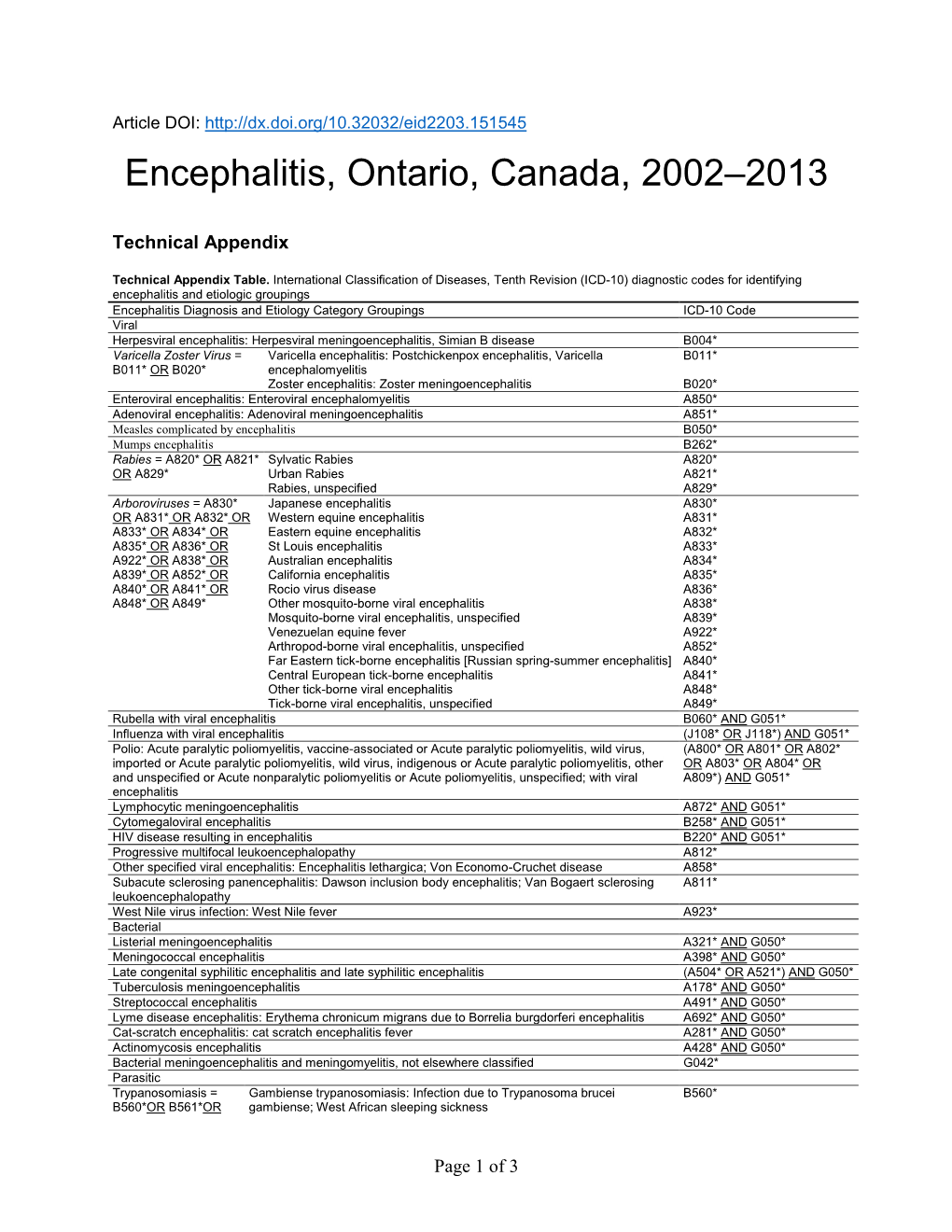
Technical Appendix
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chasing the Dragon, a Case of Leukoencephalopathy Associated with Heroin Inhalation
Chasing the dragon, a case of leukoencephalopathy associated with heroin inhalation Daniel Cho MD1, Hani Nazha MD2, Kalin Fisher BS2 Author Affiliations: 1. Charleston Area Medical Center, Charleston, West Virginia 2. West Virginia University, Morgantown, West Virginia The authors have no financial disclosures to declare and no conflicts of interest to report. Corresponding Author: Hani Nazha MD West Virginia University Morgantown, West Virginia Email: [email protected] Abstract Although rare, toxic leukoencephalopathy (TLE) associated with heroin inhalation has been reported. “Chasing the dragon” may lead to progressive spongiform degeneration of the brain and presents with a large range of neuropsychological sequelae. This case is an example of TLE in a middle-aged white male with a history of polysubstance abuse. He presented with a three week history of progressive neuropsychological symptoms, including abulia, bradyphrenia, hyperreflexia, and visual hallucinations. He was initially suspected to have progressive multifocal leukoencephalopathy, however, JCV PCR was negative. MRI showed diffuse abnormal signal in the white matter, extending into the thalami and cerebral peduncles. Brain biopsy was performed, which revealed spongiform degeneration, and a diagnosis of TLE was made. The patient was then transferred to a skilled nursing facility. Clinical suspicion based on a thorough history and clinical exam findings is paramount in recognition of heroin-associated TLE. Although rare, heroin-inhalation TLE continues to be reported. As ‘chasing the dragon’ is gaining popularity among drug users, it is important for clinicians to be able to recognize this disease process. Keywords Opioid, Addiction, Heroin, Leukoencephalopathy Introduction Toxic leukoencephalopathy (TLE) associated with heroin abuse was first described in 1982.1 “Chasing the dragon" is a method of heroin vapor inhalation in which a small amount of heroin powder is placed on aluminum foil, which is then heated by placing a match or lighter underneath. -

Viral Encephalitis: a Hard Nut to Crack
Published online: 02.10.2019 THIEME 98 ViralReview Encephalitis Article Shukla et al. Viral Encephalitis: A Hard Nut to Crack Alka Shukla1 Mayank Gangwar1 Sonam Rastogi1 Gopal Nath1 1Department of Microbiology, Viral Research and Diagnostic Address for correspondence Gopal Nath, MD, PhD, Department Laboratory, Institute of Medical Sciences, Banaras Hindu of Microbiology, Viral Research and Diagnostic Laboratory, Institute University, Varanasi, India of Medical Sciences, Banaras Hindu University, Varanasi, India (e-mail: [email protected]). Ann Natl Acad Med Sci (India) 2019;55:98–109 Abstract Viral encephalitis is inflammation of brain that manifests as neurological complication of viral infections. There are quite a good number of viruses, for example, human her- pes virus, Japanese encephalitis, and enteroviruses that can result in such a dreadful condition. Geographical location, age, gender, immune status, and climatic conditions also contribute to the establishment of this disease in an individual. Clinical signs and symptoms include fever, headache, altered level of consciousness, changed mental status, body ache, seizures, nausea, and vomiting. Effective management of this dis- ease relies on timely diagnosis that