION IN HIGHER EDUCATION Submitted to the Graduate Faculty of Texas Tech University in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF EDUCATION Approved Accepted Dean of the Graduate School August, 1993 ft 6 l^yrr^7^7 801 J ,... /;. -^o ACKNOWLEDGEMENTS C?^ /c-j/^/ C^ ;^o.^^ I would like to thank Dr. Clyde Kelsey, Jr., for his C'lp '^ ^unflagging support, his advice and his constant vigil and encouragement in the writing of this dissertation. I would also like to thank Dr. Patricia Yoder-Wise who acted as co-chairperson of my committee. Her advice was invaluable. Drs. Mezack, Willingham, and Ewalt deserve much praise for the many times they critically read the manuscript and gave their input. I would also like to thank Ms. Janey Parris, Senior Program Officer of Health, Guyana, the government officials of the Caribbean Embassies, representatives from the Caribbean Nursing Organizations, educators from the various nursing schools and librarians from the archival institutions and libraries in Trinidad and Tobago and Jamaica. These individuals agreed to face-to-face interviews, answered telephone questions and mailed or faxed information on a regular basis. Much thanks goes to Victor Williams for his computer assistance and to Hannelore Nave for her patience in typing the many versions of this manuscript. On a personal level I would like to thank my niece Eloise Walters for researching information in the nursing libraries in London, England and my husband Clifford for his belief that I could accomplish this task. -

Design and Implementation of Health Information Systems
Design and implementation of health information systems Edited by Theo Lippeveld Director of Health Information Systems, John Snow Inc., Boston, MA, USA Rainer Sauerborn Director of the Department of Tropical Hygiene and Public Health, University of Heidelberg, Germany Claude Bodart Project Director, German Development Cooperation, Manila, Philippines World Health Organization Geneva 2000 WHO Library Cataloguing in Publication Data Design and implementation of health information systems I edited by Theo Lippeveld, Rainer Sauerborn, Claude Bodart. 1.1nformation systems-organization and administration 2.Data collection-methods I.Lippeveld, Theo II.Sauerborn, Rainer III.Bodart, Claude ISBN 92 4 1561998 (NLM classification: WA 62.5) The World Health Organization welcomes requests for permission to reproduce or translate its pub lications, in part or in full. Applications and enquiries should be addressed to the Office of Publi cations, World Health Organization, Geneva, Switzerland, which will be glad to provide the latest information on any changes made to the text, plans for new editions, and reprints and translations already available. © World Health Organization 2000 Publications of the World Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. All rights reserved. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the World Health Or ganization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specific companies or of certain manufacturers' products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

Health Information Technology Basics Institute for Health & Socio-Economic Policy
Health Information Technology Basics Institute for Health & Socio-Economic Policy © Copyright IHSP 2009. All rights reserved. Table of Contents Part I Introduction 1 Part II Why Workplace Technologies Change 2 Section 1: Overview 2 Section 2: Confl icting Values 2 Section 3: Management Secrets 3 Part III Routinizing Patient Care 8 Section 1: Overview 8 Section 2: The Core Technologies 9 Section 3: Supplemental Technologies 17 Part IV Nursing Values and Resistance 19 I FOR CNA/NNOC Part I Introduction Health information technology (HIT) is widely celebrated as a universal healthcare fix. Promoters say it will contain costs, improve quality, and modernize medical care. But such promises are the public relations messages of the HIT and healthcare industries. Is HIT really the panacea to cure our healthcare crisis, or are there consequences that aren’t being discussed? RNs have good reason to be wary. Patient care processes in some hospitals have already been transformed by HIT, and many other hospitals will be adopting it in the next few years. Among other types, hospitals are adopting • electronic medical records, • clinical decision support systems, • e-prescribing, • medication dispensing, • radio frequency identification and tracking, • medical credit scoring, • telemedicine, and • robots. Clinical decision support systems (CDSS) are one widespread technology that affects patient care directly. Of the 5,139 U.S. hospitals reporting (almost all hospitals not run by the federal government), 67.6% have adopted fully automated CDSS and 8% have either begun the installation process or have contracted to do so. A revolution is well underway. It will soon reach RNs and patients in every hospital. -

1 Role of Hospitals at the Beginning of the New
MANAGEMENT IN HEALTH CARE PRACTICE A Handbook for Teachers, Researchers and Health Professionals Title ROLE OF HOSPITALS AT THE BEGINNING OF THE NEW MILLENNIUM Module: 5.4 ECTS: 0.2 Author Želimir Jakši ć, MD, PhD, Professor Emeritus Andrija Štampar School of Public Health, Medical School, University of Zagreb Address for Želimir Jakši ć Correspondence Andrija Štampar School of Public Health, Medical School, University of Zagreb Rockefellerova 4, 10000 Zagreb, Croatia [email protected] Keywords Hospital, Public Health, Organization of Health Services Learning objectives After completing this module students and public health professionals should: • be aware of the role of the hospital in the community; • be aware of the historical development of hospital services; • recognize needs for analysis of the hospital functions; • know listing the characteristics of different models of organization of hospital services; • improve the knowledge and understanding of the of function of the health care system. Abstract During a long history, hospitals were continuously changing so that diversity is one of their characteristics. Being a part of a local culture, they also reflect general global trends. At present, the winds of globalisation are stronger, following an overall trend in technology and economics. Changes in technologies will induce changes in management (“new plants do not survive in old pots”). New imaging technologies need a better clinical feed-back, and the pattern of “industry-like” hospital, where specialists work in their narrow fields on a production-line becomes inappropriate for them. Human resource management becomes more important than economic and technical management dominating at present. Teaching methods Introductory lecture, exercises, individual work and small group discussions.