Guide to the Canberra Hospital
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Guide to Patient Support and Regional Cancer Services
Guide to Patient Support and Regional Cancer Services Information for cancer patients, carers and families in the ACT and surrounding region Accessibility The ACT Government is committed to making its information, services, events and venues, accessible to as many people as possible. • If you have difficulty reading a standard printed document and would like to receive this publication in an alternative format—such as large print or audio—please telephone 13 2281 or email [email protected]. • If English is not your first language and you require the translating and interpreting service—please telephone 131 450. • If you are deaf or hearing impaired and require the TTY typewriter service—please telephone (02) 13 3677, then ask for 13 2281. • Speak and listen users—phone 1300 555 727 then ask for 13 2281. • Internet Relay Users—connect to the NRS, then ask for 13 2281. © Australian Capital Territory, Canberra, October 2011 This work is copyright. Apart from any use as permitted under the Copyright Act 1968, no part may be reproduced by any process without written permission from the Territory Records Office, Community and Infrastructure Services, Territory and Municipal Services, ACT Government, GPO Box 158, Canberra City ACT 2601. Enquiries about this publication should be directed to ACT Government Health Directorate, Communications and Marketing Unit, GPO Box 825 Canberra City ACT 2601 or email: [email protected] www.health.act.gov.au | www.act.gov.au Enquiries: Canberra 13ACT1 or 132281 Publication No 11/0815 Contents Acknowledgments -
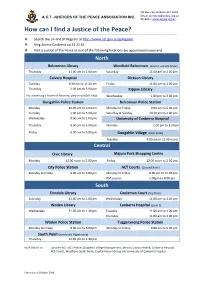
How Can I Find a JP
PO Box 766, Dickson ACT 2602 A.C.T. JUSTICES OF THE PEACE ASSOCIATION INC. Email: [email protected] Website: www.actjpa.org.au How can I find a Justice of the Peace? ❖ Search the on-line JP Register at http://www.act.gov.au/jpregister ❖ Ring Access Canberra on 13 22 81 ❖ Visit a Justice of the Peace at one of the following locations (no appointment necessary) North Belconnen Library Westfield Belconnen (level 3, outside Myer) Thursday 11.00 am to 1.00 pm Saturday 11.00 am to 1.00 pm Calvary Hospital Dickson Library Tuesday 9.30 am to 11.30 am Friday 11.00 am to 1.00 pm Thursday 1.00 pm to 3.00 pm Kippax Library For witnessing a Power of Attorney, please call 6201 6646. Wednesday 1.00 pm to 3.00 pm Gungahlin Police Station Belconnen Police Station Monday 10.00 am to 2.00 pm Monday to Friday 9.00 am to 5.00 pm Tuesday 1.00 pm to 5.00 pm Saturday & Sunday 10.30 am to 2.00 pm Wednesday 9.00 am to 1.00 pm University of Canberra Hospital Thursday 9.00 am to 5.00 pm Monday 1.00 pm to 3.00 pm Friday 9.00 am to 5.00 pm Gungahlin Village (near Coles) Tuesday 9.00 am to 12.00 noon Central Civic Library Majura Park Shopping Centre Monday 12.00 noon to 2.00 pm Friday 12.00 noon to 2.00 pm City Police Station ACT Courts (Ground floor) Monday to Friday 9.00 am to 5.00 pm Monday to Friday 9.30 am to 12.30 pm PM session 1.00pm to 4.00 pm . -

Clinical Placement Office (CPO) [email protected] Level 3, 2-6 Bowes Street, Phillip, ACT 2606
Clinical Placement Office (CPO) [email protected] Level 3, 2-6 Bowes Street, Phillip, ACT 2606 Nursing & Midwifery Ward Contact List Canberra Health Services Switchboard – (02) 5124 2222 Students should contact either the Clinical Nurse Consultant (CNC) or Clinical Development Nurse (CDN) on the relevant telephone numbers below. Work area Contact number Notes Medical & Surgery Ward 10A – General surgery 512 42562 / 42236 Ward 9A - Gastroenterology 512 42337 / 42338 Ward 9B – Neurosurgery 512 42631 / 42632 Ward 8A – Haemodialysis 512 43362 / 43363 Ward 7B – General Medicine Unit (GMU) 512 42449 / 42275 Ward 7A – Stroke/Neurology 512 42535 / 42857 Ward 6A – Medical Cardiothoracic/Respiratory/ 512 42731 / 42732 Endocrinology/Rheumatology Ward 6B - Surgical Cardiothoracic/Urology/Vascular 512 42751 / 42653 Ward 5A - Orthopaedics 512 47905 / 47907 Ward 5B – General surgery/ENT 512 47918 / 47919 Ward 4B – Renal Medicine 512 42949 / 42938 Aged Care Ward 11A – Acute care elderly 512 42773 / 42770 Ward 11B – Sub acute aged care 512 42434 / 42435 Canberra Region Cancer Centre (CRCC) Ward 14A – Haematology Ward 512 42233 / 42351 Ward 8B* – Medical Oncology Ward 512 48611 / 48613 *Previously on 14B Canberra Region Cancer Centre (CRCC) 512 48444 Bldg 19 Switchboard Medical Oncology Day Unit 512 48457 Bldg 19, Level 4 Haematology Day Unit 512 44275 Bldg 19, Level 4 Immunology Day Unit 512 48457 Bldg 19, Level 4 Cancer Specialist Nurses 0412 502 010 Bldg 19, Level 5 CRCC Outpatient Department (OPD) 512 43510 Bldg 19, Level 2 Rapid Assessment Unit (RAU) -