in turn depends on apt and suitable investigation Keywords techniques. Traditional investigations have thinned out these days owing to the fact ► encephalitis that advanced molecular technologies have been introduced to the diagnostic field. ► viral infection Treatment of viral encephalitis mainly involves symptomatic relieve from fever, mal- ► pathogenesis aise, myalgia along with measures to reduce viral load in the patient. This review men- ► molecular techniques tions about all the possible aspects of viral encephalitis starting from etiology to the ► management management and preventive measures that include immunization and vector control. -

ICD10 Diagnoses FY2018 AHD.Com
ICD10 Diagnoses FY2018 AHD.com A020 Salmonella enteritis A5217 General paresis B372 Candidiasis of skin and nail A040 Enteropathogenic Escherichia coli A523 Neurosyphilis, unspecified B373 Candidiasis of vulva and vagina infection A528 Late syphilis, latent B3741 Candidal cystitis and urethritis A044 Other intestinal Escherichia coli A530 Latent syphilis, unspecified as early or B3749 Other urogenital candidiasis infections late B376 Candidal endocarditis A045 Campylobacter enteritis A539 Syphilis, unspecified B377 Candidal sepsis A046 Enteritis due to Yersinia enterocolitica A599 Trichomoniasis, unspecified B3781 Candidal esophagitis A047 Enterocolitis due to Clostridium difficile A6000 Herpesviral infection of urogenital B3789 Other sites of candidiasis A048 Other specified bacterial intestinal system, unspecified B379 Candidiasis, unspecified infections A6002 Herpesviral infection of other male B380 Acute pulmonary coccidioidomycosis A049 Bacterial intestinal infection, genital organs B381 Chronic pulmonary coccidioidomycosis unspecified A630 Anogenital (venereal) warts B382 Pulmonary coccidioidomycosis, A059 Bacterial foodborne intoxication, A6920 Lyme disease, unspecified unspecified unspecified A7740 Ehrlichiosis, unspecified B387 Disseminated coccidioidomycosis A080 Rotaviral enteritis A7749 Other ehrlichiosis B389 Coccidioidomycosis, unspecified A0811 Acute gastroenteropathy due to A879 Viral meningitis, unspecified B399 Histoplasmosis, unspecified Norwalk agent A938 Other specified arthropod-borne viral B440 Invasive pulmonary -

Download the Abstract Book
1 Exploring the male-induced female reproduction of Schistosoma mansoni in a novel medium Jipeng Wang1, Rui Chen1, James Collins1 1) UT Southwestern Medical Center. Schistosomiasis is a neglected tropical disease caused by schistosome parasites that infect over 200 million people. The prodigious egg output of these parasites is the sole driver of pathology due to infection. Female schistosomes rely on continuous pairing with male worms to fuel the maturation of their reproductive organs, yet our understanding of their sexual reproduction is limited because egg production is not sustained for more than a few days in vitro. Here, we explore the process of male-stimulated female maturation in our newly developed ABC169 medium and demonstrate that physical contact with a male worm, and not insemination, is sufficient to induce female development and the production of viable parthenogenetic haploid embryos. By performing an RNAi screen for genes whose expression was enriched in the female reproductive organs, we identify a single nuclear hormone receptor that is required for differentiation and maturation of germ line stem cells in female gonad. Furthermore, we screen genes in non-reproductive tissues that maybe involved in mediating cell