Chromosome Instability in Human Lung Cancers: Possible Underlying Mechanisms and Potential Consequences in the Pathogenesis
Total Page:16
File Type:pdf, Size:1020Kb
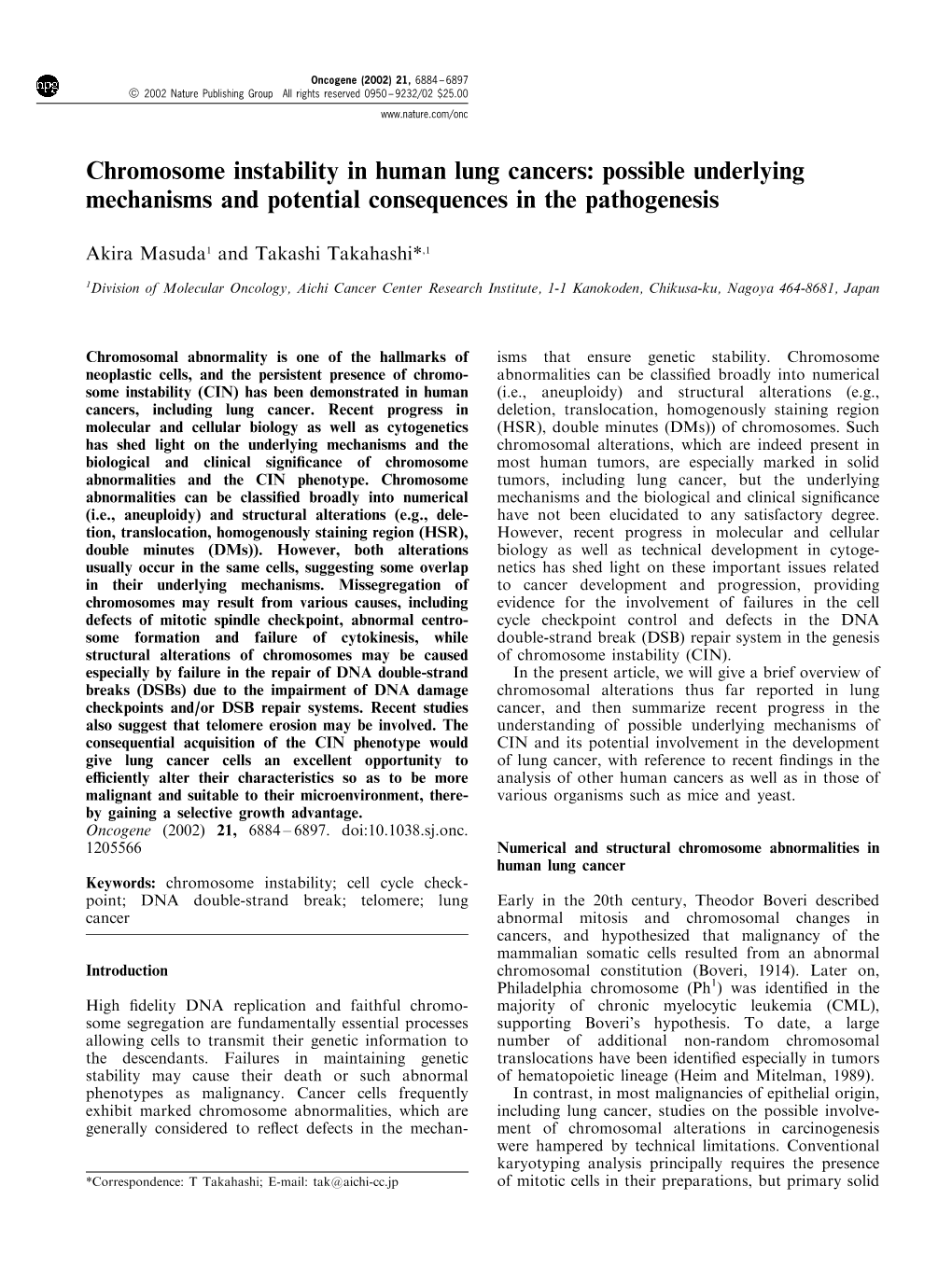
Load more
Recommended publications
-
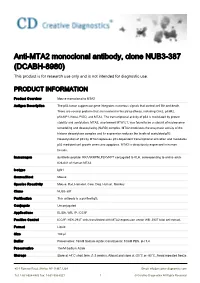
Anti-MTA2 Monoclonal Antibody, Clone NUB3-387 (DCABH-8980) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-MTA2 monoclonal antibody, clone NUB3-387 (DCABH-8980) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Mouse monoclonal to MTA2 Antigen Description The p53 tumor suppressor gene integrates numerous signals that control cell life and death. There are several proteins that are involved in the p53 pathway, including Chk2, p53R2, p53AIP1, Noxa, PIDD, and MTA2. The transcriptional activity of p53 is modulated by protein stability and acetylation. MTA2, also termed MTA1L1, was found to be a subunit of nucleosome remodeling and deacetylating (NuRD) complex. MTA2 modulates the enzymatic activity of the histone deacetylase complex and its expression reduces the levels of acetylated p53. Deacetylation of p53 by MTA2 represses p53 dependent transcriptional activation and modulates p53 mediated cell growth arrest and apoptosis. MTA2 is ubiquitously expressed in human tissues. Immunogen Synthetic peptide: RRAARRPNLPLKVKPT conjugated to KLH, corresponding to amino acids 626-641 of Human MTA2 Isotype IgG1 Source/Host Mouse Species Reactivity Mouse, Rat, Hamster, Cow, Dog, Human, Monkey Clone NUB3-387 Purification This antibody is a purified IgG. Conjugate Unconjugated Applications ELISA, WB, IP, ICC/IF Positive Control ICC/IF: HEK-293T cells transfected with MTA2 expression vector WB: 293T total cell extract. Format Liquid Size 100 μl Buffer Preservative: 15mM Sodium Azide; Constituents: 10mM PBS, pH 7.4 Preservative 15mM Sodium Azide Storage Store at +4°C short term (1-2 weeks). Aliquot and store at -20°C or -80°C. Avoid repeated freeze 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved / thaw cycles. -

Regulation of Apoptosis by P53-Inducible Transmembrane Protein Containing Sushi Domain
1193-1200.qxd 24/9/2010 08:07 Ì ™ÂÏ›‰·1193 ONCOLOGY REPORTS 24: 1193-1200, 2010 Regulation of apoptosis by p53-inducible transmembrane protein containing sushi domain HONGYAN CUI, HIROKI KAMINO, YASUYUKI NAKAMURA, NORIAKI KITAMURA, TAKAFUMI MIYAMOTO, DAISUKE SHINOGI, OLGA GODA, HIROFUMI ARAKARA and MANABU FUTAMURA Cancer Medicine and Biophysics Division, National Cancer Center Research Institute, 5-1-1 Tsukiji, Chuo-ku, Tokyo 104-0045, Japan Received January 14, 2010; Accepted March 30, 2010 DOI: 10.3892/or_00000972 Abstract. The tumor suppressor p53 is a transcription factor repair, apoptosis, and anti-angiogenesis (1,2). The p21/waf1 that induces the transcription of various target genes in gene is considered to be one of the most important p53 target response to DNA damage and it protects the cells from genes because it is essential for p53-dependent cell cycle malignant transformation. In this study, we performed cDNA arrest at G1. p53R2, which supplies nucleotides for DNA microarray analysis and found that the transmembrane