List of Accredited Chest Clinics (By State)
ACT Health Clinical Placement Office 2016 List of Accredited Chest clinics (By State) ACT Canberra Hospital TB Services Department of Contact: 02 6244 2066/ 02 6244 2702 Thoracic Medicine The Canberra Hospital PO Box 11 Woden ACT 2606 New South Wales Central Coast Local Health District Gosford Hospital Contact: TB Prevention & Control Service (Chest Clinic) Appt: 4320 3388 PO Box 361 Gosford NSW 2250 Only Mon 8.30-3; Tues & Fri 8.30-4 Illawarra and Shoalhaven LHD The Wollongong Hospital Contact: 4253 4138 Department of Respiratory Medicine Crown Street Wollongong NSW 2500 Nepean Blue Mountains Local Health District Nepean Hospital Contact: 4734 2536 Chest Clinic Outpatients Department PO Box 63 Penrith NSW 2751 Northern Sydney Local Health District Hornsby Ku-ring-gai Hospital Contact: 9477 9318 Palmerston Road Hornsby NSW 2077 New Royal North Shore Hospital Contact: 9926 7905 Chest Clinic Level 8, Dept. of Respiratory Medicine St Leonards NSW 2065 Manly District Hospital Contact: 9976 9542 Chest Clinic Manly NSW 2095 South Eastern Sydney LHD - Northern Network Prince of Wales Hospital Contact: 9382 4643/ 9382 4672 Department of Respiratory Medicine Level 2 Dickinson Building Barker Street Randwick NSW 2031 Sydney Hospital Contact: 9382 7535 Chest Clinic Macquarie Street Sydney NSW 2000 St. Vincent's Hospital Contact: 8382 3150 Heart-Lung Ambulatory Care Level 4, Xavier Building 390 Victoria Street Darlinghurst NSW 2010 South Eastern Sydney LHD - Central Network ACT Health Clinical Placement Office 2016 St George Hospital Contact: 9113 -

Canberra College Students Qualifying for This Honour
Principal’s Report - AUGUST 2015 I I welcome you all back to the business end of the year, particularly for our Year 12 students. I trust that all students returned rested and revitalised for the semester ahead. At our first week assembly I talked about the importance of feedback as it has two purposes; summative performance and also suggestions for improving performance. Last semester every student received a formal written summative report. This complements the feedback that students received throughout the term through the variety of learning and assessment activities as well as performance in the exams. Seeking and giving feedback also improves the performance of both teacher and student. Parent, teacher and student feedback along with performance data for the college collected over the past 4 years has now been analysed by an external panel as part of the review and validation process. The college validation report will be published before the end of term 3 and will contain a series of commendations and recommendations which will inform our planning for the next 4 years. I thank the students, staff and parents who contributed to the panels deliberations. In the next few weeks student, teachers and parents will be asked to complete the annual online school satisfaction survey. This is an important guide for us in our planning for whole college improvement. Please make the time complete this survey as we value your input and suggestions. Our staff and students continue to excel in a variety of areas. I acknowledge and congratulate; Jim Phillips who has won a promotion to Executive Teacher Science and PE at Lake Tuggeranong College. -

Integrating the Canberra Hospital ED with After Hours Primary Health Care Services – Final Report
Integrating the Canberra Hospital ED with after hours primary health care services – Final Report Capital Health Network 14 May 2018 Copyright & confidentiality: No part of this publication may be reproduced, stored in a retrieval system, translated, transcribed or transmitted in any form, or by any means manual, electric, electronic, electromagnetic, mechanical, chemical, optical, or otherwise, without the prior explicit written permission of Capital Health Network. © Nous Group Nous Group | Integrating the Canberra Hospital ED with after hours primary health care services – Final Report | 14 May 2018 | i | Contents 1 Executive Summary ...................................................................................................................................................................... 2 2 Introduction ..................................................................................................................................................................................... 5 3 Business Case .................................................................................................................................................................................. 8 4 Proposed interventions ........................................................................................................................................................... 13 5 Recommended interventions ............................................................................................................................................... -