signaling during the male-female interplay and identify a transcription factor gli1 whose knockdown prevents male worms from inducing the female sexual maturation while having no effect on male:female pairing. Using RNA-seq, we characterize the gene expression changes of male worms after gli1 knockdown as well as the female transcriptomic changes after pairing with gli1-knockdown males. We are currently exploring the downstream genes of this transcription factor that may mediate the male stimulus associated with pairing. -
Neuropsychological Testing
Medical Coverage Policy Effective Date ............................................. 8/15/2021 Next Review Date ....................................... 8/15/2022 Coverage Policy Number .................................. 0258 Neuropsychological Testing Table of Contents Related Coverage Resources Overview .............................................................. 1 Attention-Deficit/Hyperactivity Disorder: Assessment Coverage Policy ................................................... 1 and Treatment General Background ............................................ 2 Autism Spectrum Disorder/Pervasive Developmental Medicare Coverage Determinations .................. 15 Disorders: Assessment and Treatment Coding/Billing Information .................................. 16 Cognitive Rehabilitation Lyme Disease Treatment— Antibiotic Treatment References ........................................................ 28 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary -

Programme Against African Trypanosomiasis Year 2006 Volume
ZFBS 1""5 1SPHSBNNF *44/ WPMVNF "HBJOTU "GSJDBO QBSU 5SZQBOPTPNJBTJT 43%43%!.$4290!./3/-)!3)3).&/2-!4)/. $EPARTMENTFOR )NTERNATIONAL $EVELOPMENT year 2006 PAAT Programme volume 29 Against African part 1 Trypanosomiasis TSETSE AND TRYPANOSOMIASIS INFORMATION Numbers 13466–13600 Edited by James Dargie Bisamberg Austria FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS Rome, 2006 The designations employed and the presentation of material in this information product do not imply the expression of any opinion whatsoever on the part of the Food and Agriculture Organization of the United Nations concerning the legal or development status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. All rights reserved. Reproduction and dissemination of material in this in- formation product for educational or other non-commercial purposes are authorized without any prior written permission from the copyright holders provided the source is fully acknowledged. Reproduction of material in this information product for resale or other commercial purposes is prohibited without written permission of the copyright holders. Applications for such permission should be addressed to the Chief, Electronic Publishing Policy and Support Branch, Information Division, FAO, Viale delle Terme di Caracalla, 00100 Rome, Italy or by e-mail to [email protected] © FAO 2006 Tsetse and Trypanosomiasis Information Volume 29 Part 1, 2006 Numbers 13466–13600 Tsetse and Trypanosomiasis Information TSETSE AND TRYPANOSOMIASIS INFORMATION The Tsetse and Trypanosomiasis Information periodical has been established to disseminate current information on all aspects of tsetse and trypanosomiasis research and control to institutions and individuals involved in the problems of African trypanosomiasis. -

Leishmaniasis in the United States: Emerging Issues in a Region of Low Endemicity