protein synthesis, facilitates the repair of DNA damage. Several containing sushi domain (TMPS) gene, which encodes a mitochondrial proteins including BAX, Noxa, and p53- putative type I transmembrane protein, is a novel p53-target regulated apoptosis-inducing protein 1 (p53AIP1) contribute gene. TMPS contains a sushi domain in the extracellular to the release of cytochrome c from mitochondria. Other region, which is associated with protein-protein interaction. proteins such as Fas/ApoI and unc-5 homolog B (UNC5B) TMPS expression is induced by endogenous p53 under geno- are also associated with apoptosis. Brain-specific angio- toxic stress in several cancer cell lines. -

Role and Regulation of the P53-Homolog P73 in the Transformation of Normal Human Fibroblasts
Role and regulation of the p53-homolog p73 in the transformation of normal human fibroblasts Dissertation zur Erlangung des naturwissenschaftlichen Doktorgrades der Bayerischen Julius-Maximilians-Universität Würzburg vorgelegt von Lars Hofmann aus Aschaffenburg Würzburg 2007 Eingereicht am Mitglieder der Promotionskommission: Vorsitzender: Prof. Dr. Dr. Martin J. Müller Gutachter: Prof. Dr. Michael P. Schön Gutachter : Prof. Dr. Georg Krohne Tag des Promotionskolloquiums: Doktorurkunde ausgehändigt am Erklärung Hiermit erkläre ich, dass ich die vorliegende Arbeit selbständig angefertigt und keine anderen als die angegebenen Hilfsmittel und Quellen verwendet habe. Diese Arbeit wurde weder in gleicher noch in ähnlicher Form in einem anderen Prüfungsverfahren vorgelegt. Ich habe früher, außer den mit dem Zulassungsgesuch urkundlichen Graden, keine weiteren akademischen Grade erworben und zu erwerben gesucht. Würzburg, Lars Hofmann Content SUMMARY ................................................................................................................ IV ZUSAMMENFASSUNG ............................................................................................. V 1. INTRODUCTION ................................................................................................. 1 1.1. Molecular basics of cancer .......................................................................................... 1 1.2. Early research on tumorigenesis ................................................................................. 3 1.3. Developing -

Mutational Profile and Prognostic Significance of TP53 in Diffuse Large
LYMPHOID NEOPLASIA Mutational profile and prognostic significance of TP53 in diffuse large B-cell lymphoma patients treated with R-CHOP: report from an International DLBCL Rituximab-CHOP Consortium Program Study Zijun Y. Xu-Monette,1 Lin Wu,2 Carlo Visco,3 Yu Chuan Tai,2 Alexander Tzankov,4 Wei-min Liu,2 Santiago Montes-Moreno,5 Karen Dybkær,6 April Chiu,7 Attilio Orazi,8 Youli Zu,9 Govind Bhagat,10 Kristy L. Richards,11 Eric D. Hsi,12 X. Frank Zhao,13 William W. L. Choi,14 Xiaoying Zhao,15 J. Han van Krieken,16 Qin Huang,17 Jooryung Huh,18 Weiyun Ai,19 Maurilio Ponzoni,20 Andre´s J. M. Ferreri,20 Fan Zhou,21 Brad S. Kahl,22 Jane N. Winter,23 Wei Xu,24 Jianyong Li,24 Ronald S. Go,25 Yong Li,26 Miguel A. Piris,5 Michael B. Møller,27 