June 2019 Newsletter
JUNE 2019 NEWSLETTER Principal’s Update Semester 1 at Canberra College has been a very positive time as the engagement of the college with the community continues to impress. Evidence of this includes the magnificent Woden Square Artspace Photography project through to the academic prestige of the ANU Maths Competition Runner-up result. Reflecting a tradition of highly capable student mathematicians, the college foyer trophy cabinet contains many trophies from the ANU Maths Competition, Including the overall winner in 2017. Final assessments for approximately 350 classes have been completed and student report writing has commenced. Please note that reports will be emailed to parents/carers and students on Friday 5 July. It was at the Board meeting this week that a decision was supported to also include all students in the email distribution of their reports. Previously, students would carry printed reports home in their schoolbags and deliver them to parents/carers. This practice also acknowledges that reports are written to students and contain feedback they should reference to continuously improve their performance. Student reports are valuable in reviewing student learning and pathways, and we encourage all parents and carers to discuss the reports at home. On the topic of feedback, all students are encouraged to complete a short online survey for each unit of study they undertake. This practice is highly valued by teachers as a way they too can use student feedback to reflect on their craft as educators and seek ways to strengthen their pedagogy and areas of practice. During this time College teachers are also required to prepare their Board of Senior Secondary Studies (BSSS) Unit Moderation Portfolios for submission this semester. -

Immunohistochemical Study of Intimal Microvessels in Coronary Atherosclerosis
American Journal ofPathology, Vol. 143, No. 1, July 1993 Copyright X American Societyfor Investigative Pathology Immunohistochemical Study of Intimal Microvessels in Coronary Atherosclerosis Yixia Zhang,* Walter J. Cliff,* Gutta 1. Schoefl,* over 1000 hearts, concluded that nobody with ab- and Grace Higginst normal vascularization of the coronary artery wall was From the Clinical Science Division,* John Curtin School of free from the risk of death from coronary artery dis- Medical Research, The Australian National University, ease. However, some workers consider that vessels Canberra, and the School ofPathology,t University ofNew invading the coronary intima are of no signifi- South Wales, Sydney, Australia cance12,13 and are a function of intimal thickness and not of atherosclerosis.14 Those who emphasize the importance of intimal Two hundred ninety-nine human coronary artery vascularization propose that the microvessels may paraffin-embedded tissue blocks were examined play two roles: one, of providing blood components to for intimal microvessel invasion by probing for "nourish" the growing plaques,2'10'15 and the other, of factor VIII-associated antigen with indirect im- causing intimal hemorrhages by rupturing. Repeated munofluorescence and high resolution confocal intimal hemorrhages may eventually lead to coronary microscopy. The results obtained confirm that in- artery thrombosis.11 As to the first hypothesis, no di- timal microvessels originate in the adventitia and rect evidence of plasma components leaking from in- show that the richness ofintimal microvessels is timal microvessels to nourish atherosclerotic plaques strongly positively correlated with intimal thick- has yet been obtained but newly formed vessels are ness and negatively correlated with relative lu- known to be highly permeable.16 In addition, newly men size. -

Queanbeyan Agency Network Meeting (Quang) Meeting Minutes – October 2019
Queanbeyan Agency Network Meeting (QuANG) Meeting Minutes – October 2019 Date: 16th October 2019 Time: 11.30am to 1.30pm Venue: Queanbeyan Library Activity Room Facilitators: Terry Campese- & Rebekah De Jongh- QPRC Team Leader- Family Day Care QPRC Program coordinator-Community A forum where community organisations and government services can meet to explore opportunities, connect with Meeting Objective: each other and work together to grow with our community. Kyla Harvey- QPRC Community Vivienne Cox- Communities and Helen Ford, Anglicare Gambling Help Development Officer Justice Counselling Service Peter Gilbert- NSW Sexual Health, Linda Bruce- Help Centre Psychology Samantha Remmers- Googong Apologies: Jae Lear- Pathways Facilitator SRBEC Josef Garrington – ACON Community Community Development manager Nat Oliver- YCC/Community Engagement Health Promotion Officer Guest Speaker/s Organisation Update Elyse Cain– NCOSS Advocacy Manager The NSW Council of Social Service (NCOSS) works with and for people experiencing poverty and disadvantage in NSW to make Phone Number: (02) 8960 7912 positive change in our communities. E-Mail Address: [email protected] 1 Queanbeyan Agency Network Meeting (QuANG) Meeting Minutes – October 2019 As the peak body for health and community services in NSW for over 80 years we support the sector to deliver crucial services that make a difference. We work directly with communities to identify the challenges they face and solutions that will allow them to overcome those challenges. Through collaboration with communities, services and across government, the private sector and other civil society organisations we work to see these solutions become a reality. NCOSS has a Regional Advisory group. If you are interested in participating in this group or any other information, please contact Elyse. -