microorganisms Review Leishmaniasis in the United States: Emerging Issues in a Region of Low Endemicity John M. Curtin 1,2,* and Naomi E. Aronson 2 1 Infectious Diseases Service, Walter Reed National Military Medical Center, Bethesda, MD 20814, USA 2 Infectious Diseases Division, Uniformed Services University, Bethesda, MD 20814, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-011-301-295-6400 Abstract: Leishmaniasis, a chronic and persistent intracellular protozoal infection caused by many different species within the genus Leishmania, is an unfamiliar disease to most North American providers. Clinical presentations may include asymptomatic and symptomatic visceral leishmaniasis (so-called Kala-azar), as well as cutaneous or mucosal disease. Although cutaneous leishmaniasis (caused by Leishmania mexicana in the United States) is endemic in some southwest states, other causes for concern include reactivation of imported visceral leishmaniasis remotely in time from the initial infection, and the possible long-term complications of chronic inflammation from asymptomatic infection. Climate change, the identification of competent vectors and reservoirs, a highly mobile populace, significant population groups with proven exposure history, HIV, and widespread use of immunosuppressive medications and organ transplant all create the potential for increased frequency of leishmaniasis in the U.S. Together, these factors could contribute to leishmaniasis emerging as a health threat in the U.S., including the possibility of sustained autochthonous spread of newly introduced visceral disease. We summarize recent data examining the epidemiology and major risk factors for acquisition of cutaneous and visceral leishmaniasis, with a special focus on Citation: Curtin, J.M.; Aronson, N.E. -

Academy of Medical Sciences of Ukraine L. V. Gromashevskiy
Academy of Medical Sciences of Ukraine L. V. Gromashevskiy Institute of Epidemiology and Infektious Diseases Panasiuk Olena Leonidivna ETHIOPATHOGENETIC THERAPY OF HERPES VIRUS INFECTION WITH THE USE OF PROTEFLAZID 14.01.13 — Infektious Diseases Kyiv — 2007 TABLE OF CONTENTS LIST OF ABBREVIATIONS USED INTRODUCTION CHAPTER 1 PRESSING ISSUES OF TREATMENT OF HERPES VIRUS INFECTIONS 1.2. Main principles of treatment of patients with herpes virus infections CHAPTER 2 MATERIALS AND STUDY METHODS 2.1. Characteristic of examined patients 2.2. Characteristic of study drug and treatment methods 2.3. Study design 2.3.1. Subjects enrollment and discontinuation criteria 2.3.2. Principles and algorithm of subjects grouping 2.3.3. Assessment of therapy efficacy 2.4. Study methods 2.4.1. Clinical method 2.4.2. Special study methods 2.4.3. Statistical method CHAPTER 3 ETHIOPATHOGENETIC THERAPY OF HERPES VIRUS INFECTION WITH THE USE OF PROTEFLAZID 3.1. Clinical efficacy of Proteflazid 3.2. Adverse effects of therapy with Proteflazid 3.3. Interferon inducing and immunomodulatory activity of Proteflazid in subjects with herpes virus infection 3.3.1. Immunomodulatory activity of Proteflazid 3.3.2. Interferon inducing properties of Proteflazid CHAPTER 4 LONG-TERM RESULTS OF TREATMENT OF HERPES VIRUS INFECTION 4.1. Anti-relapse efficacy of Proteflazid CONCLUSIONS PRACTICAL GUIDELINES REFERENCES List of abbreviations used NK (CD16) — natural killer cells NSE — neurospecific enolase ME — meningoencerebritis ANAD — acyclic nucleoside antiviral drugs AB — antibody -

Primary Amoebic Meningoencephalitis Amoebic Meningoencephalitis Is Primary Ś