Roberto N. Miranda,1 Lynne V. Abruzzo,1 L. Jeffrey Medeiros,1 and Ken H. Young1 1Department of Hematopathology, The University of Texas MD Anderson Cancer Center, Houston, TX; 2Roche Molecular Systems Inc, Pleasanton, CA; 3San Bortolo Hospital, Vicenza, Italy; 4University Hospital, Basel, Switzerland; 5Hospital Universitario Marques de Valdecilla, Santander, Spain; 6Aalborg Hospital, Aarhus University Hospital, Aalborg, Denmark; 7Memorial Sloan-Kettering Cancer Center, New York, NY; 8Weill Medical College of Cornell University, New York, NY; 9The Methodist Hospital, Houston, TX; 10Columbia University Medical Center and New York Presbyterian Hospital, New York, NY; 11University of North Carolina School of Medicine, Chapel Hill, NC; 12Cleveland Clinic, Cleveland, OH; 13University of Maryland School of Medicine, Baltimore, MD; 14University of Hong Kong Li Ka Shing Faculty of Medicine, Hong Kong, China; 15Zhejiang University School of Medicine, Second University Hospital, Hangzhou, China; 16Radboud University Nijmegen Medical Centre, Nijmegen, Netherlands; 17City of Hope National Medical Center, Duarte, CA; 18Asan Medical Center, Ulsan University College of Medicine, Seoul, Korea; 19University of California-San Francisco School of Medicine, San Francisco, CA; 20San Raffaele H. -

P53aip1 Regulates the Mitochondrial Apoptotic Pathway1
[CANCER RESEARCH 62, 2883–2889, May 15, 2002] p53AIP1 Regulates the Mitochondrial Apoptotic Pathway1 Koichi Matsuda, Koji Yoshida, Yoichi Taya, Kozo Nakamura, Yusuke Nakamura,2 and Hirofumi Arakawa Human Genome Center, Institute of Medical Science, University of Tokyo, Minato-ku, Tokyo 108-8639 [K. M., K. Y., Y. N., H. A.], and Department of Orthopedic Surgery, Faculty of Medicine, University of Tokyo, Bunkyo-ku, Tokyo 113-0033 [K. M., K. N.], and National Cancer Center Research Institute, Chuo-ku, Tokyo 104-0045 [Y.T.], Japan ABSTRACT family have been reported as anti- or proapoptotic players; all of them possess at least one of the four domains. We identified recently the p53AIP1 gene, a novel p53 target that Although p53-dependent apoptosis is thought to be the most im- mediates p53-dependent apoptosis. In the experiments reported here, portant feature of tumor suppression by p53, a large part of that ectopic expression of p53AIP1 induced down-regulation of mitochondrial ⌬⌿m and release of cytochrome c from mitochondria in human cells. mechanism remains to be explained. Several target genes have been Immunoprecipitation and immunostaining experiments indicated interac- isolated as attractive candidates for p53-dependent apoptosis, includ- tion between p53AIP1 and bcl-2 proteins at mitochondria. Overexpression ing bax (23), PIG3 (24, 25), Killer/DR5 (26), Fas (27, 28), Noxa (29), of bcl-2 blocked the down-regulation of mitochondrial ⌬⌿m and the PERP (30), and PUMA (31, 32). Bax, Noxa, and PUMA are mito- proapoptotic activity of p53AIP1. Our results implicate p53AIP1 as a chondrial proteins and members of the bcl-2 family, because they pivotal mediator of the p53-dependent mitochondrial apoptotic pathway. -

The P53mh Algorithm and Its Application in Detecting P53-Responsive Genes