SNFO 45371 Snow Foundation Timeline AW.Indd
“I’m very proud to say that, over the last 25 years, the Foundation THE SNOW FOUNDATION has donated $18.4 million to 235 organisations and more than 200 individuals, many of whom would have gone without basic equipment or therapy if it wasn’t for our help” Terry Snow, Founder and Chairman | Celebrating 25 Years Twenty-five years ago my brother George and I committed $1 million to the Canberra community to establish The Snow Foundation. As long-term local Canberrans we wanted to give something to the city we love. But more than that, we strongly believe that when you see someone struggling you offer a helping hand. This is just one of the family values that guided The Snow Foundation in the beginning and continues to underpin our work. Initially, we supported individuals who slipped through A significant increase in our corpus gave us greater the cracks or had fallen on hard times – either through capacity to deepen our support into the local region and addiction or misfortune. It was early days for the extend beyond Canberra. We grew our giving significantly Foundation and these gifts were often ad hoc in nature. from $100,000 to $1 million and now give $1.7 million I deliberately chose to maintain a low profile to the annually. Importantly the family has grown the corpus to Foundation’s giving. $39 million and we aim to continue this trend. I soon connected with some well-known charities, We have developed partnerships and collaborations such as The Smith Family, Barnardos, Cancer Council with community groups, philanthropic organisations ACT and St John’s Care. -

Nsw Health Medical Retrieval - Helicopter Services in the Southern Region for the Ambulance Service of Nsw
Toll - Southern Region - DOV No 3 - Attachment 1 Redacted Contract - Execution Version (ACW:LW) CONTRACT NO HAC 13/63 BETWEEN THE HEALTH ADMINISTRATION CORPORATION AND TOLL HELICOPTERS (NSW) PTY LTD FOR NSW HEALTH MEDICAL RETRIEVAL - HELICOPTER SERVICES IN THE SOUTHERN REGION FOR THE AMBULANCE SERVICE OF NSW Clayton Utz Lawyers Level 10, 2 Phillip Law Street, Canberra ACT 2600 Australia GPO Box 9806 Canberra ACT 2601 T +61 2 6279 4008 F +61 2 6279 4099 (ACW:LW:KK) www.claytonutz.com Our reference 130/13647/80149353 1 L\339002597.1 Toll - Southern Region - DOV No 3 - Attachment 1 Redacted Contract - Execution Version (ACW:LW) CONTENTS 1. Definitions and Interpretation ................................................................................................... 4 2. Term ........................................................................................................................................... 23 3. Security ..................................................................................................................................... 25 4. Readiness for Handover .......................................................................................................... 26 4A Bankstown Base ................................................................................................................... 29 4B Aircraft Replacement ............................................................................................................ 29 5. Scope of Contract ................................................................................................................... -

April 2019 Newsletter
APRIL 2019 NEWSLETTER Principal’s Update As the Canberra College Principal this term I have had the privilege to work with a very experienced and capable staff. With our staff we have commenced the year with a clear focus on supporting the learning for all students. In a college of over 1100 students this is an exciting and rewarding challenge. As a college with a strong tradition of inclusion and success, every day we see the strength in this commitment come through the endeavour and engagement of students in their classes, and this newsletter shares with you many examples of this. As we commence another year it is important to advise our community we are guided by a focus on learning, supported by the Canberra College Strategic Plan which has three key priorities: 1. Enhance the quality of teaching and learning through systematic and evidence-based processes to improve delivery of educational services and outcomes for all students. 2. Review and develop a sustainable school resources model which supports diversity of learning pathways utilising contemporary learning environments. 3. Develop a college culture that values and reinforces wellbeing, strengthens community connectedness to support student and staff performance. Our 2019 College Board meets on Wednesday 10 April where the 2019 Annual Action Plan will be approved. At this meeting the Board will also represent the college community in a consultation about the proposed development plans for the land (previously Pitch’n’Putt) adjacent the college campus. We shall endeavour to share details in future communications and certainly advocate to preserve the integrity of the public College as an education provider to late adolescents in the Woden/Weston region.