PØEHLEDOVÉ PRÁCE PØEHLEDOVÉ JE NEGLERIÓZA VEREJNO-ZDRAVOTNÍCKYM PROBLÉMOM? IS PRIMARY AMOEBIC MENINGOENCEPHALITIS (NAEGLERIASIS) A PUBLIC HEALTH PROBLEM? KATARÍNA TRNKOVÁ, LUCIA MAĎAROVÁ, CYRIL KLEMENT Regionálny úrad verejného zdravotníctva so sídlom v Banskej Bystrici, odbor lekárskej mikrobiológie SOUHRN Neglerióza alebo primárna amébová meningoencefalitída (PAM) je zriedkavé ochorenie CNS, pôvodcom ktorého je vo¾ne žijúca meòavka Naegleria fowleri. Medzi stovkami vo¾ne žijúcich meòaviek sú známe i ïalšie rody, ktorých zástupcovia sú schopní infikovaś èloveka a vyvolaś u neho ochorenie. Za patogény sú považovaní zástupcovia rodov Acanthamoeba a Naegleria a druhy Balamuthia mandrillaris a Sappi- nia diploidea. Infekcie spôsobené týmito organizmami vyvolávajú u ¾udí syndrómy v rozsahu od akútnych fatálnych ochorení po chronické, tkanivá napadajúce infekcie s granulomatóznymi prejavmi. Epidemiológia, imunológia, patológia a klinické prejavy týchto infekcií sa vzájomne ve¾mi líšia. Príspevok podáva preh¾ad o pôvodcovi ochorenia PAM, o jeho morfológii, životnom cykle, ekológii ako aj o patogenéze, symptomatike a spôsoboch laboratórnej diagnostiky negleriózy. K¾úèové slová: neglerióza, primárna amébová meningoencefalitída, epidemiológia, laboratórna diagnostika Naegleria fowleri SUMMARY Naegleriasis or primary amoebic meningoencephalitis (PAM) is invariably an acute, often fulminant infection of CNS caused by Naegleria fowleri, a small, free-living amoeba. Pathogenic free-living amoebae can cause serious illnesses in humans. The amoe- HYGIENA bae belonging to the genus Naegleria, Acanthamoeba and Balamuthia mandrillaris and Sappinia diploidea produce syndromes in man ranging from acute fatal disease to chronic tissue invasion with granulomatous manifestation. The purpose of this report is to describe the clinical history, treatment, pathology and methods of laboratory diagnostic of naegleriasis. Key words: primary amoebic meningoencephalitis, naegleriasis, epidemiology, laboratory diagnostics of Naegleria fowleri ÈÍSLO 2 Úvod Obr. -

SNF Mobility Model: ICD-10 HCC Crosswalk, V. 3.0.1
The mapping below corresponds to NQF #2634 and NQF #2636. HCC # ICD-10 Code ICD-10 Code Category This is a filter ceThis is a filter cellThis is a filter cell 3 A0101 Typhoid meningitis 3 A0221 Salmonella meningitis 3 A066 Amebic brain abscess 3 A170 Tuberculous meningitis 3 A171 Meningeal tuberculoma 3 A1781 Tuberculoma of brain and spinal cord 3 A1782 Tuberculous meningoencephalitis 3 A1783 Tuberculous neuritis 3 A1789 Other tuberculosis of nervous system 3 A179 Tuberculosis of nervous system, unspecified 3 A203 Plague meningitis 3 A2781 Aseptic meningitis in leptospirosis 3 A3211 Listerial meningitis 3 A3212 Listerial meningoencephalitis 3 A34 Obstetrical tetanus 3 A35 Other tetanus 3 A390 Meningococcal meningitis 3 A3981 Meningococcal encephalitis 3 A4281 Actinomycotic meningitis 3 A4282 Actinomycotic encephalitis 3 A5040 Late congenital neurosyphilis, unspecified 3 A5041 Late congenital syphilitic meningitis 3 A5042 Late congenital syphilitic encephalitis 3 A5043 Late congenital syphilitic polyneuropathy 3 A5044 Late congenital syphilitic optic nerve atrophy 3 A5045 Juvenile general paresis 3 A5049 Other late congenital neurosyphilis 3 A5141 Secondary syphilitic meningitis 3 A5210 Symptomatic neurosyphilis, unspecified 3 A5211 Tabes dorsalis 3 A5212 Other cerebrospinal syphilis 3 A5213 Late syphilitic meningitis 3 A5214 Late syphilitic encephalitis 3 A5215 Late syphilitic neuropathy 3 A5216 Charcot's arthropathy (tabetic) 3 A5217 General paresis 3 A5219 Other symptomatic neurosyphilis 3 A522 Asymptomatic neurosyphilis 3 A523 Neurosyphilis, -