The p53MH algorithm and its application in detecting p53-responsive genes J. Hoh*†‡, S. Jin§†, T. Parrado*, J. Edington*, A. J. Levine§, and J. Ott* *Laboratories of Statistical Genetics and §Cancer Biology of The Rockefeller University, 1230 York Avenue, New York, NY 10021 Contributed by A. J. Levine, May 6, 2002 A computer algorithm, p53MH, was developed, which identifies overall binding likelihood is needed for a given gene of arbitrary putative p53 transcription factor DNA-binding sites on a genome- size. Three features have been implemented in an algorithm to wide scale with high power and versatility. With the sequences meet the above requirements: binding propensity plots, weighted from the human and mouse genomes, putative p53 DNA-binding scores, and statistical significance for most likely binding sites. elements were identified in a scan of 2,583 human genes and 1,713 This computer algorithm has been used to identify putative mouse orthologs based on the experimental data of el-Deiry et al. binding elements on a genomewide scale. The algorithm, [el-Deiry, W. S., Kern, S. E., Pietenpol, J. A., Kinzler, K. W. & p53MH, uses an optimal scoring system as an indication of the Vogelstein, B. (1992) Nat. Genet. 1, 45–49] and Funk et al. [Funk, percent similarity to the consensus. It can simultaneously screen W. D., Pak, D. T., Karas, R. H., Wright, W. E. & Shay, J. W. (1992) Mol. thousands of genes for degenerate consensus sequences in the Cell. Biol. 12, 2866–2871] (http:͞͞linkage.rockefeller.edu͞p53). The course of only a few minutes. With this, based on the available p53 DNA-binding motif consists of a 10-bp palindrome and most annotated human sequence databases, a White Page-like direc- commonly a second related palindrome linked by a spacer region. -

Addressing the Issue of Missing Heritability: the Importance of Apoptosis in Hereditary Breast and Ovarian Cancer and Functional Assessment of Tp53i3-S252*
Wayne State University Wayne State University Dissertations January 2020 Addressing The Issue Of Missing Heritability: The Importance Of Apoptosis In Hereditary Breast And Ovarian Cancer And Functional Assessment Of Tp53i3-S252* Sophia Chaudhry Wayne State University Follow this and additional works at: https://digitalcommons.wayne.edu/oa_dissertations Part of the Genetics Commons Recommended Citation Chaudhry, Sophia, "Addressing The Issue Of Missing Heritability: The Importance Of Apoptosis In Hereditary Breast And Ovarian Cancer And Functional Assessment Of Tp53i3-S252*" (2020). Wayne State University Dissertations. 2382. https://digitalcommons.wayne.edu/oa_dissertations/2382 This Open Access Dissertation is brought to you for free and open access by DigitalCommons@WayneState. It has been accepted for inclusion in Wayne State University Dissertations by an authorized administrator of DigitalCommons@WayneState. ADDRESSING THE ISSUE OF MISSING HERITABILITY: THE IMPORTANCE OF APOPTOSIS IN HEREDITARY BREAST AND OVARIAN CANCER AND FUNCTIONAL ASSESSMENT OF TP53I3-S252* by SOPHIA RASUL CHAUDHRY DISSERTATION Submitted to the Graduate School of Wayne State University, Detroit, Michigan in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY 2020 MAJOR: MOLECULAR GENETICS AND GENOMICS Approved By: ____________________________________ Advisor Date ____________________________________ ____________________________________ ____________________________________ DEDICATION I dedicate this work to my parents, my siblings and my nieces and nephew. All have been a positive force and motivation in becoming the scientist I am today. ii ACKNOWLEDGMENTS There are many people who deserve recognition for helping me complete my doctoral work. One of the most challenging parts of my time as a graduate student finding the right lab. I was very lucky to be accepted into the lab headed by Dr. -
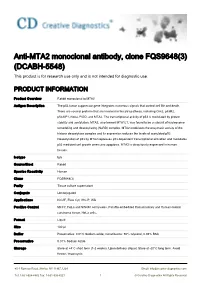
Anti-MTA2 Monoclonal Antibody, Clone FQS9648(3) (DCABH-5548) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-MTA2 monoclonal antibody, clone FQS9648(3) (DCABH-5548) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Product Overview Rabbit monoclonal to MTA2 Antigen Description The p53 tumor suppressor gene integrates numerous signals that control cell life and death. There are several proteins that are involved in the p53 pathway, including Chk2, p53R2, p53AIP1, Noxa, PIDD, and MTA2. The transcriptional activity of p53 is modulated by protein stability and acetylation. MTA2, also termed MTA1L1, was found to be a subunit of nucleosome remodeling and deacetylating (NuRD) complex. MTA2 modulates the enzymatic activity of the histone deacetylase complex and its expression reduces the levels of acetylated p53. Deacetylation of p53 by MTA2 represses p53 dependent transcriptional activation and modulates p53 mediated cell growth arrest and apoptosis. MTA2 is ubiquitously expressed in human tissues. Isotype IgG Source/Host Rabbit Species Reactivity Human Clone FQS9648(3) Purity Tissue culture supernatant Conjugate Unconjugated Applications ICC/IF, Flow Cyt, IHC-P, WB Positive Control MCF7, HeLa and SW480 cell lysates. Paraffin-embedded Human kidney and Human colonic carcinoma tissue. HeLa cells. Format Liquid Size 100 μl Buffer Preservative: 0.01% Sodium azide; Constituents: 50% Glycerol, 0.05% BSA Preservative 0.01% Sodium Azide Storage Store at +4°C short term (1-2 weeks). Upon delivery aliquot. Store at -20°C long term. Avoid freeze / thaw cycle. 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved Ship Shipped at 4°C. -

P53/P73 Protein Network in Colorectal Cancer and Other Human Malignancies
cancers Review p53/p73 Protein Network in Colorectal Cancer and Other Human Malignancies Andela¯ Horvat †, Ana Tadijan † , Ignacija Vlaši´c † and Neda Slade * Laboratory for Protein Dynamics, Division of Molecular Medicine, Ruder¯ Boškovi´cInstitute, Bijeniˇcka54, 10000 Zagreb, Croatia; [email protected] (A.H.); [email protected] (A.T.); [email protected] (I.V.) * Correspondence: [email protected] † Contributed equally. Simple Summary: The p53 family of proteins comprises p53, p63, and p73, which share high structural and functional similarity. The two distinct promoters of each locus, the alternative splicing, and the alternative translation initiation sites enable the