An Epidemic of Acute Encephalitis in Young Children
Arch Dis Child: first published as 10.1136/adc.9.51.153 on 1 June 1934. Downloaded from AN EPIDEMIC OF ACUTE ENCEPHALITIS IN YOUNG CHILDREN BY AGNES R. MACGREGOR, M.B., F.R.C.P.E., AND W. S. CRAIG, B.Sc., M.D., M.R.C.P.E. (From the Departments of Pathology and Child Life and Health, Univer- sity of Edinburgh, and the Western General Hospital, Edinburgh.) This paper is concerned with a small outbreak of illness of an unusual nature occurring in the Children's Unit of the Western General Hospital, Edinburgh. In addition to the clinical interest of the cases, there are features of considerable pathological and epidemiological importance con- nected with the outbreak. Clinical Records. Case 1. I.M.S., female, aged 1 year 7 months, was admitted to the Western General Hospital in March, 1933, at the age of 1 year 3 months. - At this time http://adc.bmj.com/ she was noted as being slightly undersized but well nourished and the liver showed moderate enlargement. Prior to admission she had been treated elsewhere for gonococcal vaginitis: during the three succeeding months her health was good and progress uninterrupted, but a positive Wassermann reaction, present on admission, persisted. On the evening of July 22, 1933, the patient was noticed to be less active than usual and generally ' out of sorts ': her conditiQn remained unchanged throughout the rest of the day, and on the 23rd she was 'Ptill quieter and less responsive to all forms of attention and refused food. By the afternoon on October 2, 2021 by guest. -

Ghanaian Mangrove Wetland Endophytic Fungus, Penicillium Herquei Strain BRS2A-AR Produces
Available online at http://www.ifgdg.org Int. J. Biol. Chem. Sci. 13(4): 1918-1937, August 2019 ISSN 1997-342X (Online), ISSN 1991-8631 (Print) Original Paper http://ajol.info/index.php/ijbcs http://indexmedicus.afro.who.int Ghanaian Mangrove Wetland Endophytic Fungus, Penicillium herquei strain BRS2A-AR produces (9Z, 11E)-13-oxooctadeca-9,11-dienoic acid with activity against Trichomonas mobilensis Kennedy HAYIBOR1, Samuel KWAIN1, Enoch OSEI1, Adwoa Padiki NARTEY1, Gilbert Mawuli TETEVI1, Kofi Baffour-Awuah OWUSU2, Mustafa CAMAS3, Anil Sazak CAMAS3 and Kwaku KYEREMEH1* 1 Marine and Plant Research Laboratory of Ghana, Department of Chemistry, School of Physical and Mathematical Sciences, University of Ghana, P.O. Box LG 56, Legon-Accra, Ghana. 2 Department of Parasitology, Noguchi Memorial Institute for Medical Research, University of Ghana, P.O. Box LG 581, Legon-Accra, Ghana. 3 Department of Bioengineering, Munzur University, 62000 Tunceli, Turkey. *Corresponding author; E-mail: [email protected]; Tel.: +233-50-482-9778 ABSTRACT Sub-Sahara Africa is burdened with a high incidence of parasitic infections, including schistosomiasis, trypanosomiasis, trichomoniasis, and leishmaniasis. Currently, there is a rapid widespread development of resistance to prescription drugs for these neglected diseases. Microbes provide the largest chemical and biological diversity in drug discovery screening programs; therefore, our project seeks to explore microbes in the sub-region for new drugs. The oxylipin (9Z,11E)-13-oxooctadeca-9,11-dienoic acid (1) was isolated from the Ghanaian endophytic fungus, Penicillium herquei strain BRS2A-AR obtained from the leaves of a Laguncularia racemosa tree growing on the banks of the River Butre in the Western Regional wetlands of Ghana.