generation of numerous isoforms with different protein-interacting domains and distinct activities. The co-expressed p53/p73 isoforms have significant but distinct roles in carcinogenesis. Their activity is frequently impaired in human tumors including colorectal carcinoma due to dysregulated expression and a dominant-negative effect accomplished by some isoforms and p53 mutants. The interactions between isoforms are particularly important to understand the onset of tumor formation, progression, and therapeutic response. The understanding of the p53/p73 network can contribute to the development of new targeted therapies. Abstract: The p53 tumor suppressor protein is crucial for cell growth control and the maintenance of genomic stability. Later discovered, p63 and p73 share structural and functional similarity with p53. To understand the p53 pathways more profoundly, all family members should be considered. Citation: Horvat, A.; Tadijan, A.; Each family member possesses two promoters and alternative translation initiation sites, and they Vlaši´c,I.; Slade, N. p53/p73 Protein undergo alternative splicing, generating multiple isoforms. -

Etude De 2 Gènes Cibles De La Protéine P53 : Siah (Seven in Absentia Human Homologue) Et Tsap6 (Tumor Suppressor Activated Pathway 6) Séverine Beaucourt
Etude de 2 gènes cibles de la protéine P53 : siah (seven in absentia human homologue) et tsap6 (tumor suppressor activated pathway 6) Séverine Beaucourt To cite this version: Séverine Beaucourt. Etude de 2 gènes cibles de la protéine P53 : siah (seven in absentia human homologue) et tsap6 (tumor suppressor activated pathway 6). Biologie cellulaire. Université Paris Sud - Paris XI, 2005. Français. tel-00157749 HAL Id: tel-00157749 https://tel.archives-ouvertes.fr/tel-00157749 Submitted on 27 Jun 2007 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. "I am satisfied with the mystery of life's eternity and with the awareness of--and glimpse into--the marvelous construction of the existing world together with the steadfast determination to comprehend a portion, be it ever so tiny, of the reason that manifests itself in nature. This is the basis of cosmic religiosity, and it appears to me that the most important function of art and science is to awaken this feeling among the receptive and keep it alive." Albert Einstein Avant-propos Je souhaiterais avant toute chose remercier Adam Telerman et Robert Amson pour m'avoir fait confiance tout au long de ces années, et surtout à mon arrivée au laboratoire lorsque je cherchais un stage qui devait marquer la "fin de mes études". -

P53aip1 Regulates the Mitochondrial Apoptotic Pathway1
[CANCER RESEARCH 62, 2883–2889, May 15, 2002] p53AIP1 Regulates the Mitochondrial Apoptotic Pathway1 Koichi Matsuda, Koji Yoshida, Yoichi Taya, Kozo Nakamura, Yusuke Nakamura,2 and Hirofumi Arakawa Human Genome Center, Institute of Medical Science, University of Tokyo, Minato-ku, Tokyo 108-8639 [K. M., K. Y., Y. N., H. A.], and Department of Orthopedic Surgery, Faculty of Medicine, University of Tokyo, Bunkyo-ku, Tokyo 113-0033 [K. M., K. N.], and National Cancer Center Research Institute, Chuo-ku, Tokyo 104-0045 [Y.T.], Japan ABSTRACT family have been reported as anti- or proapoptotic players; all of them possess at least one of the four domains. We identified recently the p53AIP1 gene, a novel p53 target that Although p53-dependent apoptosis is thought to be the most im- mediates p53-dependent apoptosis. In the experiments reported here, portant feature of tumor suppression by p53, a large part of that ectopic expression of p53AIP1 induced down-regulation of mitochondrial ⌬⌿m and release of cytochrome c from mitochondria in human cells. mechanism remains to be explained. Several target genes have been Immunoprecipitation and immunostaining experiments indicated interac- isolated as attractive candidates for p53-dependent apoptosis, includ- tion between p53AIP1 and bcl-2 proteins at mitochondria. Overexpression ing bax (23), PIG3 (24, 25), Killer/DR5 (26), Fas (27, 28), Noxa (29), of bcl-2 blocked the down-regulation of mitochondrial ⌬⌿m and the PERP (30), and PUMA (31, 32). Bax, Noxa, and PUMA are mito- proapoptotic activity of p53AIP1. Our results implicate p53AIP1 as a chondrial proteins and members of the bcl-2 family, because they pivotal mediator of the p53-dependent mitochondrial apoptotic pathway. -

Stress Via P53 Pathway Causes Apoptosis by Mitochondrial Noxa
Oncogene (2008) 27, 741–754 & 2008 Nature Publishing Group All rights reserved 0950-9232/08 $30.00 www.nature.com/onc ORIGINAL ARTICLE Stress via p53 pathway causes apoptosis by mitochondrialNoxa upregulation in doxorubicin-treated neuroblastoma cells K Kurata1, R Yanagisawa1, M Ohira2, M Kitagawa3, A Nakagawara2 and T Kamijo1,2 1Department of Pediatrics, Shinshu University School of Medicine, Matsumoto, Nagano, Japan; 2Division of Biochemistry, Chiba Cancer Center Research Institute, Chuoh-ku, Chiba, Japan and 3Department of Biochemistry, Hamamatsu University School of Medicine, Hamamatsu, Shizuoka, Japan In this study, we employed a panel of cell lines to determine which survival has been improved by recent therapies, whether p53-dependent cell death in neuroblastoma (NB) high-risk NB is still one of the most difficult tumors to cells is caused by apoptotic cellular function, and we cure, with only 30% long-term survival despite intensive further studied the molecular mechanism of apoptosis multimodal therapy. New treatments and a better induced via the p53-dependent pathway. We obtained understanding of drug resistance mechanisms are evidence that a type of p53-dependent stress, doxorubicin required for the improvement of the survival rate. A (Doxo) administration, causes accumulation of p53 in the noteworthy finding of NB research is that mutations of nucleus of NB cells and phosphorylation of several serine p53 tumor suppressor have been reported in less than residues in both Doxo-sensitive and -resistant cell lines. 2% of NBs out of 340 tested (Tweddle et al., 2001). Upregulation of p53-downstream molecules in cells and Instead of mutation, cytoplasmic sequestration of p53 upregulation of Noxa in the mitochondrial fraction were has been proposed as an alternative mechanism of observed only in Doxo-sensitive NB cells.